Sunday Poster Session
Category: Biliary/Pancreas
P0001 - EUS-Guided Hepaticogastrostomy versus EUS-Guided Hepaticogastrostomy With Antegrade Stent Placement in Patients With Unresectable Malignant Distal Biliary Obstruction: A Meta-Analysis of Individual Patient Data
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Sadia Fatima Paracha, MBBS (she/her/hers)
Massachusetts General Hospital
revere, MA
Presenting Author(s)
Ahmad Abdelrazek, MD1, Sara Metwally, MD2, Sadia Fatima Paracha, MBBS3, Mahmoud Shaaban Abdelgalil, MD4, Ryad Z. Iqbal, BS5, Manar Alaa Mabrouk, MBBCh6, Abdullah Nizar, 7, Mohamed Nasser, MBBCh8, Mahmoud Samir. Mohamed, MD9, Nader Abdel Razek, MD10, Abid A. Wazir, 7, Amro Hassan, MD11
1Hartford HealthCare - St. Vincent's Hospital, Bridgeport, CT; 2Corewell Health, Rochester Hills, MI; 3Massachusetts General Hospital, Boston, MA; 4Ain Shams University, Cairo, Al Qahirah, Egypt; 5Wayne State University, Bloomfield Hills, MI; 6Faculty of Medicine fayoum university, Al Fayyum, Al Fayyum, Egypt; 7University of Michigan, Farmington Hills, MI; 8faculty of medicine, minia university, ElMinia, Al Minya, Egypt; 9Case Western Reserve University, Cleveland, OH; 10Duke University, Durham, NC; 11Kuwaiti Ministry of health, Fahad Al-Ahmad, Al Ahmadi, Kuwait
Introduction: In patients with malignant biliary obstruction (MBO) where endoscopic retrograde cholangiopancreatography (ERCP) has failed, endoscopic ultrasound-guided hepaticogastrostomy (EUS-HGS) serves as an important rescue procedure. This study aimed to compare the safety and effectiveness of EUS-HGS alone versus EUS-HGS combined with antegrade stenting (EUS-HGAS) in this patient population.
Methods: A comprehensive literature search was performed in PubMed, SCOPUS, and Web of Science to identify studies comparing endoscopic ultrasound-guided hepaticogastrostomy (EUS-HGS) with EUS-HGS combined with antegrade stenting (EUS-HGAS) in patients with malignant biliary obstruction (MBO). The primary outcomes were the rate of recurrent biliary obstruction (RBO), the need for reinterventions, and time to RBO (TRBO). Secondary outcomes included technical success, clinical success, procedure duration, and the overall incidence of adverse events. Individual patient survival data for TRBO were extracted from Kaplan Meier curves and reconstructed using restricted mean survival time analysis.
Results: Five observational studies comprising a total of 451 patients with MBO were included, with 239 patients receiving EUS-HGS and 212 undergoing EUS-HGAS. Compared to EUS-HGAS, EUS-HGS was associated with a significantly higher rate of RBO (RR = 3.52; 95% CI: 1.95–6.36; P < 0.0001) and reintervention (RR = 2.72; 95% CI: 1.30–5.69; P = 0.008). Additionally, TRBO was significantly longer in the EUS-HGAS group (median: 715 days vs. 235 days; HR = 0.15; 95% CI: 0.03–0.83; P = 0.03). However, EUS-HGS was associated with a significantly shorter procedure time (MD = –4.01; 95% CI: –7.77 to –0.24; P = 0.04). No significant differences were found between the two groups in terms of technical success, clinical success, or overall adverse events.
Discussion: In patients with MBO following failed ERCP, EUS-HGAS appears to offer superior outcomes compared to EUS-HGS alone, with significantly lower incidence of recurrent biliary obstruction , reintervention, and longer TRBO. Although EUS-HGS is associated with a shorter procedure time, both techniques demonstrate comparable technical and clinical success rates, as well as similar safety profiles. These findings suggest that EUS-HGAS may be the preferred approach when feasible.
