Tuesday Poster Session
Category: IBD
P5471 - The Impact of Concomitant Hypothyroid Disease and Inflammatory Bowel Disease in Older Adults: Underrecognized and Underappreciated
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Jahnavi Udaikumar, MD (she/her/hers)
NYU Langone Health
Brooklyn, NY
Presenting Author(s)
Jahnavi Udaikumar, MD1, Maaz Ahsan, MD2, Olivia Delau, MS2, Simon J. Hong, MD2, Seymour Katz, MD, MACG2, Jordan Axelrad, MD, MPH3, Adam Faye, MD, MS2
1NYU Langone Health, Brooklyn, NY; 2NYU Langone Health, New York, NY; 3Division of Gastroenterology, Department of Medicine, NYU Grossman School of Medicine, New York, NY
Introduction: Inflammatory bowel disease (IBD) is a chronic immune-mediated disorder often complicated by extraintestinal manifestations (EIMs). Hypothyroidism (HT), particularly autoimmune thyroiditis, shares overlapping immunopathogenic pathways with IBD, including dysregulated T-cell activation and cytokine signaling. Although HT is linked to systemic autoimmune diseases, its impact on IBD outcomes in older adults remains unclear. We aimed to evaluate factors associated with HT in older adults with IBD and its effect on laboratory and healthcare utilization outcomes.
Methods: We conducted a retrospective study at a large academic center among adults aged ≥60 years with IBD and ≥1 thyroid-stimulating hormone (TSH) measurement prior to January 1, 2022. Patients were stratified by HT status. Demographics, clinical characteristics, medication history, labs, and healthcare utilization were collected. Associations were assessed using Chi-Squared, Fisher’s Exact, or Wilcoxon Rank-Sum tests. Multivariable logistic regression evaluated factors associated with HT, while logistic and negative binomial regression assessed HT as a predictor of anemia and healthcare utilization (2016–2022).
Results: Among 158 older adults with IBD (median age 75.4 years, 63.3% female), 119 (75.3%) had HT. Demographics, smoking status, BMI, and IBD subtype were similar by HT status (Table 1). Extraintestinal manifestations (21.0% vs 18.0%, p=0.68) and prior intestinal surgery (15.1% vs 7.7%, p=0.29) were comparable. Prior biologic therapy was more common in the HT group (30.3% vs 12.8%, p=0.03) and remained independently associated after covariate adjustment (adjOR 2.93, 95% CI: 1.05–8.20, p=0.04). Among 86 older patients followed longitudinally, HT was associated with higher anemia rates (65.2% vs 35.0%, p=0.02) and remained an independent predictor on multivariate analysis (adjOR 5.31, 95% CI: 1.52-18.58; Table 2). HT was not a significant predictor of increased healthcare utilization—including colonoscopies (adjIRR 0.91, 95% CI: 0.45–1.81), hospitalizations (adjIRR 0.94, 95% CI: 0.36–2.45), emergency department (ED) visits (adjIRR 1.67, 95% CI: 0.61–4.59), or imaging (adjIRR 1.13, 95% CI: 0.58–2.24).
Discussion: In older adults with IBD, HT was independently associated with prior biologic therapy and increased anemia burden but not greater healthcare utilization. HT may represent a marker of heightened systemic inflammation, warranting early recognition and multidisciplinary management.
