Sunday Poster Session
Category: Biliary/Pancreas
P0062 - Frequency and Predictors of Incomplete Bile Duct Clearance in Hospitalized Patients Receiving ERCP for Choledocholithiasis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Daniel Wang, MD
University of Southern California
Los Angeles, CA
Presenting Author(s)
Daniel Wang, MD1, Morgan Goodman, MD1, Patrick Chang, MD2, James Buxbaum, MD2, James Scheiman, MD, FACG3, John J.. Kim, MD, MS, FACG4
1University of Southern California, Los Angeles, CA; 2Keck School of Medicine of the University of Southern California, Los Angeles, CA; 3University of Michigan, Los Angeles, MI; 4Los Angeles General Medical Center, Los Angeles, CA
Introduction:
Background: Choledocholithiasis is the most common indication for endoscopic retrograde cholangiopancreatography (ERCP), and ERCP is highly effective in clearing bile duct stones. However, when complete bile duct clearance is not achieved, biliary stents are placed to ensure biliary drainage, necessitating a repeat procedure.
Aims: To evaluate frequency and factors associated with incomplete bile duct clearance in hospitalized patients receiving ERCP for choledocholithiasis.
Methods: National Inpatient Sample (NIS) database (2016-2020) was queried for patients who received ERCP for primary indication of choledocholithiasis without concurrent cholangitis or other biliary tract diseases. Patients receiving ERCP and sphincterotomy with or without a biliary stent were examined. The primary endpoint was complete bile duct clearance defined by patients not requiring a biliary stent after a sphincterotomy. Annual rates of complete bile duct clearance were calculated, and multi-variate analysis was performed to evaluate factors associated with incomplete bile duct clearance.
Results: During the study period, 48,366 patients (mean age 58.2+20.9 years, 17,972 (37.2%) male) met study criteria. Overall, complete bile duct clearance was achieved in 38,125 (78.8%) patients after index ERCP with sphincterotomy, and the annual complete bile duct clearance rates declined over time (P=0.001) (Figure). During the same hospitalization, 29,145 (60.3%) patients also received cholecystectomy. On multi-variate analysis, hospital settings (Midwest or Northeast vs. West, nonfederal government vs. private not-for-profit, and large vs. small/medium bed size) and not receiving in-hospital cholecystectomy increased the odds of incomplete bile duct clearance after adjusting for age, gender, race/ethnicity, comorbidities, and insurance status (Table).
Discussion: More than a fifth of hospitalized patients with choledocholithiasis failed to achieve complete bile duct clearance during the index ERCP. After adjusting for patient-related factors, geography and failure to receive cholecystectomy during hospitalization were primary predictors of incomplete bile duct clearance. Substantial variation in primary complete stone clearance rates during ERCP, other than patient-related factors, suggests opportunity for quality and process improvement.
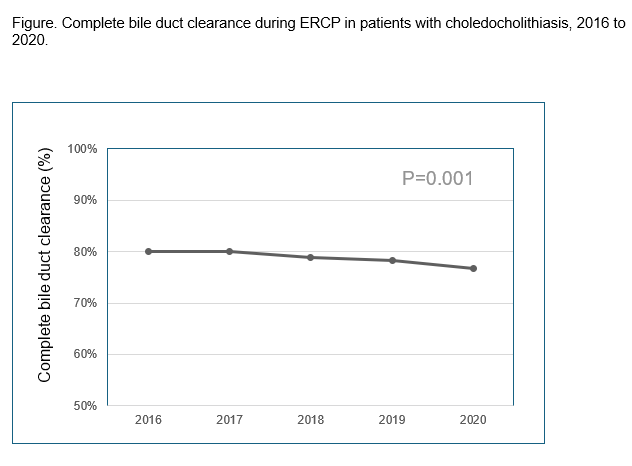
Figure: Figure. Annual complete bile duct clearance rates during ERCP in patients with choledocholithiasis, 2016 to 2020.
