Sunday Poster Session
Category: Biliary/Pancreas
P0047 - Long-Term Surveillance of Pancreatic Cystic Lesions: A Systematic Review and Meta-Analysis of Malignant Transformation and High-Risk Progression Beyond 10 Years
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Angel Miro-Gonzalez, MD
University of North Carolina at Chapel Hill School of Medicine
Chapel Hill, NC
Presenting Author(s)
Angel Miro-Gonzalez, MD1, Jay Bapaye, MD2, Shivani Desai, MD1, Jamie Conklin, BS3, Andrew Canakis, DO1
1University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC; 2Virginia Tech Carilion School of Medicine, Roanoke, VA; 3University of North Carolina at Chapel Hill, Chapel Hill, NC
Introduction: The optimal duration of surveillance for pancreatic cystic lesions (PCLs) remains uncertain. Existing guidelines vary in their recommendations, with limited long-term data beyond 10 years. This systematic review and meta-analysis aims to address this gap by providing a summative resource of studies evaluating outcomes of patients undergoing ≥10 years of surveillance for pancreatic cystic lesions without surgical intervention.
Methods: We systematically searched PubMed, Scopus, Embase, and CINAHL from inception through November 2024. Eligible studies included adult patients with intraductal papillary mucinous neoplasms (IPMNs) or mucinous cystic neoplasms (MCNs) under surveillance, with at least some patients followed beyond 10 years. Outcomes of interest were clinically significant progression (development of high-risk stigmata or worrisome features), pancreatic cancer incidence, and pancreatic cancer-related mortality. Pooled proportions were calculated using a random-effects model. Study quality was assessed using the CASP cohort checklist.