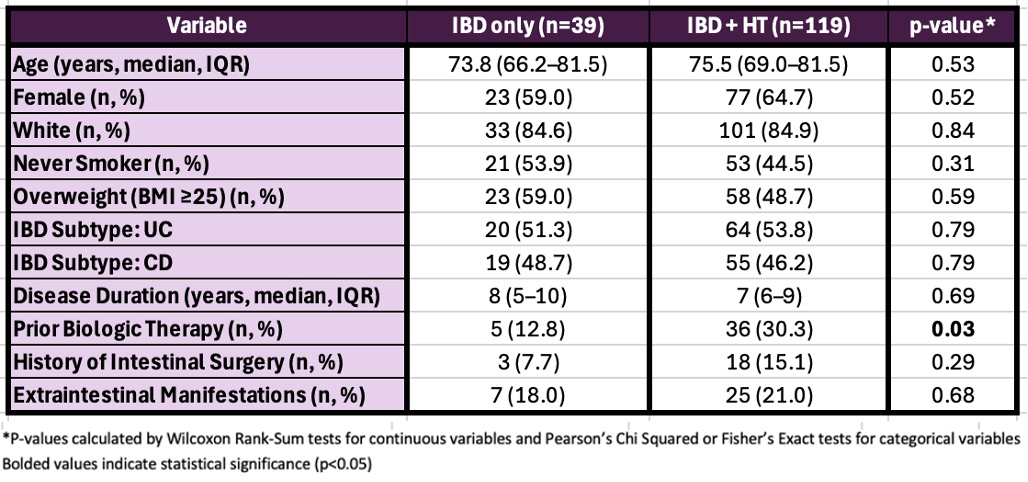
Figure: Table 1: Baseline Characteristics in Older Adults with IBD by HT Status (N = 158)
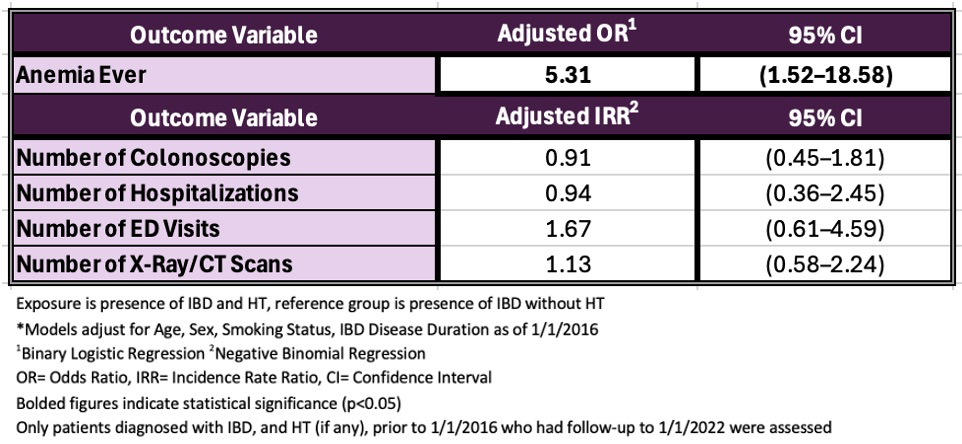
Figure: Table 2: IBD and HT as a Predictor of Anemia and Healthcare Utilization Outcomes 2016-2022 (N = 86)
Disclosures:
Jahnavi Udaikumar indicated no relevant financial relationships.
Maaz Ahsan indicated no relevant financial relationships.
Olivia Delau indicated no relevant financial relationships.
Simon Hong: Abbvie – Advisory Committee/Board Member.
Seymour Katz indicated no relevant financial relationships.
Jordan Axelrad: Abbvie – Advisory Committee/Board Member, Consultant, Honorarium. Abivax – Advisory Committee/Board Member, Consultant, Honorarium. Adiso – Advisory Committee/Board Member, Consultant, Honorarium. BioFire Diagnostics – Grant/Research Support. Biomerieux – Advisory Committee/Board Member, Consultant, Honorarium. Bristol-Myers Squibb – Advisory Committee/Board Member, Consultant, Honorarium. Celltrion – Advisory Committee/Board Member, Consultant, Honorarium. Ferring – Advisory Committee/Board Member, Consultant, Honorarium. Fresenius – Advisory Committee/Board Member, Consultant, Honorarium. Genentech – Grant/Research Support. Janssen – Advisory Committee/Board Member, Consultant. Janssen – Grant/Research Support. Janssen – Honorarium. Johnson & Johnson – Advisory Committee/Board Member, Consultant. Merck – Advisory Committee/Board Member, Consultant, Honorarium. NIH NIDDK Diseases K23DK124570 – Grant/Research Support. Pfizer – Advisory Committee/Board Member, Consultant, Honorarium. Sanofi – Advisory Committee/Board Member, Consultant, Honorarium. The Crohn's and Colitis Foundation (#878246) – Grant/Research Support. The Judith & Stewart Colton Center for Autoimmunity – Grant/Research Support. Vedanta – Advisory Committee/Board Member, Consultant, Honorarium.
Adam Faye: AbbVie – Honorarium. Eli Lilly – Consultant. NIH Grant K76AG083286 – Grant/Research Support. Takeda – Honorarium. The American College of Gastroenterology – Grant/Research Support. The Crohn's and Colitis Foundation – Grant/Research Support.