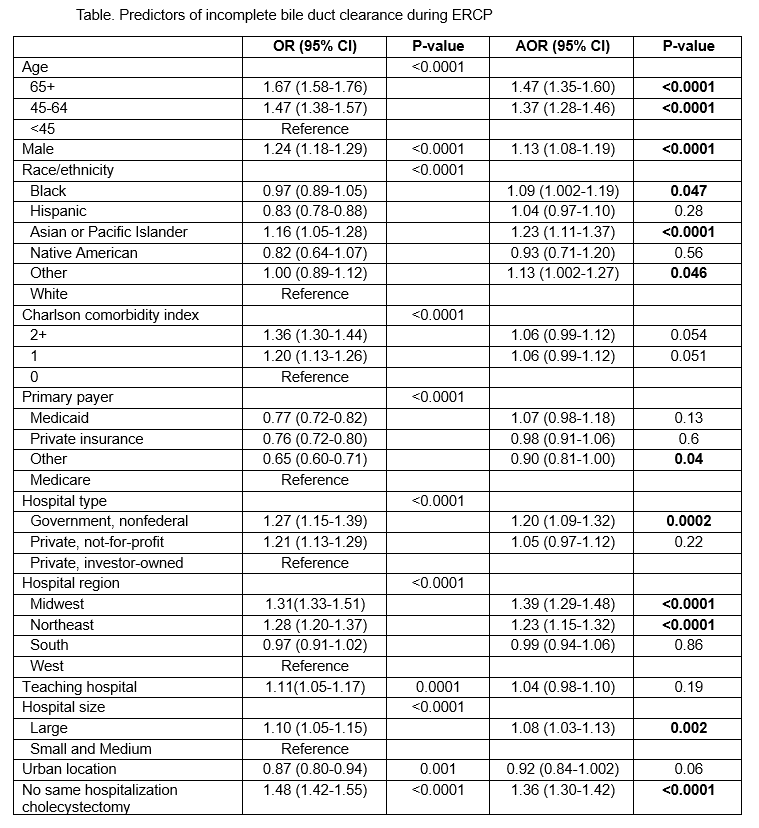
Figure: Table. Predictors of incomplete bile duct clearance during ERCP
Disclosures:
Daniel Wang indicated no relevant financial relationships.
Morgan Goodman indicated no relevant financial relationships.
Patrick Chang indicated no relevant financial relationships.
James Buxbaum: Boston Scientific – Consultant. Olympus – Consultant.
James Scheiman indicated no relevant financial relationships.
John Kim indicated no relevant financial relationships.
Daniel Wang, MD1, Morgan Goodman, MD1, Patrick Chang, MD2, James Buxbaum, MD2, James Scheiman, MD, FACG3, John J.. Kim, MD, MS, FACG4. P0062 - Frequency and Predictors of Incomplete Bile Duct Clearance in Hospitalized Patients Receiving ERCP for Choledocholithiasis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Southern California, Los Angeles, CA; 2Keck School of Medicine of the University of Southern California, Los Angeles, CA; 3University of Michigan, Los Angeles, MI; 4Los Angeles General Medical Center, Los Angeles, CA
Introduction:
Background: Choledocholithiasis is the most common indication for endoscopic retrograde cholangiopancreatography (ERCP), and ERCP is highly effective in clearing bile duct stones. However, when complete bile duct clearance is not achieved, biliary stents are placed to ensure biliary drainage, necessitating a repeat procedure.
Aims: To evaluate frequency and factors associated with incomplete bile duct clearance in hospitalized patients receiving ERCP for choledocholithiasis.
Methods: National Inpatient Sample (NIS) database (2016-2020) was queried for patients who received ERCP for primary indication of choledocholithiasis without concurrent cholangitis or other biliary tract diseases. Patients receiving ERCP and sphincterotomy with or without a biliary stent were examined. The primary endpoint was complete bile duct clearance defined by patients not requiring a biliary stent after a sphincterotomy. Annual rates of complete bile duct clearance were calculated, and multi-variate analysis was performed to evaluate factors associated with incomplete bile duct clearance.
Results: During the study period, 48,366 patients (mean age 58.2+20.9 years, 17,972 (37.2%) male) met study criteria. Overall, complete bile duct clearance was achieved in 38,125 (78.8%) patients after index ERCP with sphincterotomy, and the annual complete bile duct clearance rates declined over time (P=0.001) (Figure). During the same hospitalization, 29,145 (60.3%) patients also received cholecystectomy. On multi-variate analysis, hospital settings (Midwest or Northeast vs. West, nonfederal government vs. private not-for-profit, and large vs. small/medium bed size) and not receiving in-hospital cholecystectomy increased the odds of incomplete bile duct clearance after adjusting for age, gender, race/ethnicity, comorbidities, and insurance status (Table).
