Sunday Poster Session
Category: Biliary/Pancreas
P0061 - Cost Savings Validation of an Emergency Department Acute Pancreatitis Pathway
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Daniel Wang, MD
University of Southern California
Los Angeles, CA
Presenting Author(s)
Daniel Wang, MD1, Cameron M. Quon, MD2, Sunil Sheth, MD3, Helen Lee, FNP2, Lucas Nastaskin, 2, Kabir Rahal, 4, Alejandro Vasquez, BS2, James Buxbaum, MD5
1University of Southern California, Torrance, CA; 2University of Southern California, Los Angeles, CA; 3Beth Israel Deaconess Medical Center, Harvard Medical School, Bostom, MA; 4University of California Los Angeles, Los Angeles, CA; 5Keck School of Medicine of the University of Southern California, Los Angeles, CA
Introduction: Acute pancreatitis (AP) is a leading gastrointestinal cause of hospitalization, resulting in an estimated $2.5 billion in annual costs in the U.S[1]. Beth Israel Deaconess Medical Center (BIDMC) implemented an emergency department (ED)-based protocol to streamline AP triage and management, classifying patients for either observation with possible ED discharge or inpatient admission, with significant implications for cost and patient disruption[2].
Our project aimed to externally validate the BIDMC AP pathway by evaluating clinical outcomes and potential cost savings for patients who could be safely discharged.
Methods: We used a prospectively collected database of patients with mild AP at LA General Hospital (LAG). The BIDMC safe discharge protocol was applied retrospectively to assess cohort comparability and identify patients who would have qualified for ED discharge. We then compared this theoretical cohort to actual patient triage and calculated differences in inpatient days and associated costs, using the average daily reimbursement rate at our center for AP. We extrapolated findings based on 288,820 annual U.S. admissions for pancreatitis and a published savings estimate of $1,720.50 per avoided admission[3].
Results: We identified 704 patients with mild AP at LAG over a five-year period. While LAG demographics differed from BIDMC, disease severity, etiology, and pathway eligibility were similar. Applying BIDMC criteria, 210 patients (29.8%) at LAG would have been eligible for ED discharge, comparable to the 26.0% at BIDMC (p = NS). In practice, only 40 patients (5.6%) were discharged, and 170 eligible patients were admitted, resulting in 3,572.5 inpatient days and an estimated $8.1 million in costs. Assuming national discharge patterns mirror those at LAG, implementing the Safe for ED Discharge pathway could yield $120 million in annual savings.
Discussion: We applied the BIDMC ED pancreatitis protocol to a large safety-net hospital population and found substantial potential cost savings.
[1] Li C, et al. Global burden of acute pancreatitis, 1990–2019. BMC Gastroenterol. 2021;21:332. doi:10.1186/s12876-021-01906-2
[2] Anderson K, et al. ED protocol to prevent hospitalization in mild AP. Pancreatology. 2023;23(3):299–305. doi:10.1016/j.pan.2023.02.006
[3] Thiruvengadam N, et al. Projected savings from ED protocol for mild AP. Pancreatology. 2025;25(1):35–38. doi:10.1016/j.pan.2024.12.009
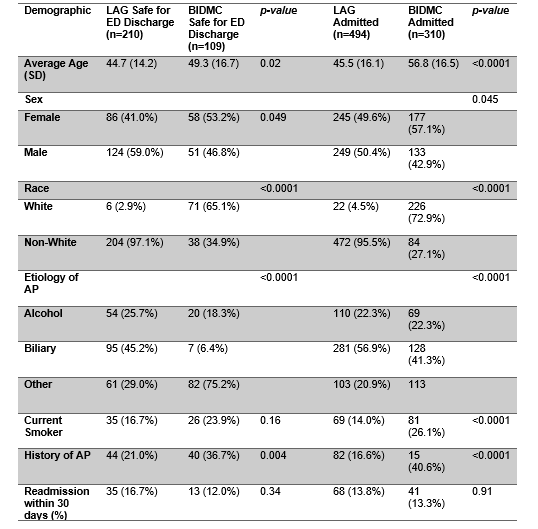
Figure: Table 1. Demographics of Safe for ED Pathway Discharges and Admissions using BIDMC Protocol at LAG Hospital
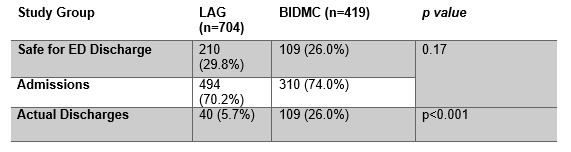
Figure: Potential and Actual Mild Acute Pancreatitis Discharges at LAG and BIDMC Hospitals Using BIDMC Protocol
Disclosures:
Daniel Wang indicated no relevant financial relationships.
Cameron Quon indicated no relevant financial relationships.
Sunil Sheth indicated no relevant financial relationships.
Helen Lee indicated no relevant financial relationships.
Lucas Nastaskin indicated no relevant financial relationships.
Kabir Rahal indicated no relevant financial relationships.
Alejandro Vasquez indicated no relevant financial relationships.
James Buxbaum: Boston Scientific – Consultant. Olympus – Consultant.