Results: Thirty-five studies involving 18,835 PCLs were included. The pooled proportion of clinically significant progression was 8.4% (1,605/16,416; 95% CI, 5.3–13%; I² = 94%). Pancreatic cancer developed in 2.1% of patients (536/18,512; 95% CI, 1.5–2.9%; I² = 86%), and pancreatic cancer-related mortality was 0.9% (95% CI, 0.6–1.4%; I² = 48%). Worrisome features and mural nodules emerged in 11.8% and 3.2% of cysts, respectively. Substantial heterogeneity was observed across most outcomes. Publication bias was present for progression and malignancy estimates.
Discussion: Despite variability in follow-up duration and surveillance practices, a meaningful proportion of cysts developed high-risk features or malignant transformation even after prolonged periods of stability.
Surveillance strategies should be individualized based on cyst features, patient comorbidities, life expectancy, and surgical candidacy. Relying on fixed-duration surveillance alone may lead to missed opportunities for early intervention or overuse of resources in minimal-risk populations. Improved risk stratification tools are needed to guide tailored, evidence-based decision-making in the long-term management of pancreatic cystic lesions.
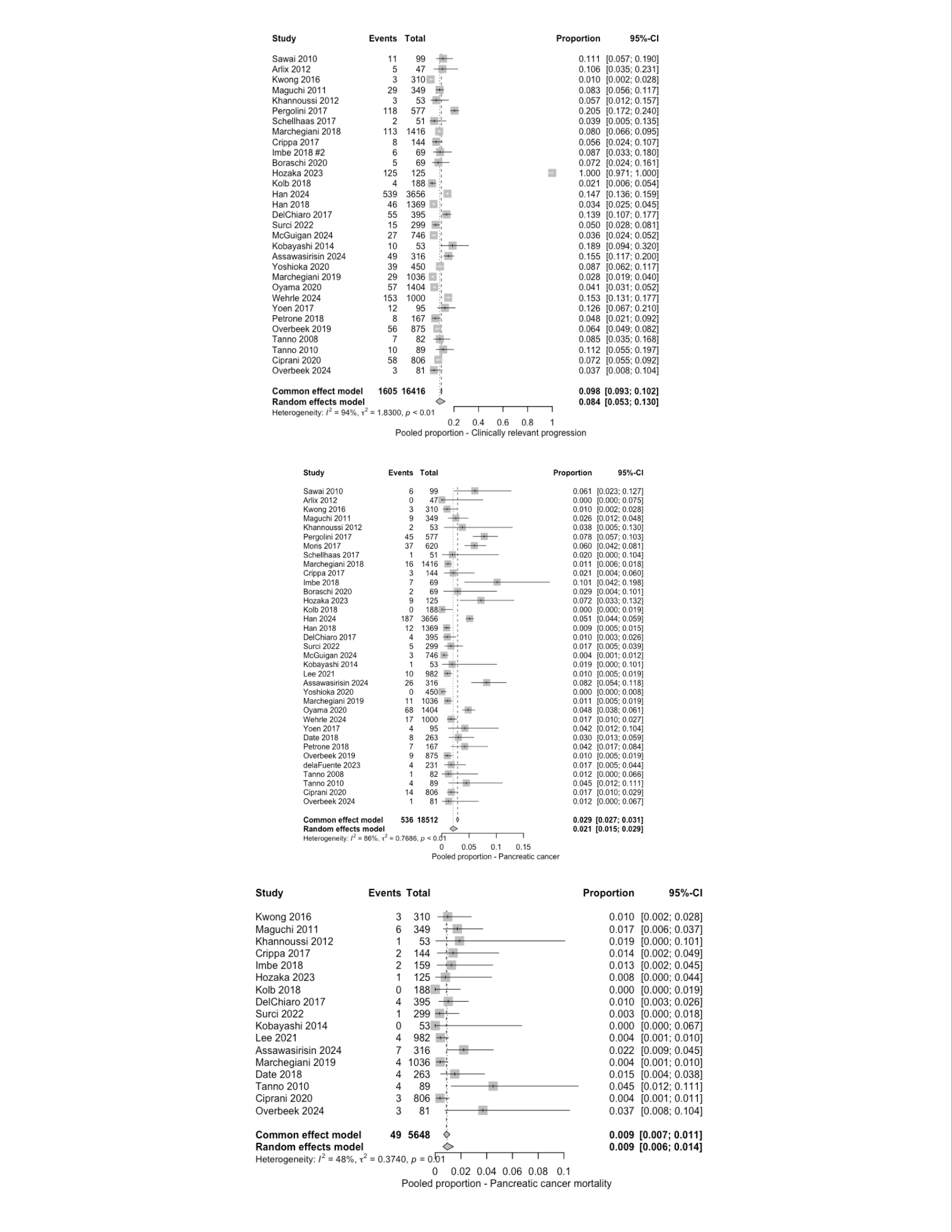
Figure: Table 1. Study characteristics
N/A: Not available from the study.
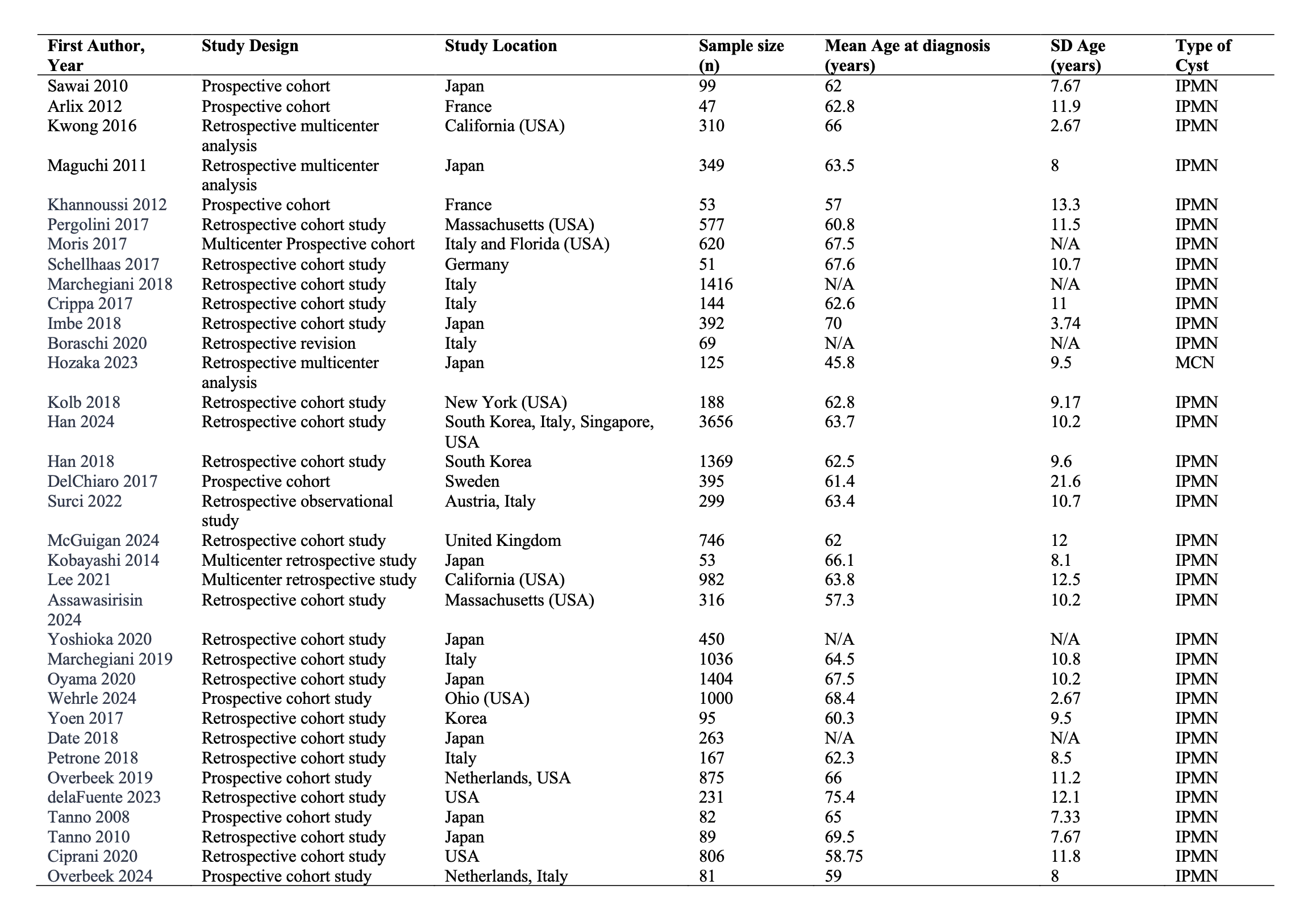
Figure: Figure 1. Pooled proportions of clinically significant progression, pancreatic cancer development, and pancreatic cancer-related mortality of the included studies.
Disclosures:
Angel Miro-Gonzalez indicated no relevant financial relationships.
Jay Bapaye indicated no relevant financial relationships.
Shivani Desai indicated no relevant financial relationships.
Jamie Conklin indicated no relevant financial relationships.
Andrew Canakis indicated no relevant financial relationships.
Angel Miro-Gonzalez, MD1, Jay Bapaye, MD2, Shivani Desai, MD1, Jamie Conklin, BS3, Andrew Canakis, DO1. P0047 - Long-Term Surveillance of Pancreatic Cystic Lesions: A Systematic Review and Meta-Analysis of Malignant Transformation and High-Risk Progression Beyond 10 Years, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC; 2Virginia Tech Carilion School of Medicine, Roanoke, VA; 3University of North Carolina at Chapel Hill, Chapel Hill, NC
