Sunday Poster Session
Category: Biliary/Pancreas
P0129 - Fungating Colon Mass, Not Always Cancer: A Case Report of Fistulizing Infected Necrotizing Pancreatitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Samuel Wilcox, MD (he/him/his)
University of Michigan
Ann Arbor, MI
Presenting Author(s)
Samuel Wilcox, MD, Reid Herran, MD, Jeffrey Berinstein, MD, MS
University of Michigan, Ann Arbor, MI
Introduction: Necrotizing pancreatitis is a manifestation of acute pancreatitis and represents one of the criteria for moderately severe disease. Infected necrosis is the leading cause of morbidity and mortality in acute pancreatitis and often occurs 7-10 days following initial presentation.
Case Description/
Methods: A 60-year-old man with an initial hospitalization for gallstone pancreatitis treated with ERCP and cholecystectomy and subsequent admission for an infected necrotizing pancreatic abscess growing Enterobacter cloacae complex and Enterococcus faecium treated with IV vancomycin and piperacillin-sulbactam with transition to levofloxacin and linezolid, presented as an outside hospital transfer for worsening abdominal pain, bloody bowel movements, and hemorrhagic shock. While at the outside hospital, a colonoscopy was performed and demonstrated a fungating, infiltrative, ulcerated and partially obstructing mass in the transverse colon measuring 5 cm in length (Figure 1). Biopsies were taken with cold forceps and were pending at time of transfer but eventually returned with predominantly subepithelial acute and chronic inflammatory exudate with granulation tissue and no identifiable malignancy. CT of the abdomen demonstrated enlarged necrotic collections with proximity to the transverse colon (Figure 2). His course was complicated by recurrence of hemorrhagic shock requiring return to the ICU with IR embolizations of an SMA pseudoaneurysm as well as pancreatic necrosectomy, partial colectomy, and end transverse colostomy. Pathology from the resected transverse colon demonstrated active and chronic inflammation with abscess and granulation tissue involving the outer colonic wall and pericolonic adipose tissue with unremarkable colonic mucosa and no evidence of malignancy.
Discussion: The standard differential diagnosis for a fungating colonic mass includes malignancy versus inflammatory pseudotumor. This case of colonic fistulization represents a rarer, but known, complication of severe necrotizing pancreatitis that can produce a similar appearance on endoscopy. Cases of infected necrotizing pancreatitis involve careful decision making around conservative management versus drainage and necrosectomy. Fistulization of infected necrotizing pancreatitis into nearby structures, including the transverse colon, increases the difficulty of source control and infection management.
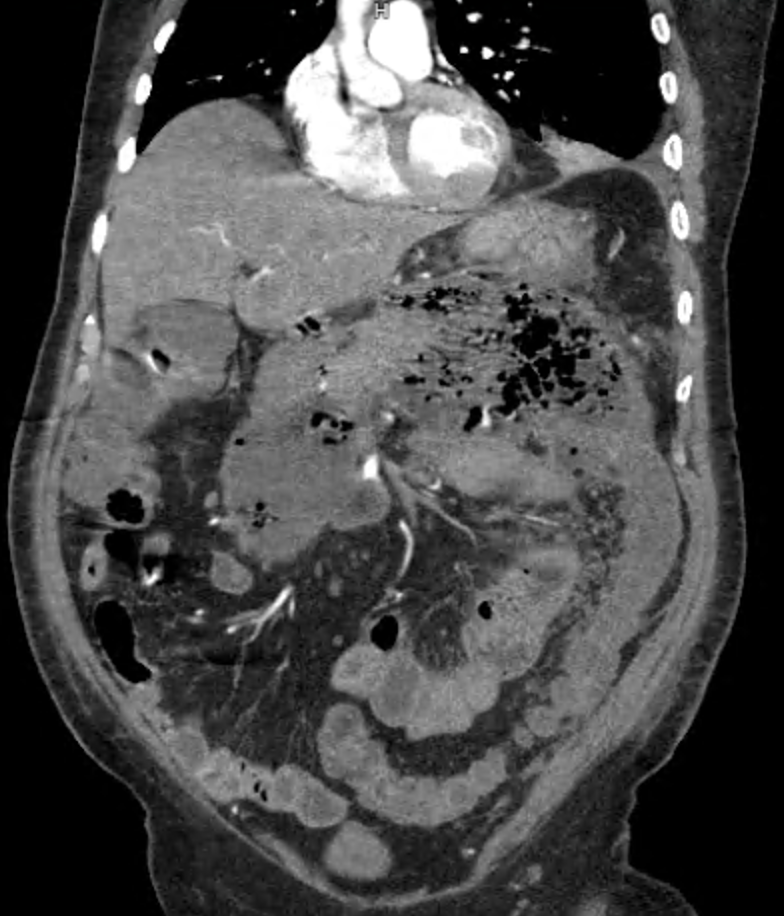
Figure: Figure 1. Fungating mass seen within the transverse colon on colonoscopy.
