Monday Poster Session
Category: Interventional Endoscopy
P3614 - Duodenal Perforation From Dislodged Prophylactic Pancreatic Stent Following ERCP for Hilar Cholangiocarcinoma: A Rare Adverse Event
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mina Fransawy Alkomos, MD
St. Joseph's University Medical Center
Paterson, NJ
Presenting Author(s)
Mina Fransawy Alkomos, MD1, Patrick Tempera, DO1, Beshoy Effat Elkomos, MD2, Walid Baddoura, MD1, Youssef Botros, MD1
1St. Joseph's University Medical Center, Paterson, NJ; 2General and colorectal surgery department, Royal United Hospital, Bath, UK, Path, England, United Kingdom
Introduction: ERCP is central in the diagnostic and therapeutic approach to cholangiocarcinoma. Prophylactic pancreatic stenting is a routine measure to reduce post-ERCP pancreatitis, especially after inadvertent duct cannulation. While generally safe, stent migration and perforation are exceedingly rare complications. We describe a case of duodenal perforation following dislodgement of a prophylactic pancreatic duct stent in a patient undergoing ERCP for hilar cholangiocarcinoma evaluation.
Case Description/
Methods: A 47-year-old woman presented with two weeks of painless jaundice. Labs revealed total bilirubin of 18 mg/dL and elevated alkaline phosphatase and GGT. CT showed intrahepatic ductal dilation without CBD enlargement. ERCP with SpyGlass cholangioscopy identified a dominant right hepatic duct stricture; targeted biopsies were obtained. A covered metal biliary stent (10 mm × 4 cm) and a right hepatic plastic stent (7 Fr × 12 cm) were placed. Due to inadvertent dorsal pancreatic duct cannulation, a prophylactic 4 Fr × 5 cm plastic stent was placed.
Two days post-ERCP, the patient developed abdominal pain. CT demonstrated free air and migration of the pancreatic stent into the peritoneum (Figure 1). Repeat ERCP confirmed duodenal perforation from the stent tip. The stent was removed, and the defect was closed endoscopically (Figure 2). The metal CBD stent was exchanged for a plastic stent to allow closer follow-up. Biopsies confirmed moderately differentiated perihilar cholangiocarcinoma. The patient recovered and proceeded with further oncologic care.
Discussion: While prophylactic pancreatic stenting is considered standard for preventing post-ERCP pancreatitis, complications such as stent migration and perforation are rare but serious. Most cases involve longer or rigid stents; however, even small-caliber stents may dislodge unpredictably. This case underscores that even technically successful ERCPs can carry delayed risks. Clinicians should remain vigilant for post-procedural symptoms suggestive of complications and consider early imaging in symptomatic patients. Prompt recognition and endoscopic management can minimize morbidity. Literature remains limited, but growing reports call for individualized risk-benefit assessments when placing prophylactic pancreatic stents.
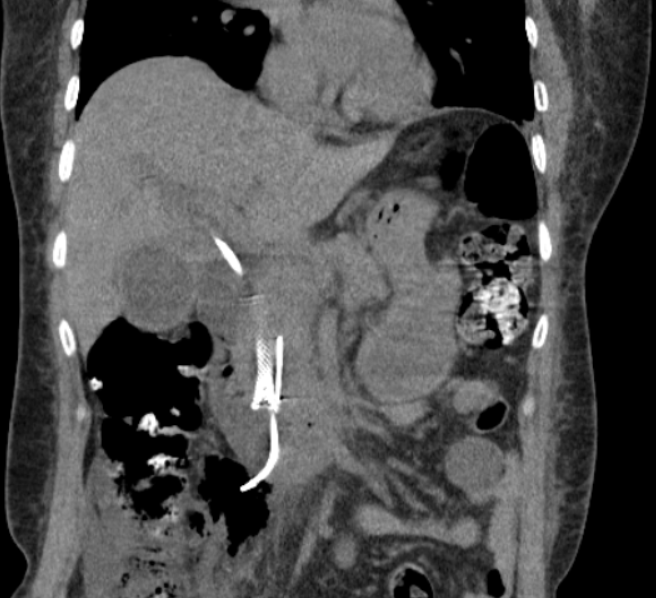
Figure: Figure 1: Plastic stent perforation into the peritoneum.
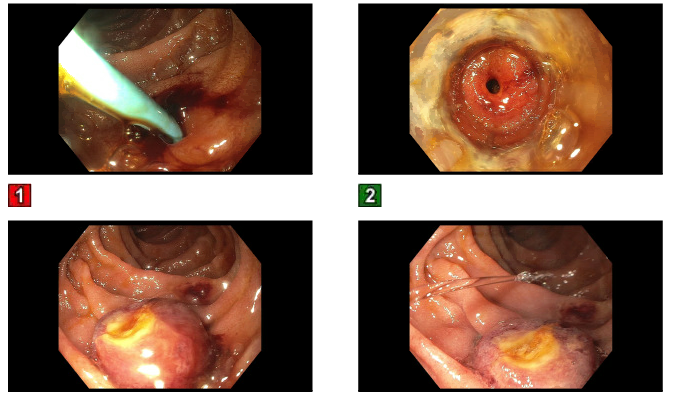
Figure: Figure 2: ERCP view of the stent causing perforation and Ovesco closure.
Disclosures:
Mina Fransawy Alkomos indicated no relevant financial relationships.
Patrick Tempera indicated no relevant financial relationships.
Beshoy Effat Elkomos indicated no relevant financial relationships.
Walid Baddoura indicated no relevant financial relationships.
Youssef Botros indicated no relevant financial relationships.
