Sunday Poster Session
Category: Biliary/Pancreas
P0049 - Clinical Predictors of In-Hospital Mortality in Female Patients With Pancreatic Cancer: Insights From a Nationwide Database
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Cherechi Nwabueze, MBBS, MPH (she/her/hers)
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Cherechi Nwabueze, MBBS, MPH1, Youjin Oh, MD1, Eunice Omeludike, MD2, Favour C. Ezem, MBBS3, Pranav Singh, MBBS1
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Piedmont Athens Regional Medical Centre, Athens, GA; 3University of Nigeria teaching hospital Ituku Ozalla, Lagos, Lagos, Nigeria
Introduction: Pancreatic cancer has high morbidity and mortality, with increasing incidence among women in the US; however, data on the in-hospital outcome remain limited. We aimed to identify predictors of these outcomes to inform clinical management.
Methods: The National Inpatient Sample database from 2016-2020 was utilized to assess demographic and clinical factors associated with in-hospital mortality among females ≥ 18 years with pancreatic cancer. We used multivariable logistic regression to examine patient characteristics and clinical outcome predictors, estimating adjusted odds ratios (aORs) for age, ethnicity, income, insurance, hospital size, region, and teaching status.
Results: 544,864 hospitalized patients had pancreatic cancer, 260,644 (48%) were female (69 ± 0.06 years), 7% (19,288) inpatient deaths. The mean length of stay was 6 days, and mean total adjusted hospital charges were $71,454. Each 1-year increase in age was associated with a 2% higher chance of in-hospital death (aOR 1.02; p < 0.001). Compared to White patients, Black patients had a slightly increased risk of mortality (aOR 1.1; p = 0.1), as did Asians (aOR 1.24; p = 0.002), while Hispanics had significantly lower chance of dying in the hospital (aOR 0.82; p = 0.02). Interestingly, patients with anemia had 24% lower odds of mortality (aOR 0.76; p < 0.001) while those with acute kidney injury (aOR 2.6; p < 0.001), ascites (aOR 2.3; p < 0.001), and hypoglycemia (aOR 2.5; p < 0.001) were more than twice as likely to die during hospitalization. Coagulopathy (aOR 1.6; p < 0.001), and PE (aOR 1.9; p < 0.001) were also strongly linked to death. Those who underwent intubation during hospitalization had a fivefold increase in risk of mortality (aOR 5; p < 0.001). Similarly, mechanical ventilation (aOR 2.7; p < 0.001) and vasopressor use (aOR 2.2; p < 0.001) significantly increased mortality risk. The strongest predictor of death was sepsis, with over a threefold increase in mortality risk (aOR 3.3; p < 0.001).
Discussion: Several clinical and demographic factors were noted to significantly influence in-hospital mortality among females with pancreatic cancer. Sepsis was the most critical complication and intubation the major procedure predicting death. Surprisingly, anemia was associated with lower mortality, warranting further study into understanding this association. These findings highlight the importance of early identification and prompt management of high-risk complications to improve survival outcomes in this population.
