Sunday Poster Session
Category: Biliary/Pancreas
P0042 - Lactate Levels Don't Lie: A Powerful Predictor in Acute Cholangitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Muhammad Ali Ibrahim Kazi, MD
Anne Arundel Medical Center
Annapolis, MD
Presenting Author(s)
Muhammad Ali Ibrahim Kazi, MD1, Imran Qureshi, MD2, Akshay Sharma, MD1, Nirav Agrawal, MD1, Patel Manthanbhai, MD3, Sanmeet Singh, MD1
1Anne Arundel Medical Center, Annapolis, MD; 2Rutgers New Jersey Medical School, Newark, NJ; 3University of Toledo College of Medicine and Life Sciences, Toledo, OH
Introduction: Acute cholangitis is a life-threatening condition that requires timely diagnosis and intervention. The Tokyo Guidelines serve as the primary framework for diagnosing and grading acute cholangitis, incorporating clinical symptoms, inflammatory markers, and imaging findings. However, lactate levels, a widely recognized biomarker is not included in these criteria. Elevated lactate has been associated with poor outcomes in sepsis and critical illness, yet its role in risk stratification for cholangitis remains unexplored.
In this study, we aim to evaluate the prognostic significance of lactate in patients with cholangitis. By conducting a propensity-matched cohort analysis, we compare outcomes between patients with normal lactate (0-2 mmol/L) and those with elevated lactate (2-12 mmol/L) to determine whether lactate should be integrated into the Tokyo Guidelines for improved risk assessment and clinical decision-making
Methods: This retrospective propensity-matched cohort study evaluated patients diagnosed with cholangitis using ICD-10 codes, stratified into two groups based on lactate levels: 0–2 mmol/L and 2–12 mmol/L. One-to-one matching was performed to minimize confounding, adjusting for demographics (age, sex, race, ethnicity), Charlson Comorbidity Index components (e.g., cardiovascular, pulmonary, hepatic, renal, and oncologic conditions), and clinical variables (albumin levels, fever). Outcomes within one month were compared, including mortality, sepsis/bacteremia, ICU admission, vasopressor use, and interventions such as ERCP, cholecystectomy, and cholecystostomy tube placement.
Results: Patients with elevated Lactate levels had worse outcomes in comparison
Discussion: This propensity-matched analysis demonstrates that elevated lactate levels are a strong predictor of adverse outcomes in cholangitis. Patients with lactate 2-12 mmol/L have significantly higher mortality, sepsis rates, and vasopressor use, yet are less likely to undergo ERCP or cholecystectomy. Given these findings, lactate should be considered for inclusion in the Tokyo Guidelines as a key risk stratification tool. Future prospective studies are warranted to establish optimal lactate thresholds for guiding management decisions in cholangitis.
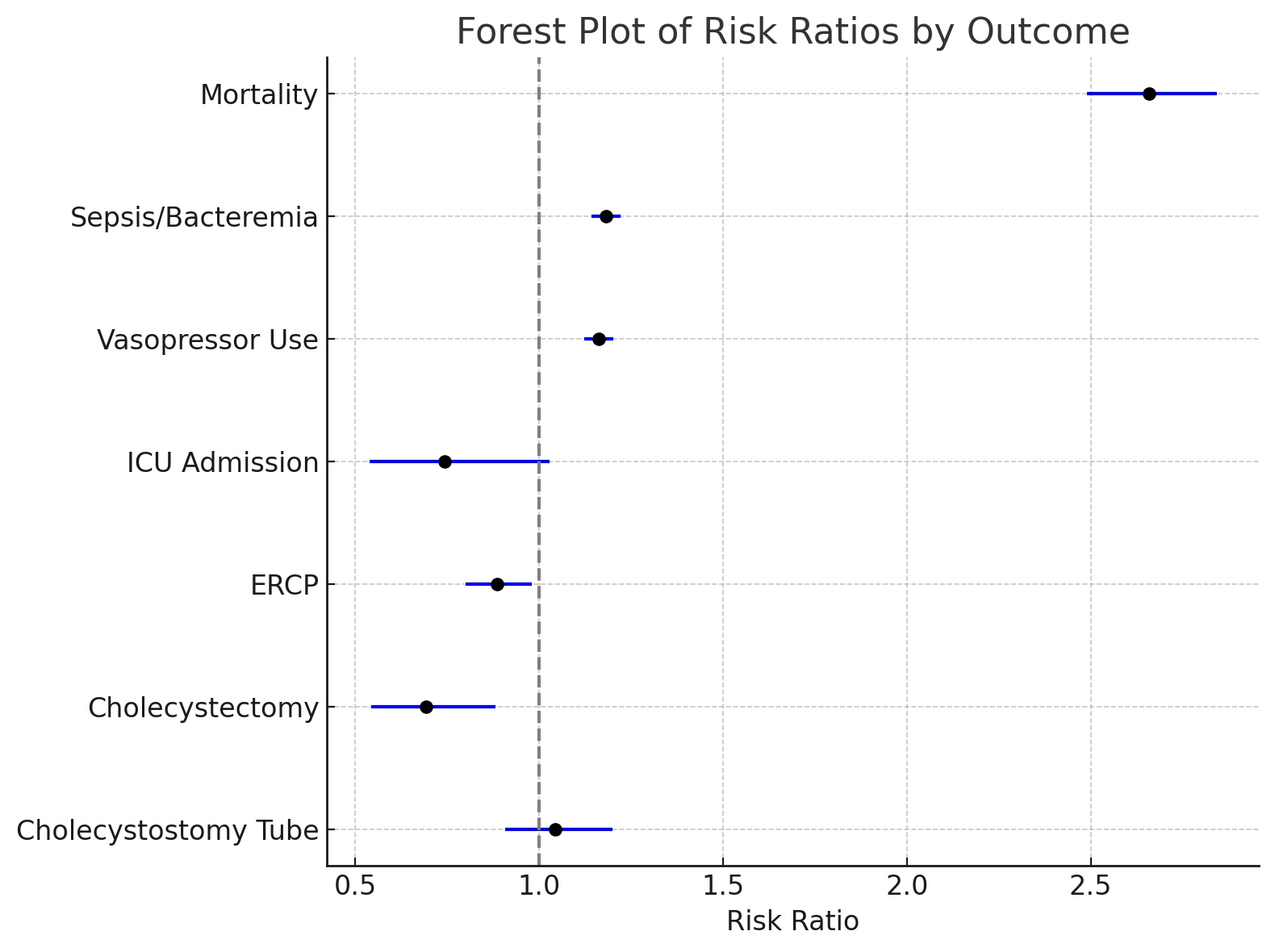
Figure: Figure 1.1
Forrest plot representing the results
Disclosures:
Muhammad Ali Ibrahim Kazi indicated no relevant financial relationships.
Imran Qureshi indicated no relevant financial relationships.
Akshay Sharma indicated no relevant financial relationships.
