Tuesday Poster Session
Category: Esophagus
P4933 - The Prevalence of Barrett’s Esophagus and Esophageal Adenocarcinoma After Laparoscopic Sleeve Gastrectomy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Alexandra Kimchy, DO
MedStar Georgetown University Hospital
Washington, DC
Presenting Author(s)
Alexandra Kimchy, DO1, Summer McCloud, BS2, Ayah Arafat, BS3, Thomas Loughney, MD1
1MedStar Georgetown University Hospital, Washington, DC; 2Georgetown University School of Medicine, Washington, DC; 3MedStar Health Research Institute, Hyattsville, MD
Introduction: Laparoscopic sleeve gastrectomy (LSG) has become the most popular bariatric procedure performed worldwide. With the rise in patients undergoing LSG, gastroesophageal reflux disease (GERD) has emerged as a concerning side effect of this operation. Chronic GERD is a well-established risk factor for the development of Barrett’s esophagus (BE), a pre-malignant condition for esophageal adenocarcinoma (EAC). There have been few studies investigating the risk of BE after LSG. The aim of this study was to determine the prevalence of BE and EAC in patients who have undergone LSG.
Methods: We conducted a retrospective, observational study of patients who underwent LSG at four hospitals within a regional health network from 2014 to 2023. Patients included were those who had an esophagogastroduodenoscopy (EGD) with biopsy prior to and at least 6 months after LSG. ICD 9/10 PCS codes were used to identify patients with LSG and CPT code for EGD with biopsy. EGD and pathology reports were reviewed to confirm the diagnosis of BE and/or EAC. Clinical risk factors were evaluated in patients with and without BE. Statistical analyses were performed in R version 4.4.2.
Results: Of the 422 LSG patients who had an EGD with biopsy after surgery, 5 patients (1.2%) were found to have BE that was not found on the pre-operative (pre-op) EGD, and there were no patients with EAC. Gender, race, tobacco use, GERD, hiatal hernia, proton pump inhibitor use, esophagitis and H. pylori did not significantly differ between the two groups. Patients with BE were significantly older than patients without BE at the time of the pre-op and post-operative (post-op) EGD (55 vs 43, p=0.002; 59 vs. 47, p=0.004). The BE group had a lower mean body mass index (BMI) and higher percentage of total body weight loss (TBWL) at post-op EGD than the cohort without BE (29 vs. 38, p=0.016; 37 vs. 20; p=0.039). There was an association between older age and greater TBWL at post-op EGD with BE (OR 1.18, p=0.006; OR 1.08, p=0.003). Patients with a higher BMI post-op had a lower odds of BE (OR 0.84; p=0.029).
Discussion: The prevalence of BE among patients with LSG was found to be no greater than rates observed in the general population, approximately 1-2%. Therefore, having a history of LSG may not be sufficient to recommend screening for BE after surgery. Future longitudinal studies evaluating disease risk in this patient population over multiple decades are needed for further confirmation of these results.
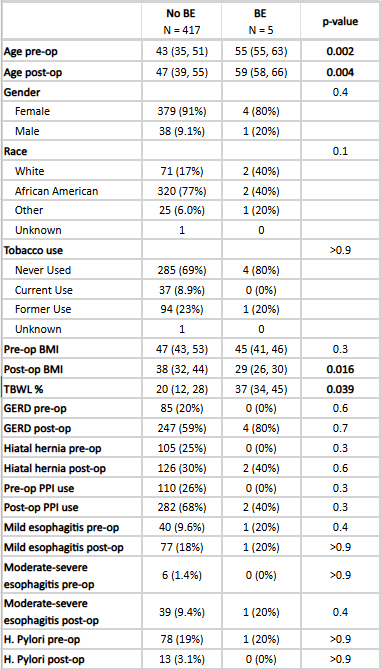
Figure: Table 1. Comparison of clinical risk factors in patients with and without Barrett's esophagus
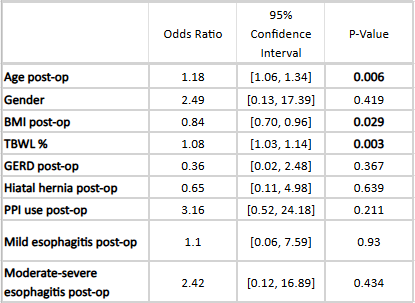
Figure: Table 2. Univariate logistic regression of risk factors for Barrett's esophagus
Disclosures:
Alexandra Kimchy indicated no relevant financial relationships.
Summer McCloud indicated no relevant financial relationships.
Ayah Arafat indicated no relevant financial relationships.
Thomas Loughney indicated no relevant financial relationships.