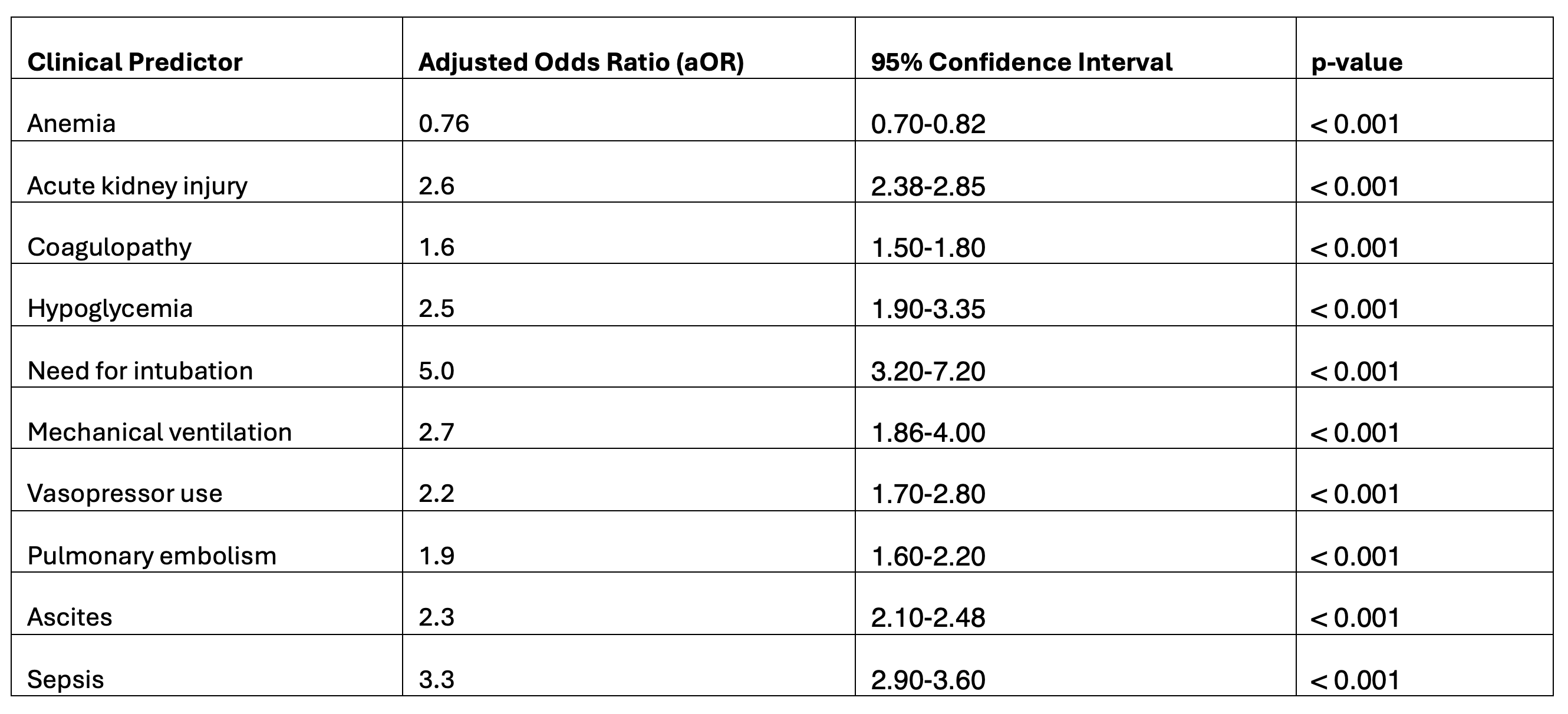
Figure: Table 1. Summary of the clinical Predictors of In-Hospital Mortality in Female Patients with Pancreatic Cancer (Adjusted for age, ethnicity, median household income, insurance type, hospital bed size, geographic region, and teaching status)
Disclosures:
Cherechi Nwabueze indicated no relevant financial relationships.
Youjin Oh indicated no relevant financial relationships.
Eunice Omeludike indicated no relevant financial relationships.
Favour Ezem indicated no relevant financial relationships.
Pranav Singh indicated no relevant financial relationships.
Cherechi Nwabueze, MBBS, MPH1, Youjin Oh, MD1, Eunice Omeludike, MD2, Favour C. Ezem, MBBS3, Pranav Singh, MBBS1. P0049 - Clinical Predictors of In-Hospital Mortality in Female Patients With Pancreatic Cancer: Insights From a Nationwide Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Piedmont Athens Regional Medical Centre, Athens, GA; 3University of Nigeria teaching hospital Ituku Ozalla, Lagos, Lagos, Nigeria
Introduction: Pancreatic cancer has high morbidity and mortality, with increasing incidence among women in the US; however, data on the in-hospital outcome remain limited. We aimed to identify predictors of these outcomes to inform clinical management.
Methods: The National Inpatient Sample database from 2016-2020 was utilized to assess demographic and clinical factors associated with in-hospital mortality among females ≥ 18 years with pancreatic cancer. We used multivariable logistic regression to examine patient characteristics and clinical outcome predictors, estimating adjusted odds ratios (aORs) for age, ethnicity, income, insurance, hospital size, region, and teaching status.
Results: 544,864 hospitalized patients had pancreatic cancer, 260,644 (48%) were female (69 ± 0.06 years), 7% (19,288) inpatient deaths. The mean length of stay was 6 days, and mean total adjusted hospital charges were $71,454. Each 1-year increase in age was associated with a 2% higher chance of in-hospital death (aOR 1.02; p < 0.001). Compared to White patients, Black patients had a slightly increased risk of mortality (aOR 1.1; p = 0.1), as did Asians (aOR 1.24; p = 0.002), while Hispanics had significantly lower chance of dying in the hospital (aOR 0.82; p = 0.02). Interestingly, patients with anemia had 24% lower odds of mortality (aOR 0.76; p < 0.001) while those with acute kidney injury (aOR 2.6; p < 0.001), ascites (aOR 2.3; p < 0.001), and hypoglycemia (aOR 2.5; p < 0.001) were more than twice as likely to die during hospitalization. Coagulopathy (aOR 1.6; p < 0.001), and PE (aOR 1.9; p < 0.001) were also strongly linked to death. Those who underwent intubation during hospitalization had a fivefold increase in risk of mortality (aOR 5; p < 0.001). Similarly, mechanical ventilation (aOR 2.7; p < 0.001) and vasopressor use (aOR 2.2; p < 0.001) significantly increased mortality risk. The strongest predictor of death was sepsis, with over a threefold increase in mortality risk (aOR 3.3; p < 0.001).