Introduction: The optimal duration of surveillance for pancreatic cystic lesions (PCLs) remains uncertain. Existing guidelines vary in their recommendations, with limited long-term data beyond 10 years. This systematic review and meta-analysis aims to address this gap by providing a summative resource of studies evaluating outcomes of patients undergoing ≥10 years of surveillance for pancreatic cystic lesions without surgical intervention.
Methods: We systematically searched PubMed, Scopus, Embase, and CINAHL from inception through November 2024. Eligible studies included adult patients with intraductal papillary mucinous neoplasms (IPMNs) or mucinous cystic neoplasms (MCNs) under surveillance, with at least some patients followed beyond 10 years. Outcomes of interest were clinically significant progression (development of high-risk stigmata or worrisome features), pancreatic cancer incidence, and pancreatic cancer-related mortality. Pooled proportions were calculated using a random-effects model. Study quality was assessed using the CASP cohort checklist.
Results: Thirty-five studies involving 18,835 PCLs were included. The pooled proportion of clinically significant progression was 8.4% (1,605/16,416; 95% CI, 5.3–13%; I² = 94%). Pancreatic cancer developed in 2.1% of patients (536/18,512; 95% CI, 1.5–2.9%; I² = 86%), and pancreatic cancer-related mortality was 0.9% (95% CI, 0.6–1.4%; I² = 48%). Worrisome features and mural nodules emerged in 11.8% and 3.2% of cysts, respectively. Substantial heterogeneity was observed across most outcomes. Publication bias was present for progression and malignancy estimates.
Discussion: Despite variability in follow-up duration and surveillance practices, a meaningful proportion of cysts developed high-risk features or malignant transformation even after prolonged periods of stability.
