Monday Poster Session
Category: Liver
P3924 - Acute Liver Failure in a Patient With Alcohol Use Disorder; Surprising Turn of Events
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Yazan Omari, MD (he/him/his)
Ascension Providence Hospital
Southfield, MI
Presenting Author(s)
Award: ACG Presidential Poster Award
Yazan Omari, MD1, Saif Affas, MD1, Dima Sallam, MD2, Brian Nohomovich, DO, PhD1
1Ascension Providence Hospital, Southfield, MI; 2Henry Ford Providence Hospital, Southfield, MI
Introduction: Acute liver failure (ALF) is a life-threatening condition characterized by rapid liver dysfunction, often requiring urgent medical intervention. One rare but significant cause of ALF is portal vein thrombosis (PVT), especially in patients with risk factors.This case highlights a 48-year-old female with AMS and severe liver dysfunction due to PVT.
Case Description/
Methods: A 48-year-old woman with chronic alcohol abuse was found unconscious at home surrounded by empty liquor bottles. On presentation to the emergency department, she exhibited altered mental status (GCS of 10), jaundice, abdominal swelling, and progressive yellowing of her eyes over the prior day. she was hemodynamically unstable, requiring vasopressor support in the ICU. Laboratory tests showed severe anemia, necessitating 2 units of packed red blood cells, a total bilirubin of 12 mg/dL, AST of 746 U/L, ALT of 115 U/L, INR of 3.2, ammonia of 142 µmol/L, and lactate of 12.1 mmol/L. The Maddrey’s Discriminant Function was 132, and MELD-Na score was 29. Imaging studies included CT of the abdomen and pelvis, revealing PVT with filling defects in the main portal vein, while the right and left portal veins were patent. Ultrasound confirmed mild fluid collections and PVT. The patient was treated in the ICU for 3 days before being transferred to a tertiary care center for liver transplant evaluation.
Discussion: PVT is a rare cause of ALF, and its rarity makes it challenging to diagnose. The obstruction of portal vein flow leads to increased portal pressure, reduced hepatic perfusion, and ischemia. This ischemia causes hepatocyte necrosis and inflammation, which exacerbates liver dysfunction and can lead to coagulopathy, encephalopathy, and metabolic disturbances.
In this case, the patient’s alcohol abuse and acute decompensation raised suspicion for PVT, though it remains a rare etiology. Symptoms of PVT often overlap with other causes of ALF, which complicates diagnosis. Timely imaging with Doppler ultrasound and contrast-enhanced CT is essential to confirm PVT, evaluate the extent of thrombosis, and rule out other pathologies.
Given the severe coagulopathy in PVT, anticoagulation is generally contraindicated due to the high risk of bleeding. The management is largely supportive, focusing on hemodynamic stabilization, infection prevention, and ammonia-lowering therapies Liver transplantation is the definitive treatment for those with progressive liver failure, and early referral to a transplant center is crucial for improving outcomes.