Daniel Wang, MD1, Cameron M. Quon, MD2, Sunil Sheth, MD3, Helen Lee, FNP2, Lucas Nastaskin, 2, Kabir Rahal, 4, Alejandro Vasquez, BS2, James Buxbaum, MD5. P0061 - Cost Savings Validation of an Emergency Department Acute Pancreatitis Pathway, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Southern California, Torrance, CA; 2University of Southern California, Los Angeles, CA; 3Beth Israel Deaconess Medical Center, Harvard Medical School, Bostom, MA; 4University of California Los Angeles, Los Angeles, CA; 5Keck School of Medicine of the University of Southern California, Los Angeles, CA
Introduction: Acute pancreatitis (AP) is a leading gastrointestinal cause of hospitalization, resulting in an estimated $2.5 billion in annual costs in the U.S[1]. Beth Israel Deaconess Medical Center (BIDMC) implemented an emergency department (ED)-based protocol to streamline AP triage and management, classifying patients for either observation with possible ED discharge or inpatient admission, with significant implications for cost and patient disruption[2].
Our project aimed to externally validate the BIDMC AP pathway by evaluating clinical outcomes and potential cost savings for patients who could be safely discharged.
Methods: We used a prospectively collected database of patients with mild AP at LA General Hospital (LAG). The BIDMC safe discharge protocol was applied retrospectively to assess cohort comparability and identify patients who would have qualified for ED discharge. We then compared this theoretical cohort to actual patient triage and calculated differences in inpatient days and associated costs, using the average daily reimbursement rate at our center for AP. We extrapolated findings based on 288,820 annual U.S. admissions for pancreatitis and a published savings estimate of $1,720.50 per avoided admission[3].
Results: We identified 704 patients with mild AP at LAG over a five-year period. While LAG demographics differed from BIDMC, disease severity, etiology, and pathway eligibility were similar. Applying BIDMC criteria, 210 patients (29.8%) at LAG would have been eligible for ED discharge, comparable to the 26.0% at BIDMC (p = NS). In practice, only 40 patients (5.6%) were discharged, and 170 eligible patients were admitted, resulting in 3,572.5 inpatient days and an estimated $8.1 million in costs. Assuming national discharge patterns mirror those at LAG, implementing the Safe for ED Discharge pathway could yield $120 million in annual savings.
Discussion: We applied the BIDMC ED pancreatitis protocol to a large safety-net hospital population and found substantial potential cost savings.
[1] Li C, et al. Global burden of acute pancreatitis, 1990–2019. BMC Gastroenterol. 2021;21:332. doi:10.1186/s12876-021-01906-2
[2] Anderson K, et al. ED protocol to prevent hospitalization in mild AP. Pancreatology. 2023;23(3):299–305. doi:10.1016/j.pan.2023.02.006
[3] Thiruvengadam N, et al. Projected savings from ED protocol for mild AP. Pancreatology. 2025;25(1):35–38. doi:10.1016/j.pan.2024.12.009
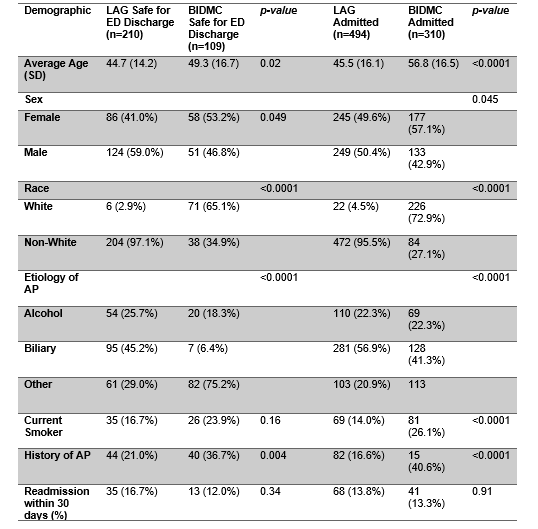
Figure: Table 1. Demographics of Safe for ED Pathway Discharges and Admissions using BIDMC Protocol at LAG Hospital
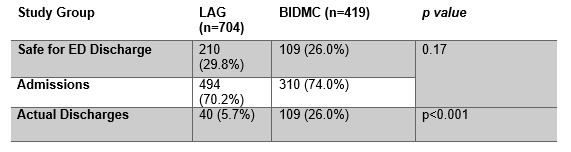
Figure: Potential and Actual Mild Acute Pancreatitis Discharges at LAG and BIDMC Hospitals Using BIDMC Protocol
Disclosures:
Daniel Wang indicated no relevant financial relationships.
Cameron Quon indicated no relevant financial relationships.
Sunil Sheth indicated no relevant financial relationships.
Helen Lee indicated no relevant financial relationships.
Lucas Nastaskin indicated no relevant financial relationships.
Kabir Rahal indicated no relevant financial relationships.
Alejandro Vasquez indicated no relevant financial relationships.
James Buxbaum: Boston Scientific – Consultant. Olympus – Consultant.
Daniel Wang, MD1, Cameron M. Quon, MD2, Sunil Sheth, MD3, Helen Lee, FNP2, Lucas Nastaskin, 2, Kabir Rahal, 4, Alejandro Vasquez, BS2, James Buxbaum, MD5. P0061 - Cost Savings Validation of an Emergency Department Acute Pancreatitis Pathway, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