Surveillance strategies should be individualized based on cyst features, patient comorbidities, life expectancy, and surgical candidacy. Relying on fixed-duration surveillance alone may lead to missed opportunities for early intervention or overuse of resources in minimal-risk populations. Improved risk stratification tools are needed to guide tailored, evidence-based decision-making in the long-term management of pancreatic cystic lesions.
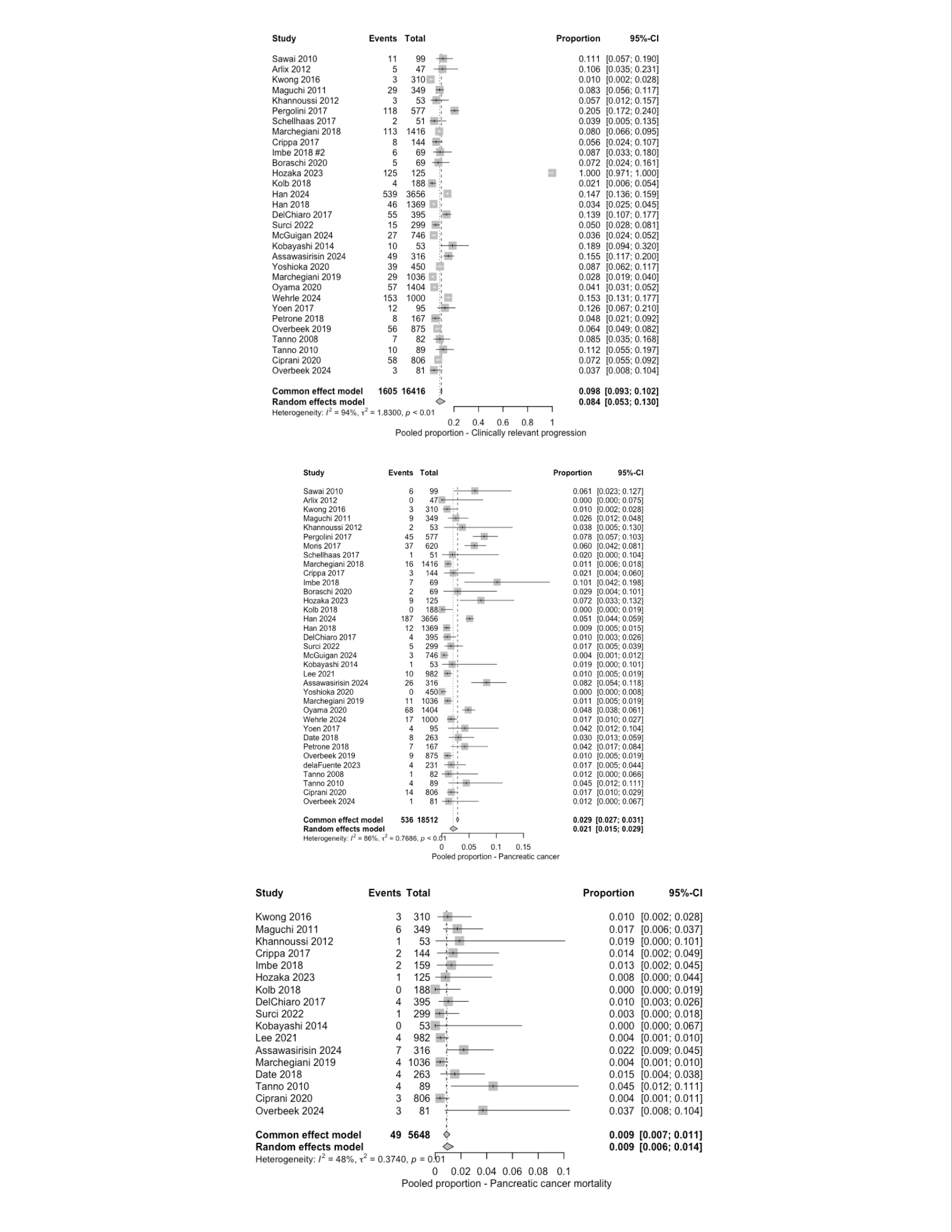
Figure: Table 1. Study characteristics
N/A: Not available from the study.