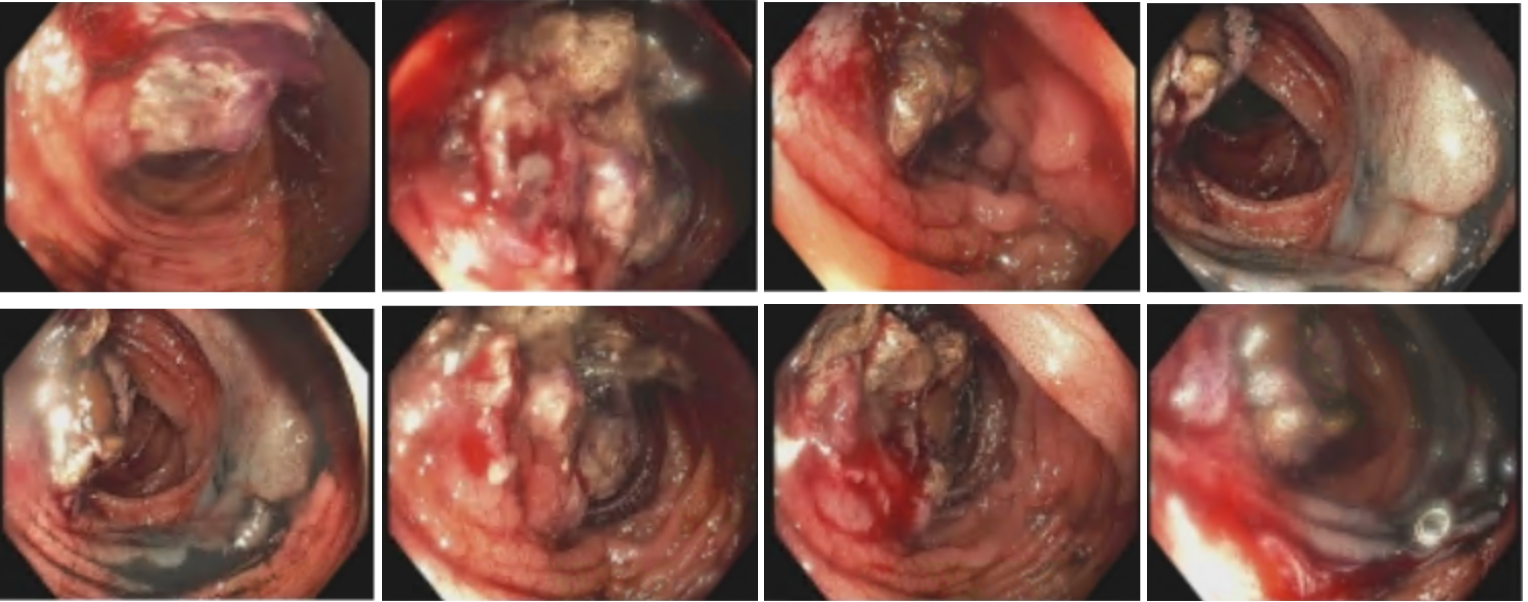
Figure: Figure 2. Severe necrotizing pancreatitis with walled off necrotic collections and involvement of the transverse colon seen on CT imaging.
Disclosures:
Samuel Wilcox indicated no relevant financial relationships.
Reid Herran indicated no relevant financial relationships.
Jeffrey Berinstein indicated no relevant financial relationships.
Samuel Wilcox, MD, Reid Herran, MD, Jeffrey Berinstein, MD, MS. P0129 - Fungating Colon Mass, Not Always Cancer: A Case Report of Fistulizing Infected Necrotizing Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Michigan, Ann Arbor, MI
Introduction: Necrotizing pancreatitis is a manifestation of acute pancreatitis and represents one of the criteria for moderately severe disease. Infected necrosis is the leading cause of morbidity and mortality in acute pancreatitis and often occurs 7-10 days following initial presentation.