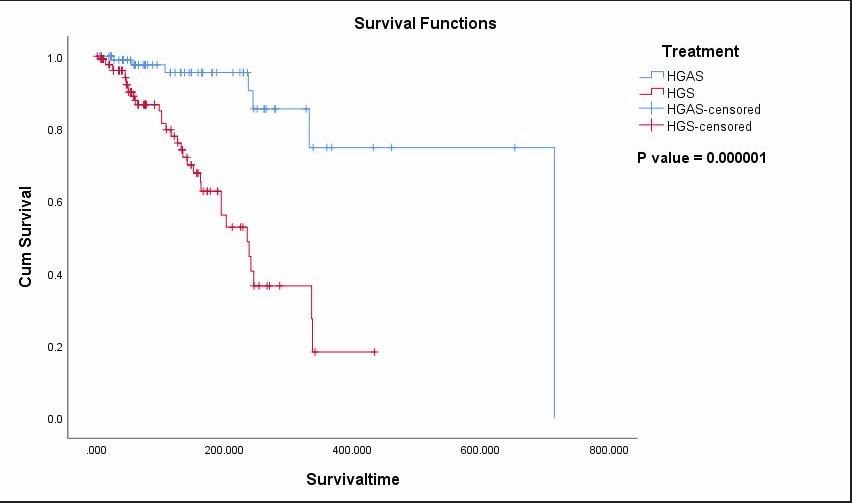
Figure: Kaplan-Meier survival curve comparing HGAS and HGS treatments based on reconstructed individual patient data. (Fig A)
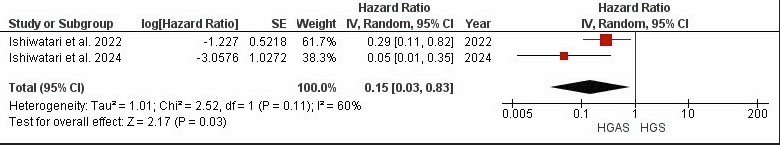
Figure: Forest Plot of Risk Ratios for Recurrent Biliary Obstruction in HGS vs. HGAS. (Fig B)
Disclosures:
Ahmad Abdelrazek indicated no relevant financial relationships.
Sara Metwally indicated no relevant financial relationships.
Sadia Fatima Paracha indicated no relevant financial relationships.
Mahmoud Shaaban Abdelgalil indicated no relevant financial relationships.
Ryad Iqbal indicated no relevant financial relationships.
Manar Alaa Mabrouk indicated no relevant financial relationships.
Abdullah Nizar indicated no relevant financial relationships.
Mohamed Nasser indicated no relevant financial relationships.
Mahmoud Mohamed indicated no relevant financial relationships.
Nader Abdel Razek indicated no relevant financial relationships.
Abid Wazir indicated no relevant financial relationships.
Amro Hassan indicated no relevant financial relationships.
Ahmad Abdelrazek, MD1, Sara Metwally, MD2, Sadia Fatima Paracha, MBBS3, Mahmoud Shaaban Abdelgalil, MD4, Ryad Z. Iqbal, BS5, Manar Alaa Mabrouk, MBBCh6, Abdullah Nizar, 7, Mohamed Nasser, MBBCh8, Mahmoud Samir. Mohamed, MD9, Nader Abdel Razek, MD10, Abid A. Wazir, 7, Amro Hassan, MD11. P0001 - EUS-Guided Hepaticogastrostomy versus EUS-Guided Hepaticogastrostomy With Antegrade Stent Placement in Patients With Unresectable Malignant Distal Biliary Obstruction: A Meta-Analysis of Individual Patient Data, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Hartford HealthCare - St. Vincent's Hospital, Bridgeport, CT; 2Corewell Health, Rochester Hills, MI; 3Massachusetts General Hospital, Boston, MA; 4Ain Shams University, Cairo, Al Qahirah, Egypt; 5Wayne State University, Bloomfield Hills, MI; 6Faculty of Medicine fayoum university, Al Fayyum, Al Fayyum, Egypt; 7University of Michigan, Farmington Hills, MI; 8faculty of medicine, minia university, ElMinia, Al Minya, Egypt; 9Case Western Reserve University, Cleveland, OH; 10Duke University, Durham, NC; 11Kuwaiti Ministry of health, Fahad Al-Ahmad, Al Ahmadi, Kuwait
Introduction: In patients with malignant biliary obstruction (MBO) where endoscopic retrograde cholangiopancreatography (ERCP) has failed, endoscopic ultrasound-guided hepaticogastrostomy (EUS-HGS) serves as an important rescue procedure. This study aimed to compare the safety and effectiveness of EUS-HGS alone versus EUS-HGS combined with antegrade stenting (EUS-HGAS) in this patient population.
Methods: A comprehensive literature search was performed in PubMed, SCOPUS, and Web of Science to identify studies comparing endoscopic ultrasound-guided hepaticogastrostomy (EUS-HGS) with EUS-HGS combined with antegrade stenting (EUS-HGAS) in patients with malignant biliary obstruction (MBO). The primary outcomes were the rate of recurrent biliary obstruction (RBO), the need for reinterventions, and time to RBO (TRBO). Secondary outcomes included technical success, clinical success, procedure duration, and the overall incidence of adverse events. Individual patient survival data for TRBO were extracted from Kaplan Meier curves and reconstructed using restricted mean survival time analysis.