Jahnavi Udaikumar, MD1, Maaz Ahsan, MD2, Olivia Delau, MS2, Simon J. Hong, MD2, Seymour Katz, MD, MACG2, Jordan Axelrad, MD, MPH3, Adam Faye, MD, MS2. P5471 - The Impact of Concomitant Hypothyroid Disease and Inflammatory Bowel Disease in Older Adults: Underrecognized and Underappreciated, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NYU Langone Health, Brooklyn, NY; 2NYU Langone Health, New York, NY; 3Division of Gastroenterology, Department of Medicine, NYU Grossman School of Medicine, New York, NY
Introduction: Inflammatory bowel disease (IBD) is a chronic immune-mediated disorder often complicated by extraintestinal manifestations (EIMs). Hypothyroidism (HT), particularly autoimmune thyroiditis, shares overlapping immunopathogenic pathways with IBD, including dysregulated T-cell activation and cytokine signaling. Although HT is linked to systemic autoimmune diseases, its impact on IBD outcomes in older adults remains unclear. We aimed to evaluate factors associated with HT in older adults with IBD and its effect on laboratory and healthcare utilization outcomes.
Methods: We conducted a retrospective study at a large academic center among adults aged ≥60 years with IBD and ≥1 thyroid-stimulating hormone (TSH) measurement prior to January 1, 2022. Patients were stratified by HT status. Demographics, clinical characteristics, medication history, labs, and healthcare utilization were collected. Associations were assessed using Chi-Squared, Fisher’s Exact, or Wilcoxon Rank-Sum tests. Multivariable logistic regression evaluated factors associated with HT, while logistic and negative binomial regression assessed HT as a predictor of anemia and healthcare utilization (2016–2022).
Results: Among 158 older adults with IBD (median age 75.4 years, 63.3% female), 119 (75.3%) had HT. Demographics, smoking status, BMI, and IBD subtype were similar by HT status (Table 1). Extraintestinal manifestations (21.0% vs 18.0%, p=0.68) and prior intestinal surgery (15.1% vs 7.7%, p=0.29) were comparable. Prior biologic therapy was more common in the HT group (30.3% vs 12.8%, p=0.03) and remained independently associated after covariate adjustment (adjOR 2.93, 95% CI: 1.05–8.20, p=0.04). Among 86 older patients followed longitudinally, HT was associated with higher anemia rates (65.2% vs 35.0%, p=0.02) and remained an independent predictor on multivariate analysis (adjOR 5.31, 95% CI: 1.52-18.58; Table 2). HT was not a significant predictor of increased healthcare utilization—including colonoscopies (adjIRR 0.91, 95% CI: 0.45–1.81), hospitalizations (adjIRR 0.94, 95% CI: 0.36–2.45), emergency department (ED) visits (adjIRR 1.67, 95% CI: 0.61–4.59), or imaging (adjIRR 1.13, 95% CI: 0.58–2.24).
