Monday Poster Session
Category: Biliary/Pancreas
P2273 - Severe Hyperbilirubinemia and Multi-Organ Failure in a Patient With Weil’s Disease
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Amro Abdellatief, MD (he/him/his)
Howard University Hospital
Washington, DC
Presenting Author(s)
Amro Abdellatief, MD1, Justice Arhinful, MD1, Kristen Miller, MD1, Sneha Adidam, MD1, Mesay Asfaw, MD1, Juan C. Santiago-Gonzalez, MD, MSc1, Jacqueline Laurin, MD2
1Howard University Hospital, Washington, DC; 2Johns Hopkins University, Arlington, VA
Introduction: Leptospirosis is the most common zoonosis worldwide1. It's prevalence in the United States is low, with around 100-150 cases annually, mostly in Hawaii and Puerto Rico2. It's a bacterial infection caused by Leptospira and is transmitted through direct contact with the urine of infected animals, such as rodents3. Symptoms can range from asymptomatic infection to life-threatening multi-organ failure, known as Weil’s disease3.
Case Description/
Methods: A 68-year-old retired male dentist with a medical history only for asthma, presented with 4 days of fever, rigors, nausea, non-bilious non-bloody vomiting, thirst, arthralgia, orange-colored urine, and diarrhea after he ate a tuna sandwich. In the emergency department (ED), he was febrile, tachycardic, and hypotensive despite 3 L of fluids. Physical examination revealed jaundice, and dry mucous membranes. Laboratory results indicated acute kidney injury (AKI), severe thrombocytopenia (platelets 20), leukocytosis (WBC 18,000), and conjugated hyperbilirubinemia (peaking at 22, primarily conjugated) with normal AST, ALT, and ALK. He was admitted to the ICU for septic shock and was started on pressors, hemodialysis and piperacillin/tazobactam. Blood smears were negative for schistocytes. Viral hepatitis panel, including hepatitis C, Epstein-Barr virus (EBV) and cytomegalovirus (CMV) PCRs, were negative. Blood cultures, urine Legionella antigen test and Hantavirus serology were negative. Stool cultures were also negative. A subsequent CT scan of the abdomen revealed large hematomas in the bilateral psoas muscles (Figures 1 + 2)) An MRCP showed no bile duct dilatation, obstruction, or masses. Due to dropping hemoglobin (HgB), he received multiple blood transfusions. The patient lived near a park with several lakes containing brackish water, where rats frequently ran into his basement. Leptospira PCR returned positive in both blood and urine. He was started on doxycycline with gradual weaning off of dialysis, and made a slow recovery.
Discussion: Weil’s disease is a life-threatening disease which presents with non-specific symptoms Key clues include a combination of fever, renal failure, conjugated hyperbilirubinemia with normal or slightly elevated liver enzymes. The combination of previously described symptoms, multiorgan failure, and disproportionate conjugated hyperbilirubinemia with normal to slightly elevated liver associated enzymes should raise suspicion for leptospirosis. Prompt ICU admission and treatment with antibiotics can be life-saving.
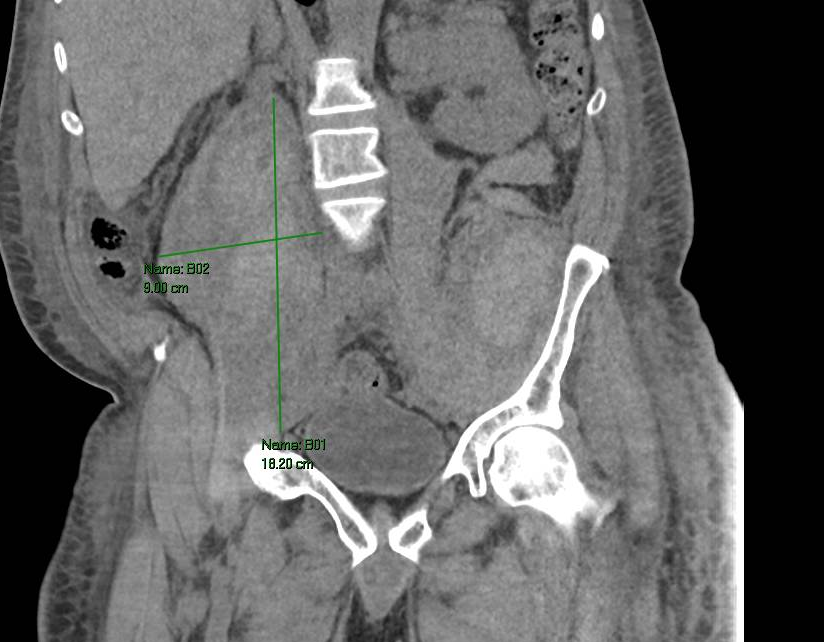
Figure: FIgure 1, Large right iliopsoas hematoma (18 x 9.0 cm)

Figure: Figure 2. Left iliopsoas hematoma (18 x 6.0 cm)
Disclosures:
Amro Abdellatief indicated no relevant financial relationships.
Justice Arhinful indicated no relevant financial relationships.
Kristen Miller indicated no relevant financial relationships.
Sneha Adidam indicated no relevant financial relationships.
Mesay Asfaw indicated no relevant financial relationships.
Juan Santiago-Gonzalez indicated no relevant financial relationships.
Jacqueline Laurin indicated no relevant financial relationships.