Alexandra Kimchy, DO1, Summer McCloud, BS2, Ayah Arafat, BS3, Thomas Loughney, MD1. P4933 - The Prevalence of Barrett’s Esophagus and Esophageal Adenocarcinoma After Laparoscopic Sleeve Gastrectomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1MedStar Georgetown University Hospital, Washington, DC; 2Georgetown University School of Medicine, Washington, DC; 3MedStar Health Research Institute, Hyattsville, MD
Introduction: Laparoscopic sleeve gastrectomy (LSG) has become the most popular bariatric procedure performed worldwide. With the rise in patients undergoing LSG, gastroesophageal reflux disease (GERD) has emerged as a concerning side effect of this operation. Chronic GERD is a well-established risk factor for the development of Barrett’s esophagus (BE), a pre-malignant condition for esophageal adenocarcinoma (EAC). There have been few studies investigating the risk of BE after LSG. The aim of this study was to determine the prevalence of BE and EAC in patients who have undergone LSG.
Methods: We conducted a retrospective, observational study of patients who underwent LSG at four hospitals within a regional health network from 2014 to 2023. Patients included were those who had an esophagogastroduodenoscopy (EGD) with biopsy prior to and at least 6 months after LSG. ICD 9/10 PCS codes were used to identify patients with LSG and CPT code for EGD with biopsy. EGD and pathology reports were reviewed to confirm the diagnosis of BE and/or EAC. Clinical risk factors were evaluated in patients with and without BE. Statistical analyses were performed in R version 4.4.2.
Results: Of the 422 LSG patients who had an EGD with biopsy after surgery, 5 patients (1.2%) were found to have BE that was not found on the pre-operative (pre-op) EGD, and there were no patients with EAC. Gender, race, tobacco use, GERD, hiatal hernia, proton pump inhibitor use, esophagitis and H. pylori did not significantly differ between the two groups. Patients with BE were significantly older than patients without BE at the time of the pre-op and post-operative (post-op) EGD (55 vs 43, p=0.002; 59 vs. 47, p=0.004). The BE group had a lower mean body mass index (BMI) and higher percentage of total body weight loss (TBWL) at post-op EGD than the cohort without BE (29 vs. 38, p=0.016; 37 vs. 20; p=0.039). There was an association between older age and greater TBWL at post-op EGD with BE (OR 1.18, p=0.006; OR 1.08, p=0.003). Patients with a higher BMI post-op had a lower odds of BE (OR 0.84; p=0.029).
Discussion: The prevalence of BE among patients with LSG was found to be no greater than rates observed in the general population, approximately 1-2%. Therefore, having a history of LSG may not be sufficient to recommend screening for BE after surgery. Future longitudinal studies evaluating disease risk in this patient population over multiple decades are needed for further confirmation of these results.
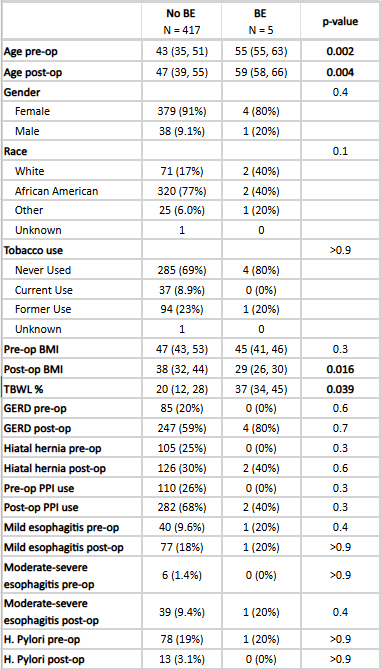
Figure: Table 1. Comparison of clinical risk factors in patients with and without Barrett's esophagus
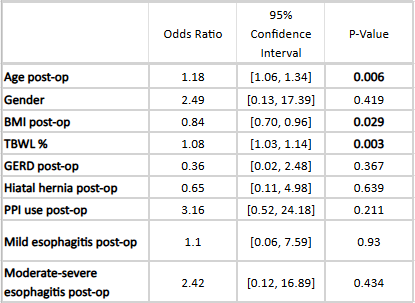
Figure: Table 2. Univariate logistic regression of risk factors for Barrett's esophagus
Disclosures:
Alexandra Kimchy indicated no relevant financial relationships.
Summer McCloud indicated no relevant financial relationships.
Ayah Arafat indicated no relevant financial relationships.
Thomas Loughney indicated no relevant financial relationships.
Alexandra Kimchy, DO1, Summer McCloud, BS2, Ayah Arafat, BS3, Thomas Loughney, MD1. P4933 - The Prevalence of Barrett’s Esophagus and Esophageal Adenocarcinoma After Laparoscopic Sleeve Gastrectomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
