Sunday Poster Session
Category: Biliary/Pancreas
P0054 - Cost-Effectiveness of Cholangioscopy-Guided Biopsy as a Primary Diagnostic Tool for Indeterminate Biliary Stricture
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Noppachai Siranart, MD
Brigham and Women's Hospital, Harvard Medical School
Boston, MA
Presenting Author(s)
Noppachai Siranart, MD1, Patavee Pajareya, MD2, Kittithat Tantitanawat, MD3, Steven Steinway, MD4
1Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 2King Chulalongkorn Memorial Hospital, Bangkok, Krung Thep, Thailand; 3Phramongkutklao Hospital, Bangkok, Krung Thep, Thailand; 4Brigham and Women's Hospital, Boston, MA
Introduction: Cholangioscopy offers direct visualization and higher diagnostic accuracy than conventional ERCP for evaluating indeterminate biliary strictures. Despite its diagnostic benefits, its cost and limited availability have led guidelines to recommend it as a second-line tool after inconclusive ERCP. The cost-effectiveness of earlier cholangioscopy use remains uncertain. We aimed to evaluate the cost-effectiveness of ERCP- and cholangioscopy-based strategies for diagnosing indeterminate biliary strictures.
Methods: A deterministic Markov cohort model was developed from the U.S. healthcare payer’s perspective to assess three diagnostic strategies: (1) ERCP followed by repeat ERCP (E-E), (2) ERCP followed by cholangioscopy (E-C), and (3) cholangioscopy followed by repeat cholangioscopy (C-C). The model incorporated published estimates of diagnostic accuracy for tissue sampling by ERCP and cholangioscopy, and health utility values for cholangiocarcinoma (CCA) and related health states. Outcomes included costs (USD), quality-adjusted life years (QALYs), and incremental cost-effectiveness ratios (ICERs), using both 3-year and lifetime horizons with a 3% annual discount rate. A willingness-to-pay (WTP) threshold of $100,000/QALY was applied. Sensitivity analyses explored the impact of key parameters, including diagnostic accuracy, baseline utility, and CCA prevalence.
Results: In the base-case analysis, C-C yielded 1.53 QALYs at a cost of $21,431, followed by E-C (1.40 QALYs, $14,651) and E-E (1.39 QALYs, $14,208). The ICER for C-C vs E-E was $52,049/QALY; for E-C vs E-E, $44,821/QALY. Net monetary benefit (NMB) was highest for C-C ($131,812). At a $100,000 WTP, C-C was optimal in 99.01% of simulations. Cost-effectiveness acceptability curves showed C-C became optimal at WTP >$50,000. Threshold analysis showed E-E was favored when WTP was < $45,000. Two-way sensitivity analysis revealed C-C was most cost-effective when baseline utility exceeded 0.4; E-E and E-C were preferred when baseline utility was lower, depending on CCA prevalence.
Discussion: Cholangioscopy as the initial diagnostic tool is a cost-effective strategy for evaluating indeterminate biliary strictures, especially in settings with higher CCA prevalence or higher baseline utility in the post-diagnosis state.