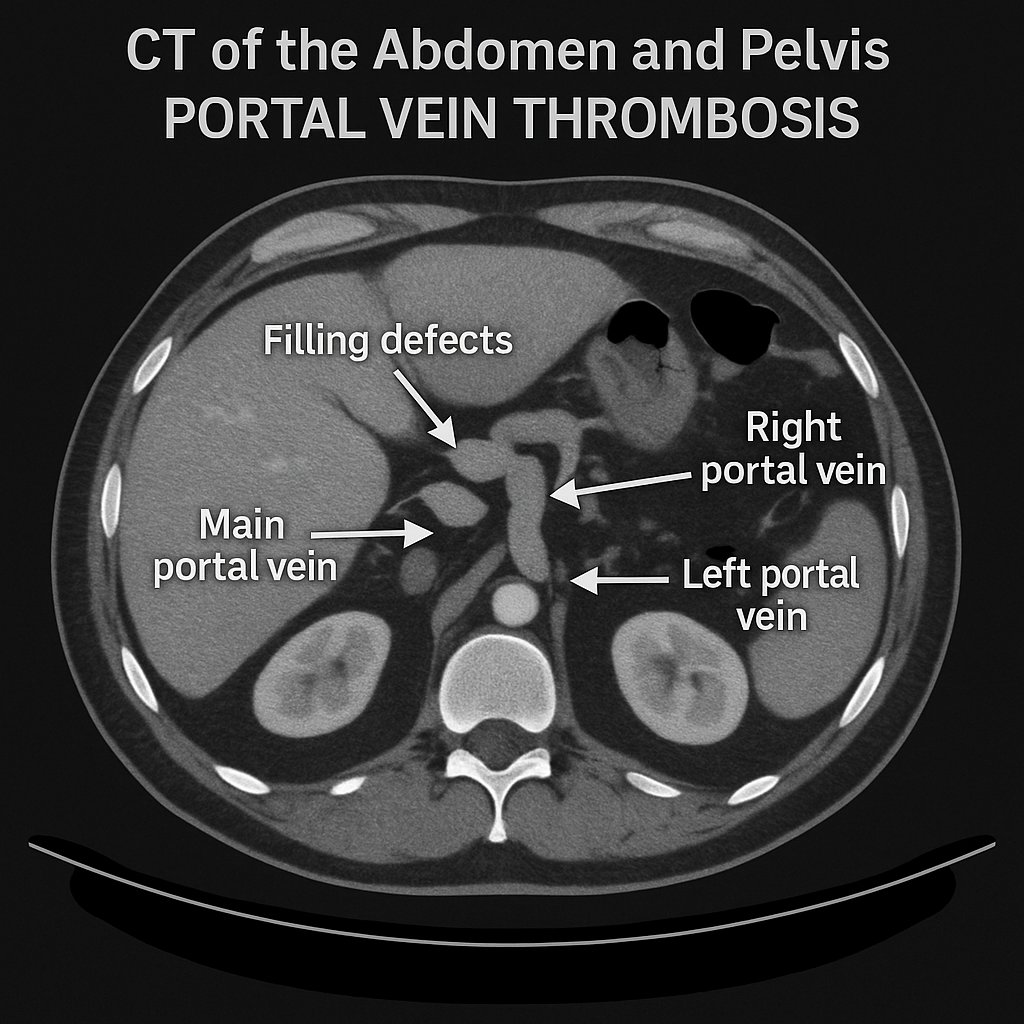
Figure: Fig!1: Illustration of portal vein thrombosis (PVT) on Computed Tomography with emphasis on filling defects (arrow)
Disclosures:
Yazan Omari indicated no relevant financial relationships.
Saif Affas indicated no relevant financial relationships.
Dima Sallam indicated no relevant financial relationships.
Brian Nohomovich indicated no relevant financial relationships.
Yazan Omari, MD1, Saif Affas, MD1, Dima Sallam, MD2, Brian Nohomovich, DO, PhD1. P3924 - Acute Liver Failure in a Patient With Alcohol Use Disorder; Surprising Turn of Events, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Yazan Omari, MD1, Saif Affas, MD1, Dima Sallam, MD2, Brian Nohomovich, DO, PhD1
1Ascension Providence Hospital, Southfield, MI; 2Henry Ford Providence Hospital, Southfield, MI
Introduction: Acute liver failure (ALF) is a life-threatening condition characterized by rapid liver dysfunction, often requiring urgent medical intervention. One rare but significant cause of ALF is portal vein thrombosis (PVT), especially in patients with risk factors.This case highlights a 48-year-old female with AMS and severe liver dysfunction due to PVT.
Case Description/
Methods: A 48-year-old woman with chronic alcohol abuse was found unconscious at home surrounded by empty liquor bottles. On presentation to the emergency department, she exhibited altered mental status (GCS of 10), jaundice, abdominal swelling, and progressive yellowing of her eyes over the prior day. she was hemodynamically unstable, requiring vasopressor support in the ICU. Laboratory tests showed severe anemia, necessitating 2 units of packed red blood cells, a total bilirubin of 12 mg/dL, AST of 746 U/L, ALT of 115 U/L, INR of 3.2, ammonia of 142 µmol/L, and lactate of 12.1 mmol/L. The Maddrey’s Discriminant Function was 132, and MELD-Na score was 29. Imaging studies included CT of the abdomen and pelvis, revealing PVT with filling defects in the main portal vein, while the right and left portal veins were patent. Ultrasound confirmed mild fluid collections and PVT. The patient was treated in the ICU for 3 days before being transferred to a tertiary care center for liver transplant evaluation.
Discussion: PVT is a rare cause of ALF, and its rarity makes it challenging to diagnose. The obstruction of portal vein flow leads to increased portal pressure, reduced hepatic perfusion, and ischemia. This ischemia causes hepatocyte necrosis and inflammation, which exacerbates liver dysfunction and can lead to coagulopathy, encephalopathy, and metabolic disturbances.
In this case, the patient’s alcohol abuse and acute decompensation raised suspicion for PVT, though it remains a rare etiology. Symptoms of PVT often overlap with other causes of ALF, which complicates diagnosis. Timely imaging with Doppler ultrasound and contrast-enhanced CT is essential to confirm PVT, evaluate the extent of thrombosis, and rule out other pathologies.