Discussion: In older adults with IBD, HT was independently associated with prior biologic therapy and increased anemia burden but not greater healthcare utilization. HT may represent a marker of heightened systemic inflammation, warranting early recognition and multidisciplinary management.
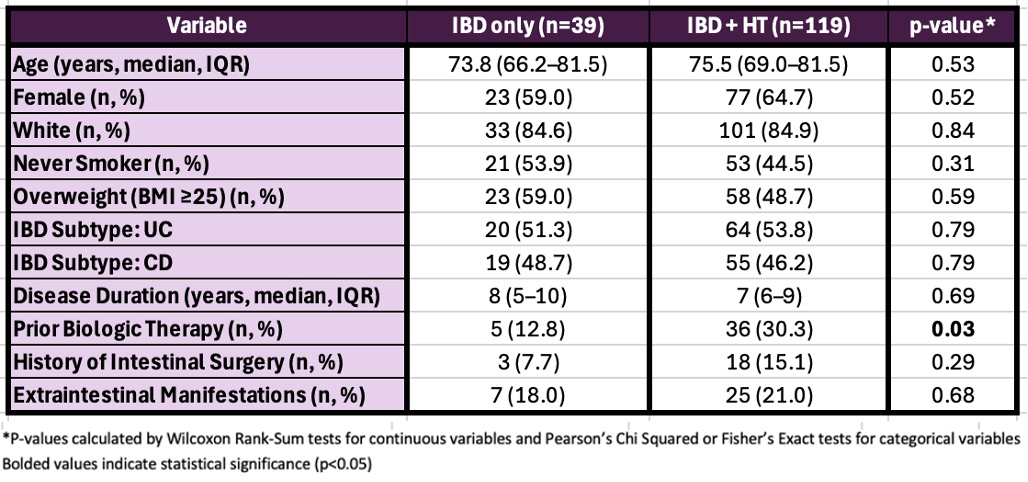
Figure: Table 1: Baseline Characteristics in Older Adults with IBD by HT Status (N = 158)
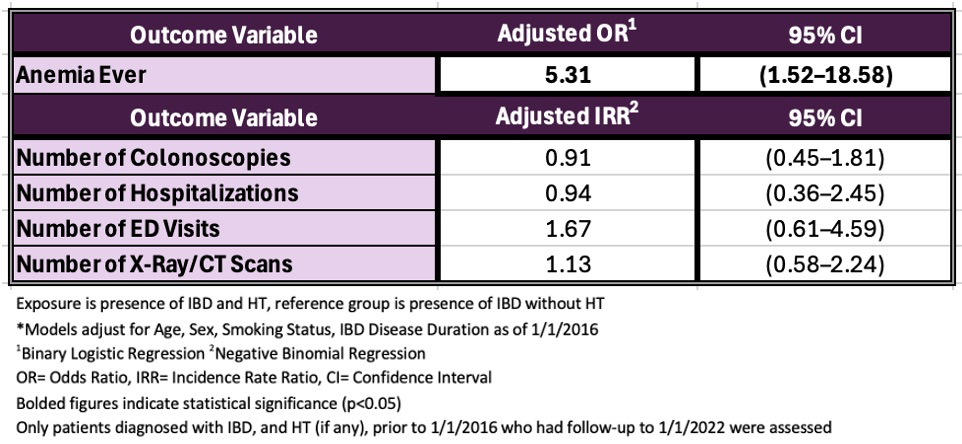
Figure: Table 2: IBD and HT as a Predictor of Anemia and Healthcare Utilization Outcomes 2016-2022 (N = 86)
Disclosures:
Jahnavi Udaikumar indicated no relevant financial relationships.
Maaz Ahsan indicated no relevant financial relationships.
Olivia Delau indicated no relevant financial relationships.
Simon Hong: Abbvie – Advisory Committee/Board Member.
Seymour Katz indicated no relevant financial relationships.
Jordan Axelrad: Abbvie – Advisory Committee/Board Member, Consultant, Honorarium. Abivax – Advisory Committee/Board Member, Consultant, Honorarium. Adiso – Advisory Committee/Board Member, Consultant, Honorarium. BioFire Diagnostics – Grant/Research Support. Biomerieux – Advisory Committee/Board Member, Consultant, Honorarium. Bristol-Myers Squibb – Advisory Committee/Board Member, Consultant, Honorarium. Celltrion – Advisory Committee/Board Member, Consultant, Honorarium. Ferring – Advisory Committee/Board Member, Consultant, Honorarium. Fresenius – Advisory Committee/Board Member, Consultant, Honorarium. Genentech – Grant/Research Support. Janssen – Advisory Committee/Board Member, Consultant. Janssen – Grant/Research Support. Janssen – Honorarium. Johnson & Johnson – Advisory Committee/Board Member, Consultant. Merck – Advisory Committee/Board Member, Consultant, Honorarium. NIH NIDDK Diseases K23DK124570 – Grant/Research Support. Pfizer – Advisory Committee/Board Member, Consultant, Honorarium. Sanofi – Advisory Committee/Board Member, Consultant, Honorarium. The Crohn's and Colitis Foundation (#878246) – Grant/Research Support. The Judith & Stewart Colton Center for Autoimmunity – Grant/Research Support. Vedanta – Advisory Committee/Board Member, Consultant, Honorarium.
Adam Faye: AbbVie – Honorarium. Eli Lilly – Consultant. NIH Grant K76AG083286 – Grant/Research Support. Takeda – Honorarium. The American College of Gastroenterology – Grant/Research Support. The Crohn's and Colitis Foundation – Grant/Research Support.
Jahnavi Udaikumar, MD1, Maaz Ahsan, MD2, Olivia Delau, MS2, Simon J. Hong, MD2, Seymour Katz, MD, MACG2, Jordan Axelrad, MD, MPH3, Adam Faye, MD, MS2. P5471 - The Impact of Concomitant Hypothyroid Disease and Inflammatory Bowel Disease in Older Adults: Underrecognized and Underappreciated, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