Mina Fransawy Alkomos, MD1, Patrick Tempera, DO1, Beshoy Effat Elkomos, MD2, Walid Baddoura, MD1, Youssef Botros, MD1. P3614 - Duodenal Perforation From Dislodged Prophylactic Pancreatic Stent Following ERCP for Hilar Cholangiocarcinoma: A Rare Adverse Event, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. Joseph's University Medical Center, Paterson, NJ; 2General and colorectal surgery department, Royal United Hospital, Bath, UK, Path, England, United Kingdom
Introduction: ERCP is central in the diagnostic and therapeutic approach to cholangiocarcinoma. Prophylactic pancreatic stenting is a routine measure to reduce post-ERCP pancreatitis, especially after inadvertent duct cannulation. While generally safe, stent migration and perforation are exceedingly rare complications. We describe a case of duodenal perforation following dislodgement of a prophylactic pancreatic duct stent in a patient undergoing ERCP for hilar cholangiocarcinoma evaluation.
Case Description/
Methods: A 47-year-old woman presented with two weeks of painless jaundice. Labs revealed total bilirubin of 18 mg/dL and elevated alkaline phosphatase and GGT. CT showed intrahepatic ductal dilation without CBD enlargement. ERCP with SpyGlass cholangioscopy identified a dominant right hepatic duct stricture; targeted biopsies were obtained. A covered metal biliary stent (10 mm × 4 cm) and a right hepatic plastic stent (7 Fr × 12 cm) were placed. Due to inadvertent dorsal pancreatic duct cannulation, a prophylactic 4 Fr × 5 cm plastic stent was placed.
Two days post-ERCP, the patient developed abdominal pain. CT demonstrated free air and migration of the pancreatic stent into the peritoneum (Figure 1). Repeat ERCP confirmed duodenal perforation from the stent tip. The stent was removed, and the defect was closed endoscopically (Figure 2). The metal CBD stent was exchanged for a plastic stent to allow closer follow-up. Biopsies confirmed moderately differentiated perihilar cholangiocarcinoma. The patient recovered and proceeded with further oncologic care.
Discussion: While prophylactic pancreatic stenting is considered standard for preventing post-ERCP pancreatitis, complications such as stent migration and perforation are rare but serious. Most cases involve longer or rigid stents; however, even small-caliber stents may dislodge unpredictably. This case underscores that even technically successful ERCPs can carry delayed risks. Clinicians should remain vigilant for post-procedural symptoms suggestive of complications and consider early imaging in symptomatic patients. Prompt recognition and endoscopic management can minimize morbidity. Literature remains limited, but growing reports call for individualized risk-benefit assessments when placing prophylactic pancreatic stents.
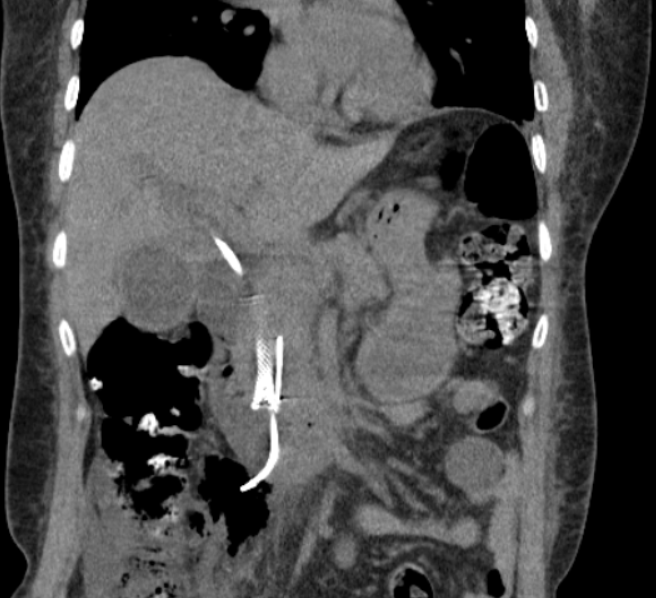
Figure: Figure 1: Plastic stent perforation into the peritoneum.
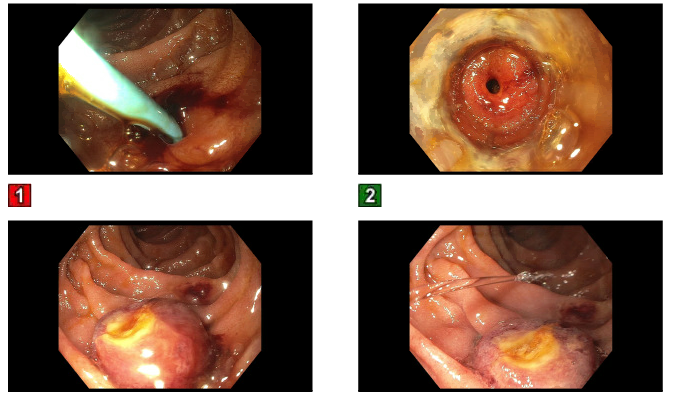
Figure: Figure 2: ERCP view of the stent causing perforation and Ovesco closure.
Disclosures:
Mina Fransawy Alkomos indicated no relevant financial relationships.
Patrick Tempera indicated no relevant financial relationships.
Beshoy Effat Elkomos indicated no relevant financial relationships.
Walid Baddoura indicated no relevant financial relationships.
Youssef Botros indicated no relevant financial relationships.
Mina Fransawy Alkomos, MD1, Patrick Tempera, DO1, Beshoy Effat Elkomos, MD2, Walid Baddoura, MD1, Youssef Botros, MD1. P3614 - Duodenal Perforation From Dislodged Prophylactic Pancreatic Stent Following ERCP for Hilar Cholangiocarcinoma: A Rare Adverse Event, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