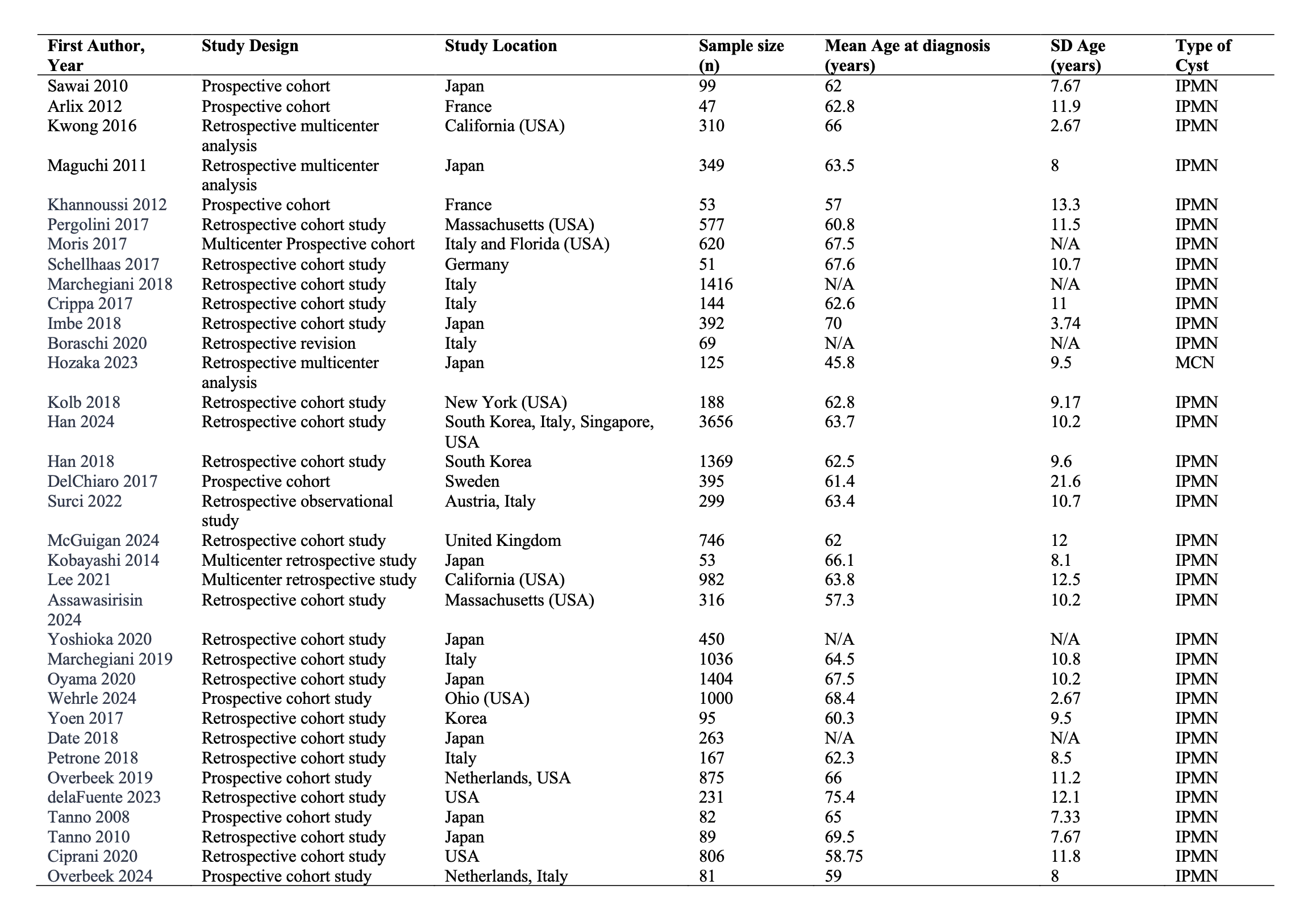
Figure: Figure 1. Pooled proportions of clinically significant progression, pancreatic cancer development, and pancreatic cancer-related mortality of the included studies.
Disclosures:
Angel Miro-Gonzalez indicated no relevant financial relationships.
Jay Bapaye indicated no relevant financial relationships.
Shivani Desai indicated no relevant financial relationships.
Jamie Conklin indicated no relevant financial relationships.
Andrew Canakis indicated no relevant financial relationships.
Angel Miro-Gonzalez, MD1, Jay Bapaye, MD2, Shivani Desai, MD1, Jamie Conklin, BS3, Andrew Canakis, DO1. P0047 - Long-Term Surveillance of Pancreatic Cystic Lesions: A Systematic Review and Meta-Analysis of Malignant Transformation and High-Risk Progression Beyond 10 Years, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