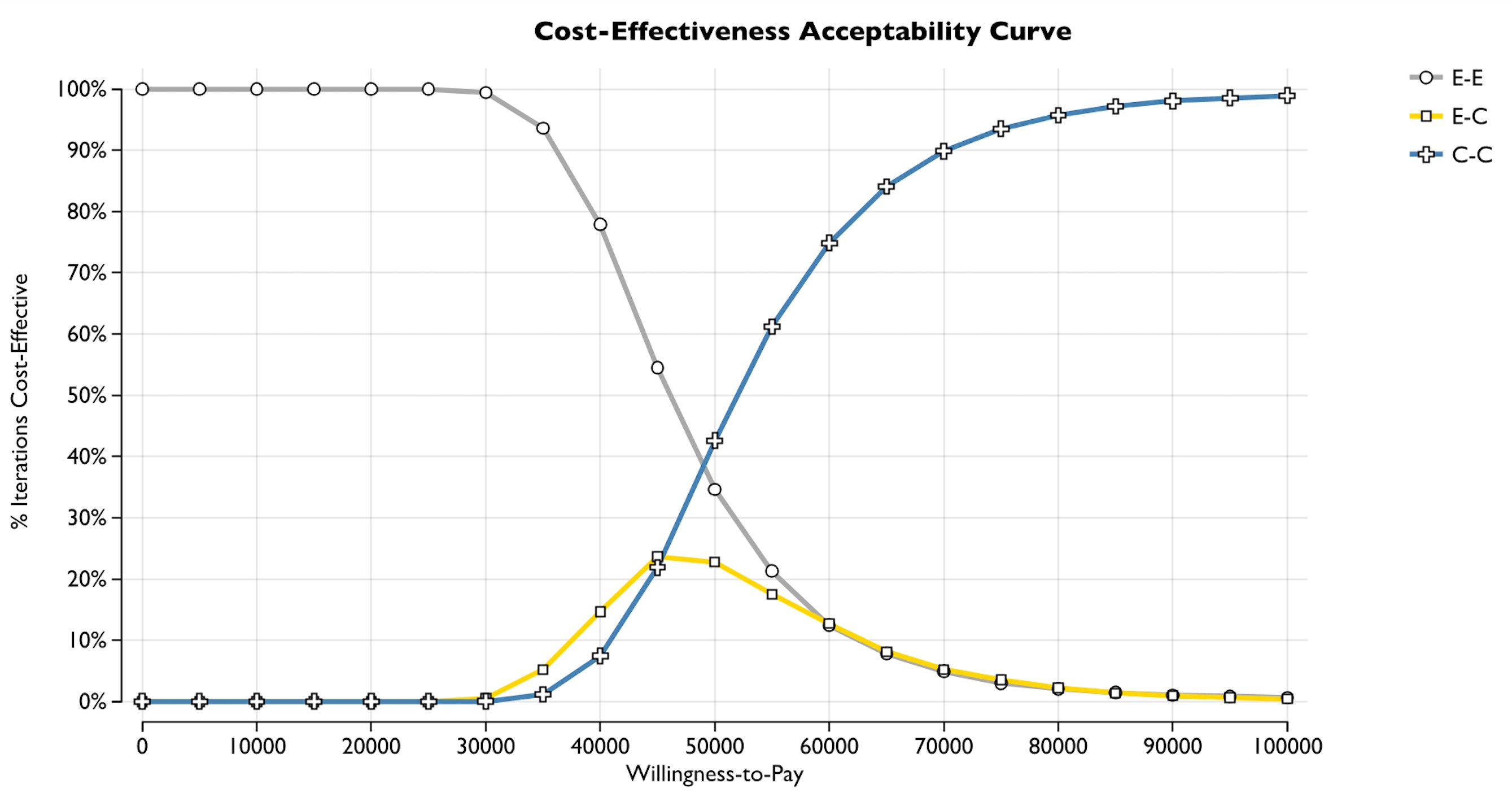
Figure: Figure 1.

Figure: Figure 2.
Disclosures:
Noppachai Siranart indicated no relevant financial relationships.
Patavee Pajareya indicated no relevant financial relationships.
Kittithat Tantitanawat indicated no relevant financial relationships.
Steven Steinway indicated no relevant financial relationships.
Noppachai Siranart, MD1, Patavee Pajareya, MD2, Kittithat Tantitanawat, MD3, Steven Steinway, MD4. P0054 - Cost-Effectiveness of Cholangioscopy-Guided Biopsy as a Primary Diagnostic Tool for Indeterminate Biliary Stricture, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 2King Chulalongkorn Memorial Hospital, Bangkok, Krung Thep, Thailand; 3Phramongkutklao Hospital, Bangkok, Krung Thep, Thailand; 4Brigham and Women's Hospital, Boston, MA
Introduction: Cholangioscopy offers direct visualization and higher diagnostic accuracy than conventional ERCP for evaluating indeterminate biliary strictures. Despite its diagnostic benefits, its cost and limited availability have led guidelines to recommend it as a second-line tool after inconclusive ERCP. The cost-effectiveness of earlier cholangioscopy use remains uncertain. We aimed to evaluate the cost-effectiveness of ERCP- and cholangioscopy-based strategies for diagnosing indeterminate biliary strictures.
Methods: A deterministic Markov cohort model was developed from the U.S. healthcare payer’s perspective to assess three diagnostic strategies: (1) ERCP followed by repeat ERCP (E-E), (2) ERCP followed by cholangioscopy (E-C), and (3) cholangioscopy followed by repeat cholangioscopy (C-C). The model incorporated published estimates of diagnostic accuracy for tissue sampling by ERCP and cholangioscopy, and health utility values for cholangiocarcinoma (CCA) and related health states. Outcomes included costs (USD), quality-adjusted life years (QALYs), and incremental cost-effectiveness ratios (ICERs), using both 3-year and lifetime horizons with a 3% annual discount rate. A willingness-to-pay (WTP) threshold of $100,000/QALY was applied. Sensitivity analyses explored the impact of key parameters, including diagnostic accuracy, baseline utility, and CCA prevalence.
Results: In the base-case analysis, C-C yielded 1.53 QALYs at a cost of $21,431, followed by E-C (1.40 QALYs, $14,651) and E-E (1.39 QALYs, $14,208). The ICER for C-C vs E-E was $52,049/QALY; for E-C vs E-E, $44,821/QALY. Net monetary benefit (NMB) was highest for C-C ($131,812). At a $100,000 WTP, C-C was optimal in 99.01% of simulations. Cost-effectiveness acceptability curves showed C-C became optimal at WTP >$50,000. Threshold analysis showed E-E was favored when WTP was < $45,000. Two-way sensitivity analysis revealed C-C was most cost-effective when baseline utility exceeded 0.4; E-E and E-C were preferred when baseline utility was lower, depending on CCA prevalence.