Discussion: Several clinical and demographic factors were noted to significantly influence in-hospital mortality among females with pancreatic cancer. Sepsis was the most critical complication and intubation the major procedure predicting death. Surprisingly, anemia was associated with lower mortality, warranting further study into understanding this association. These findings highlight the importance of early identification and prompt management of high-risk complications to improve survival outcomes in this population.
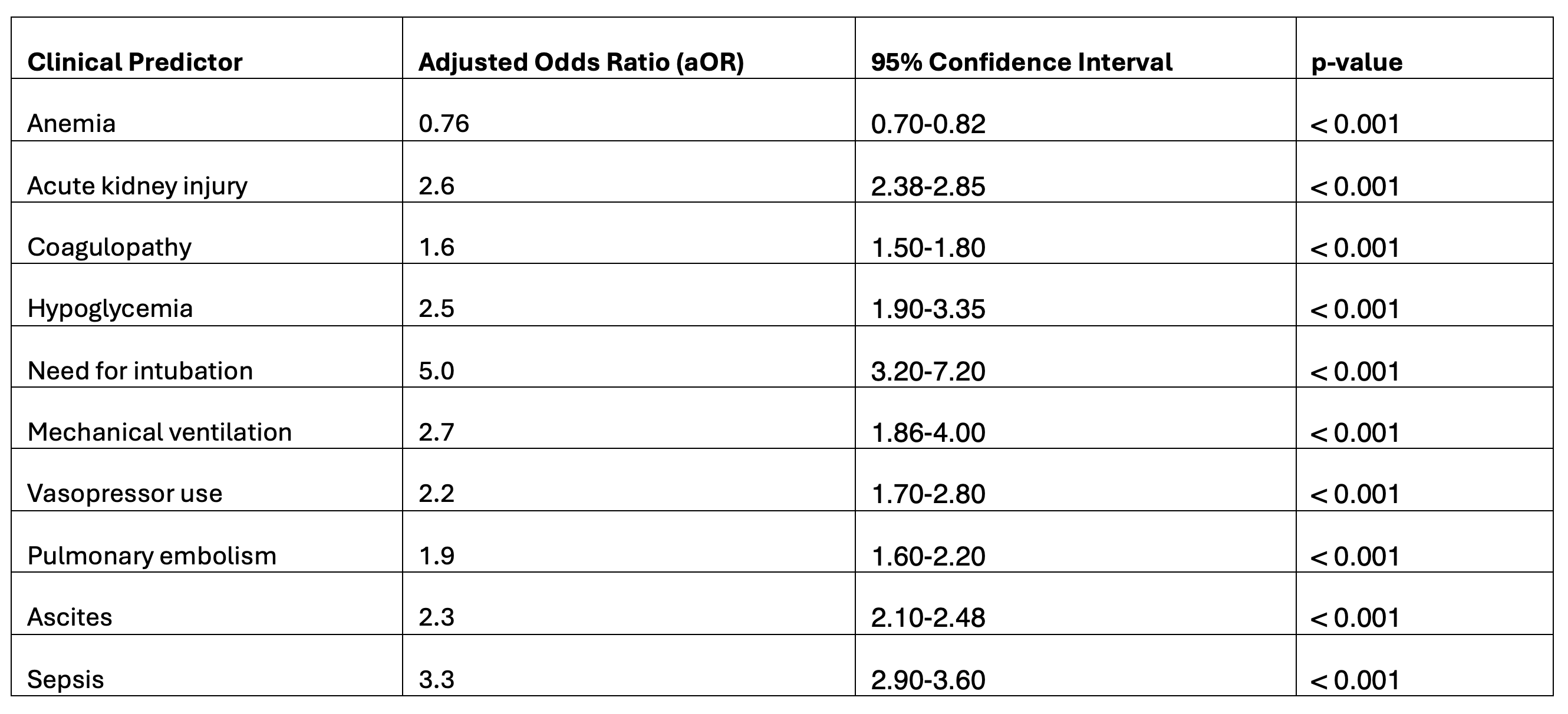
Figure: Table 1. Summary of the clinical Predictors of In-Hospital Mortality in Female Patients with Pancreatic Cancer (Adjusted for age, ethnicity, median household income, insurance type, hospital bed size, geographic region, and teaching status)
Disclosures:
Cherechi Nwabueze indicated no relevant financial relationships.
Youjin Oh indicated no relevant financial relationships.
Eunice Omeludike indicated no relevant financial relationships.
Favour Ezem indicated no relevant financial relationships.
Pranav Singh indicated no relevant financial relationships.
Cherechi Nwabueze, MBBS, MPH1, Youjin Oh, MD1, Eunice Omeludike, MD2, Favour C. Ezem, MBBS3, Pranav Singh, MBBS1. P0049 - Clinical Predictors of In-Hospital Mortality in Female Patients With Pancreatic Cancer: Insights From a Nationwide Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
