Monday Poster Session
Category: Esophagus
P2879 - Esophageal Parakeratosis in a Patient With Reflux Improved With Zinc Replacement
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- PM
Padmavathi Mali, MD (she/her/hers)
Gundersen Health
Onalaska, WI
Presenting Author(s)
Padmavathi Mali, MD
Gundersen Health, Onalaska, WI
Introduction: Esophageal parakeratosis is a rare histological finding characterized by incomplete keratinization of the squamous epithelium. While not considered a direct precursor to malignancy, it may occur alongside conditions that elevate cancer risk. Animal studies have demonstrated a potential link between zinc deficiency and esophageal keratinization. We present a unique case of esophageal parakeratosis in a patient with confirmed zinc deficiency that resolved following zinc supplementation.
Case Description/
Methods: A 59-year-old woman underwent EGD as part of a workup for esophageal thickening seen on a CT scan, performed due to concern for malignancy in the setting of hypercalcemia (serum calcium: 12.3 mg/dL) and a history of smoking. EGD showed an irregular Z-line and mild mucosal changes in the lower third of the esophagus, including congestion and sloughing. Biopsies showed squamous mucosa with parakeratosis, acanthosis, and mild reactive epithelial changes.
Laboratory workup revealed a low zinc level of 58.4 mcg/dL (normal: 60–120). Zinc supplementation was initiated, and levels improved to 70 mcg/dL. A repeat EGD a year later demonstrated mild mucosal changes at the gastroesophageal junction with altered texture and resolution of sloughing. Biopsies showed only reactive squamous mucosa consistent with reflux, with no evidence of parakeratosis or intestinal metaplasia. Additional lab findings included vitamin D deficiency (16.2 ng/mL; normal: 31–100), which was also treated.
Discussion: This case illustrates a rare presentation of esophageal parakeratosis in association with zinc deficiency and reflux disease. Although esophageal parakeratosis is often an incidental histologic finding, its association with zinc deficiency warrants consideration. Zinc plays a critical role in cellular proliferation and epithelial repair, and its deficiency may contribute to abnormal keratinization. Resolution of parakeratosis following zinc supplementation supports a potential causal relationship. While the malignant potential of parakeratosis remains uncertain, this case adds to the growing body of evidence suggesting that micronutrient deficiencies may contribute to esophageal mucosal changes. Further research is needed to clarify its clinical implications and whether patients with esophageal parakeratosis should undergo surveillance for dysplasia.
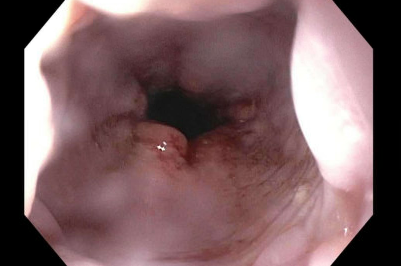
Figure: Initial EGD: Sloughing of the mucosa observed in the distal third of the esophagus

Figure: Subsequent EGD: Demonstrated improvement in mucosal sloughing, with mildly altered mucosal texture
Disclosures:
Padmavathi Mali indicated no relevant financial relationships.
Padmavathi Mali, MD. P2879 - Esophageal Parakeratosis in a Patient With Reflux Improved With Zinc Replacement, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Gundersen Health, Onalaska, WI
Introduction: Esophageal parakeratosis is a rare histological finding characterized by incomplete keratinization of the squamous epithelium. While not considered a direct precursor to malignancy, it may occur alongside conditions that elevate cancer risk. Animal studies have demonstrated a potential link between zinc deficiency and esophageal keratinization. We present a unique case of esophageal parakeratosis in a patient with confirmed zinc deficiency that resolved following zinc supplementation.
Case Description/
Methods: A 59-year-old woman underwent EGD as part of a workup for esophageal thickening seen on a CT scan, performed due to concern for malignancy in the setting of hypercalcemia (serum calcium: 12.3 mg/dL) and a history of smoking. EGD showed an irregular Z-line and mild mucosal changes in the lower third of the esophagus, including congestion and sloughing. Biopsies showed squamous mucosa with parakeratosis, acanthosis, and mild reactive epithelial changes.
Laboratory workup revealed a low zinc level of 58.4 mcg/dL (normal: 60–120). Zinc supplementation was initiated, and levels improved to 70 mcg/dL. A repeat EGD a year later demonstrated mild mucosal changes at the gastroesophageal junction with altered texture and resolution of sloughing. Biopsies showed only reactive squamous mucosa consistent with reflux, with no evidence of parakeratosis or intestinal metaplasia. Additional lab findings included vitamin D deficiency (16.2 ng/mL; normal: 31–100), which was also treated.
Discussion: This case illustrates a rare presentation of esophageal parakeratosis in association with zinc deficiency and reflux disease. Although esophageal parakeratosis is often an incidental histologic finding, its association with zinc deficiency warrants consideration. Zinc plays a critical role in cellular proliferation and epithelial repair, and its deficiency may contribute to abnormal keratinization. Resolution of parakeratosis following zinc supplementation supports a potential causal relationship. While the malignant potential of parakeratosis remains uncertain, this case adds to the growing body of evidence suggesting that micronutrient deficiencies may contribute to esophageal mucosal changes. Further research is needed to clarify its clinical implications and whether patients with esophageal parakeratosis should undergo surveillance for dysplasia.
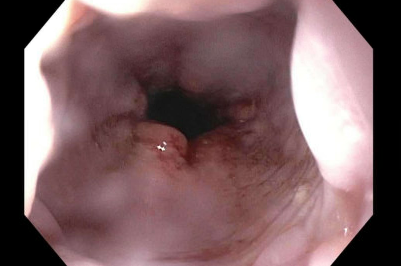
Figure: Initial EGD: Sloughing of the mucosa observed in the distal third of the esophagus

Figure: Subsequent EGD: Demonstrated improvement in mucosal sloughing, with mildly altered mucosal texture
Disclosures:
Padmavathi Mali indicated no relevant financial relationships.
Padmavathi Mali, MD. P2879 - Esophageal Parakeratosis in a Patient With Reflux Improved With Zinc Replacement, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