Nirav Agrawal indicated no relevant financial relationships.
Patel Manthanbhai indicated no relevant financial relationships.
Sanmeet Singh indicated no relevant financial relationships.
Muhammad Ali Ibrahim Kazi, MD1, Imran Qureshi, MD2, Akshay Sharma, MD1, Nirav Agrawal, MD1, Patel Manthanbhai, MD3, Sanmeet Singh, MD1. P0042 - Lactate Levels Don't Lie: A Powerful Predictor in Acute Cholangitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Anne Arundel Medical Center, Annapolis, MD; 2Rutgers New Jersey Medical School, Newark, NJ; 3University of Toledo College of Medicine and Life Sciences, Toledo, OH
Introduction: Acute cholangitis is a life-threatening condition that requires timely diagnosis and intervention. The Tokyo Guidelines serve as the primary framework for diagnosing and grading acute cholangitis, incorporating clinical symptoms, inflammatory markers, and imaging findings. However, lactate levels, a widely recognized biomarker is not included in these criteria. Elevated lactate has been associated with poor outcomes in sepsis and critical illness, yet its role in risk stratification for cholangitis remains unexplored.
In this study, we aim to evaluate the prognostic significance of lactate in patients with cholangitis. By conducting a propensity-matched cohort analysis, we compare outcomes between patients with normal lactate (0-2 mmol/L) and those with elevated lactate (2-12 mmol/L) to determine whether lactate should be integrated into the Tokyo Guidelines for improved risk assessment and clinical decision-making
Methods: This retrospective propensity-matched cohort study evaluated patients diagnosed with cholangitis using ICD-10 codes, stratified into two groups based on lactate levels: 0–2 mmol/L and 2–12 mmol/L. One-to-one matching was performed to minimize confounding, adjusting for demographics (age, sex, race, ethnicity), Charlson Comorbidity Index components (e.g., cardiovascular, pulmonary, hepatic, renal, and oncologic conditions), and clinical variables (albumin levels, fever). Outcomes within one month were compared, including mortality, sepsis/bacteremia, ICU admission, vasopressor use, and interventions such as ERCP, cholecystectomy, and cholecystostomy tube placement.
Results: Patients with elevated Lactate levels had worse outcomes in comparison
Mortality: RR 2.659; p < 0.001
Sepsis/Bacteremia: RR 1.182; p < 0.001
Vasopressor Use: RR 1.162; p < 0.001
ICU Admission: RR 0.744; p = 0.072
ERCP: RR 0.886; p = 0.019
Cholecystectomy: RR 0.692; p = 0.003
Cholecystostomy Tube: RR 1.043; p = 0.559
Discussion: This propensity-matched analysis demonstrates that elevated lactate levels are a strong predictor of adverse outcomes in cholangitis. Patients with lactate 2-12 mmol/L have significantly higher mortality, sepsis rates, and vasopressor use, yet are less likely to undergo ERCP or cholecystectomy. Given these findings, lactate should be considered for inclusion in the Tokyo Guidelines as a key risk stratification tool. Future prospective studies are warranted to establish optimal lactate thresholds for guiding management decisions in cholangitis.