Amro Abdellatief, MD1, Justice Arhinful, MD1, Kristen Miller, MD1, Sneha Adidam, MD1, Mesay Asfaw, MD1, Juan C. Santiago-Gonzalez, MD, MSc1, Jacqueline Laurin, MD2. P2273 - Severe Hyperbilirubinemia and Multi-Organ Failure in a Patient With Weil’s Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Howard University Hospital, Washington, DC; 2Johns Hopkins University, Arlington, VA
Introduction: Leptospirosis is the most common zoonosis worldwide1. It's prevalence in the United States is low, with around 100-150 cases annually, mostly in Hawaii and Puerto Rico2. It's a bacterial infection caused by Leptospira and is transmitted through direct contact with the urine of infected animals, such as rodents3. Symptoms can range from asymptomatic infection to life-threatening multi-organ failure, known as Weil’s disease3.
Case Description/
Methods: A 68-year-old retired male dentist with a medical history only for asthma, presented with 4 days of fever, rigors, nausea, non-bilious non-bloody vomiting, thirst, arthralgia, orange-colored urine, and diarrhea after he ate a tuna sandwich. In the emergency department (ED), he was febrile, tachycardic, and hypotensive despite 3 L of fluids. Physical examination revealed jaundice, and dry mucous membranes. Laboratory results indicated acute kidney injury (AKI), severe thrombocytopenia (platelets 20), leukocytosis (WBC 18,000), and conjugated hyperbilirubinemia (peaking at 22, primarily conjugated) with normal AST, ALT, and ALK. He was admitted to the ICU for septic shock and was started on pressors, hemodialysis and piperacillin/tazobactam. Blood smears were negative for schistocytes. Viral hepatitis panel, including hepatitis C, Epstein-Barr virus (EBV) and cytomegalovirus (CMV) PCRs, were negative. Blood cultures, urine Legionella antigen test and Hantavirus serology were negative. Stool cultures were also negative. A subsequent CT scan of the abdomen revealed large hematomas in the bilateral psoas muscles (Figures 1 + 2)) An MRCP showed no bile duct dilatation, obstruction, or masses. Due to dropping hemoglobin (HgB), he received multiple blood transfusions. The patient lived near a park with several lakes containing brackish water, where rats frequently ran into his basement. Leptospira PCR returned positive in both blood and urine. He was started on doxycycline with gradual weaning off of dialysis, and made a slow recovery.
Discussion: Weil’s disease is a life-threatening disease which presents with non-specific symptoms Key clues include a combination of fever, renal failure, conjugated hyperbilirubinemia with normal or slightly elevated liver enzymes. The combination of previously described symptoms, multiorgan failure, and disproportionate conjugated hyperbilirubinemia with normal to slightly elevated liver associated enzymes should raise suspicion for leptospirosis. Prompt ICU admission and treatment with antibiotics can be life-saving.
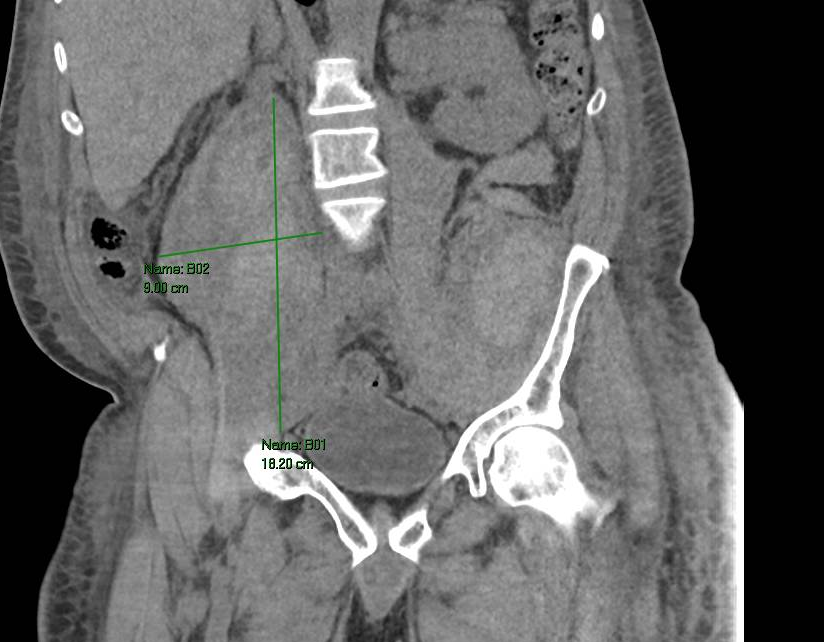
Figure: FIgure 1, Large right iliopsoas hematoma (18 x 9.0 cm)

Figure: Figure 2. Left iliopsoas hematoma (18 x 6.0 cm)
Disclosures:
Amro Abdellatief indicated no relevant financial relationships.
Justice Arhinful indicated no relevant financial relationships.
Kristen Miller indicated no relevant financial relationships.
Sneha Adidam indicated no relevant financial relationships.
Mesay Asfaw indicated no relevant financial relationships.
Juan Santiago-Gonzalez indicated no relevant financial relationships.
Jacqueline Laurin indicated no relevant financial relationships.
Amro Abdellatief, MD1, Justice Arhinful, MD1, Kristen Miller, MD1, Sneha Adidam, MD1, Mesay Asfaw, MD1, Juan C. Santiago-Gonzalez, MD, MSc1, Jacqueline Laurin, MD2. P2273 - Severe Hyperbilirubinemia and Multi-Organ Failure in a Patient With Weil’s Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