Results: Five observational studies comprising a total of 451 patients with MBO were included, with 239 patients receiving EUS-HGS and 212 undergoing EUS-HGAS. Compared to EUS-HGAS, EUS-HGS was associated with a significantly higher rate of RBO (RR = 3.52; 95% CI: 1.95–6.36; P < 0.0001) and reintervention (RR = 2.72; 95% CI: 1.30–5.69; P = 0.008). Additionally, TRBO was significantly longer in the EUS-HGAS group (median: 715 days vs. 235 days; HR = 0.15; 95% CI: 0.03–0.83; P = 0.03). However, EUS-HGS was associated with a significantly shorter procedure time (MD = –4.01; 95% CI: –7.77 to –0.24; P = 0.04). No significant differences were found between the two groups in terms of technical success, clinical success, or overall adverse events.
Discussion: In patients with MBO following failed ERCP, EUS-HGAS appears to offer superior outcomes compared to EUS-HGS alone, with significantly lower incidence of recurrent biliary obstruction , reintervention, and longer TRBO. Although EUS-HGS is associated with a shorter procedure time, both techniques demonstrate comparable technical and clinical success rates, as well as similar safety profiles. These findings suggest that EUS-HGAS may be the preferred approach when feasible.
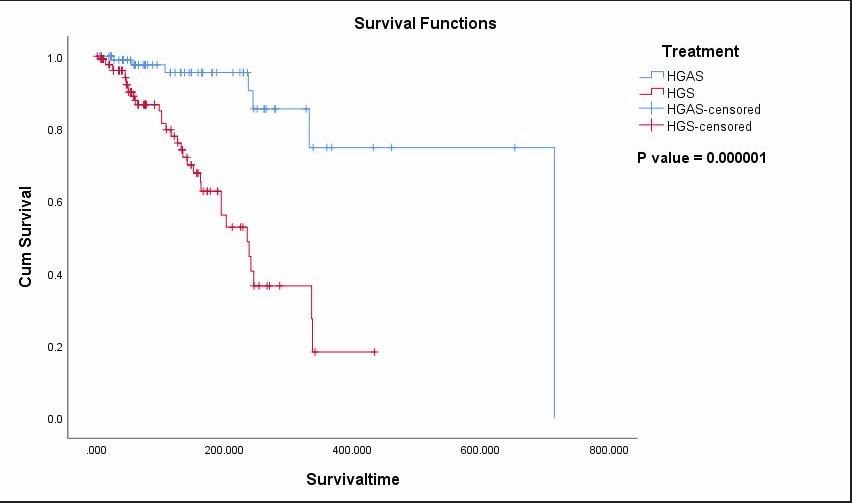
Figure: Kaplan-Meier survival curve comparing HGAS and HGS treatments based on reconstructed individual patient data. (Fig A)
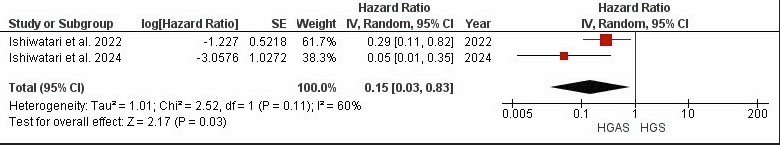
Figure: Forest Plot of Risk Ratios for Recurrent Biliary Obstruction in HGS vs. HGAS. (Fig B)
Disclosures:
Ahmad Abdelrazek indicated no relevant financial relationships.
Sara Metwally indicated no relevant financial relationships.
Sadia Fatima Paracha indicated no relevant financial relationships.
Mahmoud Shaaban Abdelgalil indicated no relevant financial relationships.
Ryad Iqbal indicated no relevant financial relationships.
Manar Alaa Mabrouk indicated no relevant financial relationships.
Abdullah Nizar indicated no relevant financial relationships.
Mohamed Nasser indicated no relevant financial relationships.
Mahmoud Mohamed indicated no relevant financial relationships.
Nader Abdel Razek indicated no relevant financial relationships.
Abid Wazir indicated no relevant financial relationships.
Amro Hassan indicated no relevant financial relationships.
Ahmad Abdelrazek, MD1, Sara Metwally, MD2, Sadia Fatima Paracha, MBBS3, Mahmoud Shaaban Abdelgalil, MD4, Ryad Z. Iqbal, BS5, Manar Alaa Mabrouk, MBBCh6, Abdullah Nizar, 7, Mohamed Nasser, MBBCh8, Mahmoud Samir. Mohamed, MD9, Nader Abdel Razek, MD10, Abid A. Wazir, 7, Amro Hassan, MD11. P0001 - EUS-Guided Hepaticogastrostomy versus EUS-Guided Hepaticogastrostomy With Antegrade Stent Placement in Patients With Unresectable Malignant Distal Biliary Obstruction: A Meta-Analysis of Individual Patient Data, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