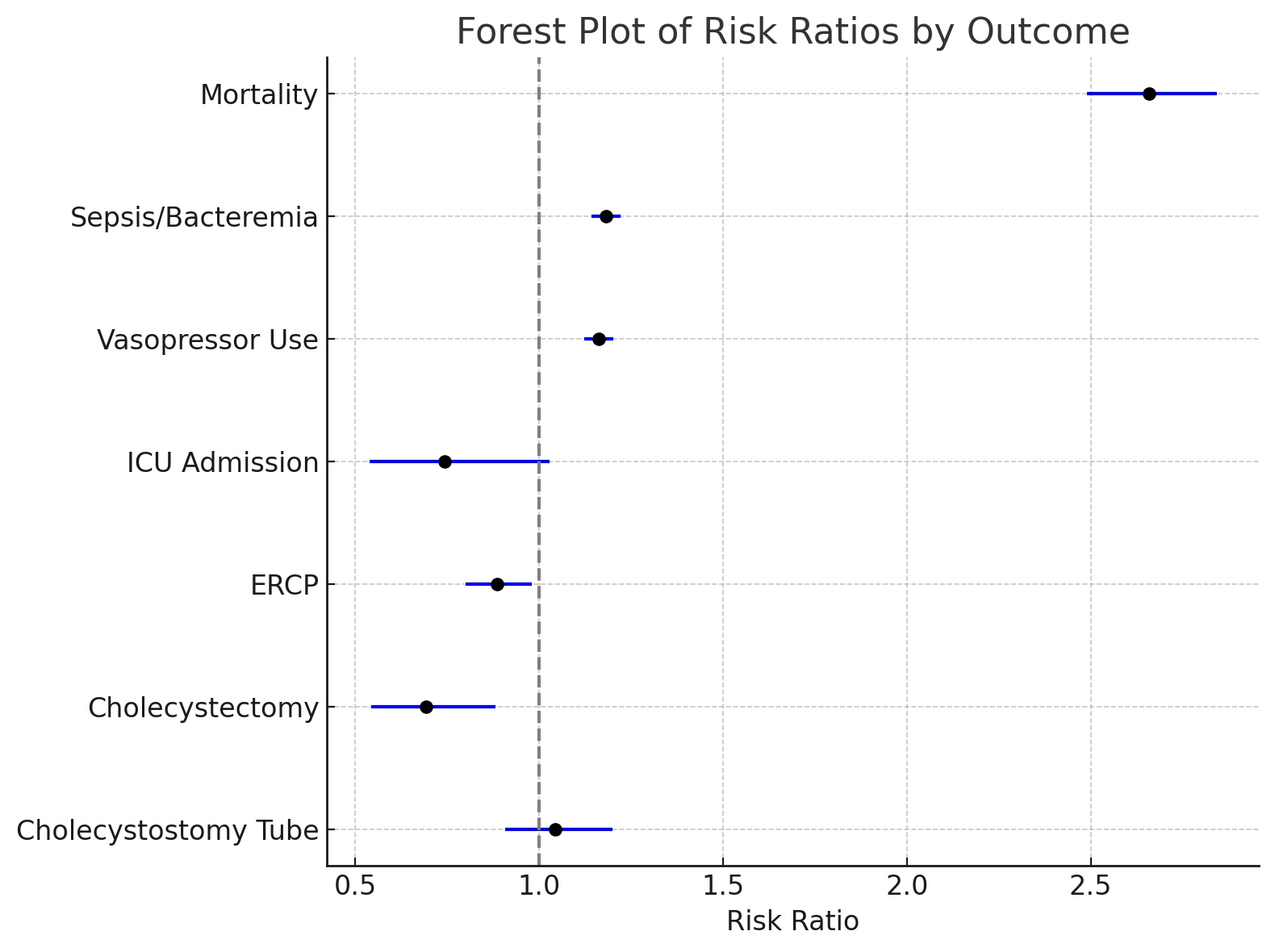
Figure: Figure 1.1
Forrest plot representing the results
Disclosures:
Muhammad Ali Ibrahim Kazi indicated no relevant financial relationships.
Imran Qureshi indicated no relevant financial relationships.
Akshay Sharma indicated no relevant financial relationships.
Nirav Agrawal indicated no relevant financial relationships.
Patel Manthanbhai indicated no relevant financial relationships.
Sanmeet Singh indicated no relevant financial relationships.
Muhammad Ali Ibrahim Kazi, MD1, Imran Qureshi, MD2, Akshay Sharma, MD1, Nirav Agrawal, MD1, Patel Manthanbhai, MD3, Sanmeet Singh, MD1. P0042 - Lactate Levels Don't Lie: A Powerful Predictor in Acute Cholangitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