Discussion: More than a fifth of hospitalized patients with choledocholithiasis failed to achieve complete bile duct clearance during the index ERCP. After adjusting for patient-related factors, geography and failure to receive cholecystectomy during hospitalization were primary predictors of incomplete bile duct clearance. Substantial variation in primary complete stone clearance rates during ERCP, other than patient-related factors, suggests opportunity for quality and process improvement.
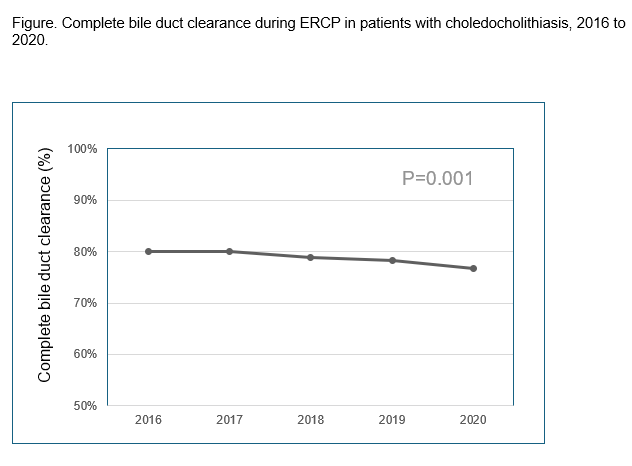
Figure: Figure. Annual complete bile duct clearance rates during ERCP in patients with choledocholithiasis, 2016 to 2020.
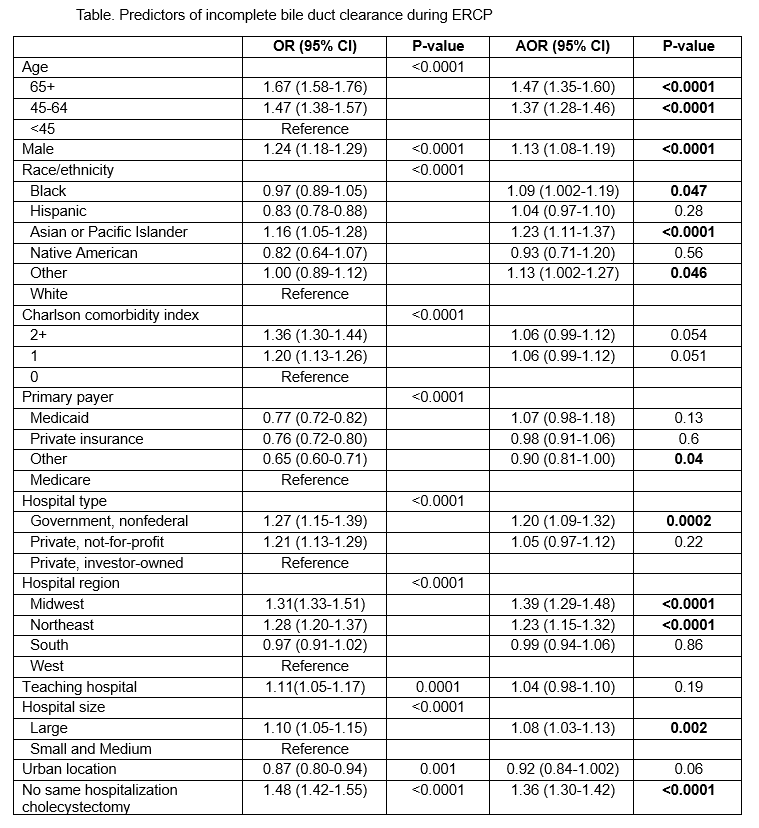
Figure: Table. Predictors of incomplete bile duct clearance during ERCP
Disclosures:
Daniel Wang indicated no relevant financial relationships.
Morgan Goodman indicated no relevant financial relationships.
Patrick Chang indicated no relevant financial relationships.
James Buxbaum: Boston Scientific – Consultant. Olympus – Consultant.
James Scheiman indicated no relevant financial relationships.
John Kim indicated no relevant financial relationships.
Daniel Wang, MD1, Morgan Goodman, MD1, Patrick Chang, MD2, James Buxbaum, MD2, James Scheiman, MD, FACG3, John J.. Kim, MD, MS, FACG4. P0062 - Frequency and Predictors of Incomplete Bile Duct Clearance in Hospitalized Patients Receiving ERCP for Choledocholithiasis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