Given the severe coagulopathy in PVT, anticoagulation is generally contraindicated due to the high risk of bleeding. The management is largely supportive, focusing on hemodynamic stabilization, infection prevention, and ammonia-lowering therapies Liver transplantation is the definitive treatment for those with progressive liver failure, and early referral to a transplant center is crucial for improving outcomes.
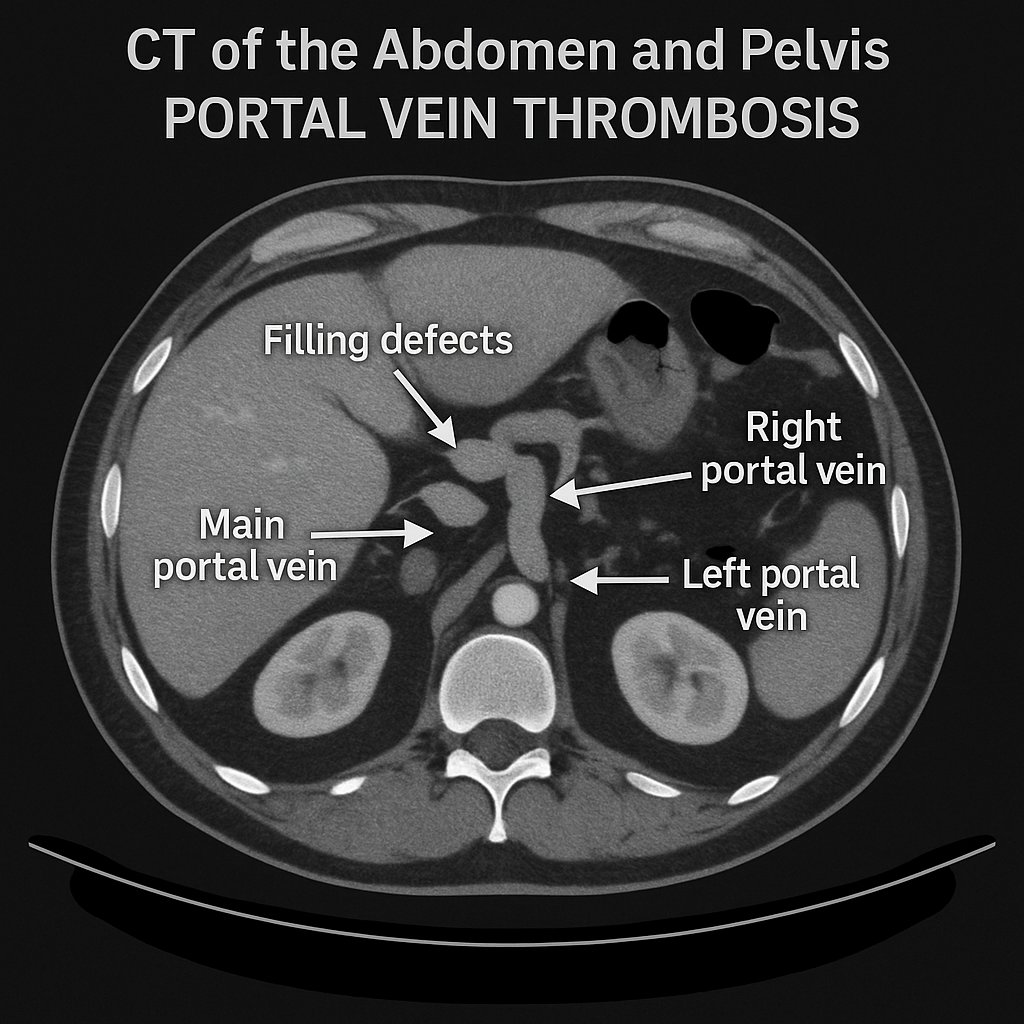
Figure: Fig!1: Illustration of portal vein thrombosis (PVT) on Computed Tomography with emphasis on filling defects (arrow)
Disclosures:
Yazan Omari indicated no relevant financial relationships.
Saif Affas indicated no relevant financial relationships.
Dima Sallam indicated no relevant financial relationships.
Brian Nohomovich indicated no relevant financial relationships.
Yazan Omari, MD1, Saif Affas, MD1, Dima Sallam, MD2, Brian Nohomovich, DO, PhD1. P3924 - Acute Liver Failure in a Patient With Alcohol Use Disorder; Surprising Turn of Events, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