Discussion: Cholangioscopy as the initial diagnostic tool is a cost-effective strategy for evaluating indeterminate biliary strictures, especially in settings with higher CCA prevalence or higher baseline utility in the post-diagnosis state.
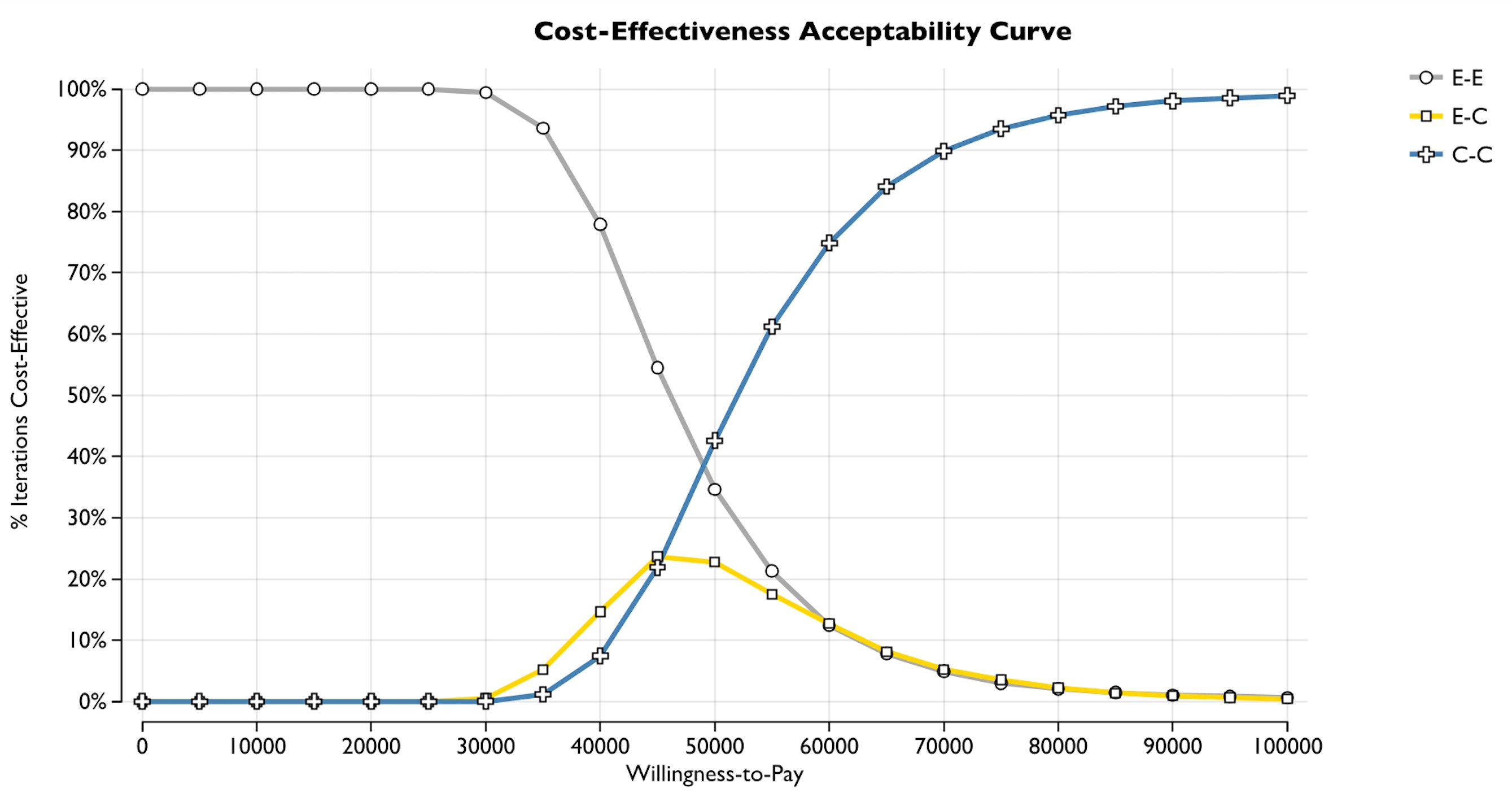
Figure: Figure 1.

Figure: Figure 2.
Disclosures:
Noppachai Siranart indicated no relevant financial relationships.
Patavee Pajareya indicated no relevant financial relationships.
Kittithat Tantitanawat indicated no relevant financial relationships.
Steven Steinway indicated no relevant financial relationships.
Noppachai Siranart, MD1, Patavee Pajareya, MD2, Kittithat Tantitanawat, MD3, Steven Steinway, MD4. P0054 - Cost-Effectiveness of Cholangioscopy-Guided Biopsy as a Primary Diagnostic Tool for Indeterminate Biliary Stricture, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