Case Description/
Methods: A 60-year-old man with an initial hospitalization for gallstone pancreatitis treated with ERCP and cholecystectomy and subsequent admission for an infected necrotizing pancreatic abscess growing Enterobacter cloacae complex and Enterococcus faecium treated with IV vancomycin and piperacillin-sulbactam with transition to levofloxacin and linezolid, presented as an outside hospital transfer for worsening abdominal pain, bloody bowel movements, and hemorrhagic shock. While at the outside hospital, a colonoscopy was performed and demonstrated a fungating, infiltrative, ulcerated and partially obstructing mass in the transverse colon measuring 5 cm in length (Figure 1). Biopsies were taken with cold forceps and were pending at time of transfer but eventually returned with predominantly subepithelial acute and chronic inflammatory exudate with granulation tissue and no identifiable malignancy. CT of the abdomen demonstrated enlarged necrotic collections with proximity to the transverse colon (Figure 2). His course was complicated by recurrence of hemorrhagic shock requiring return to the ICU with IR embolizations of an SMA pseudoaneurysm as well as pancreatic necrosectomy, partial colectomy, and end transverse colostomy. Pathology from the resected transverse colon demonstrated active and chronic inflammation with abscess and granulation tissue involving the outer colonic wall and pericolonic adipose tissue with unremarkable colonic mucosa and no evidence of malignancy.
Discussion: The standard differential diagnosis for a fungating colonic mass includes malignancy versus inflammatory pseudotumor. This case of colonic fistulization represents a rarer, but known, complication of severe necrotizing pancreatitis that can produce a similar appearance on endoscopy. Cases of infected necrotizing pancreatitis involve careful decision making around conservative management versus drainage and necrosectomy. Fistulization of infected necrotizing pancreatitis into nearby structures, including the transverse colon, increases the difficulty of source control and infection management.
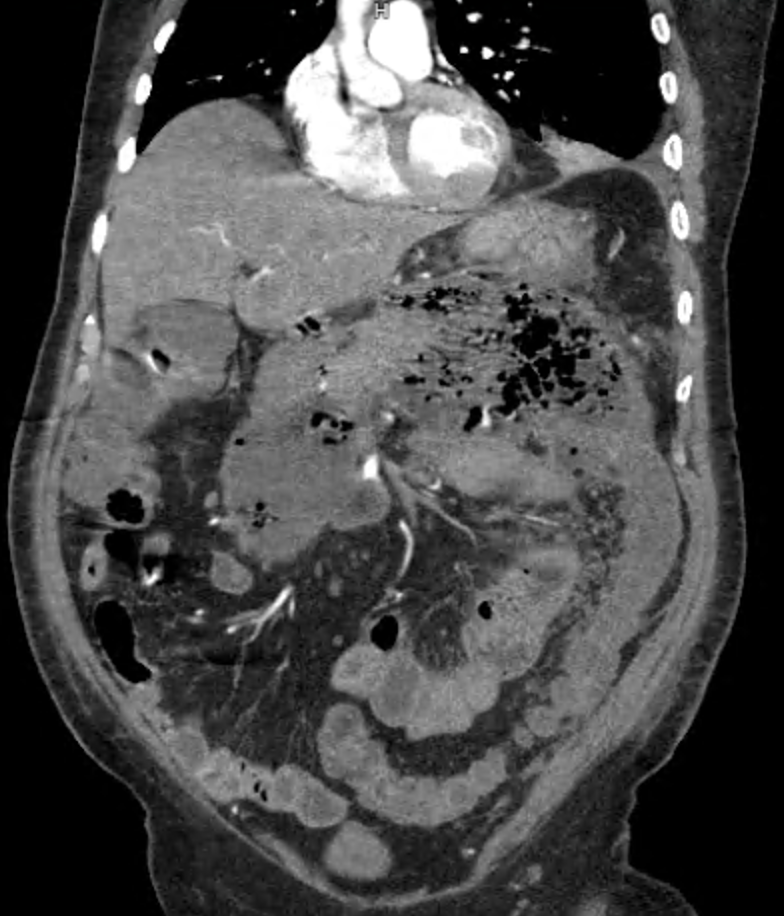
Figure: Figure 1. Fungating mass seen within the transverse colon on colonoscopy.
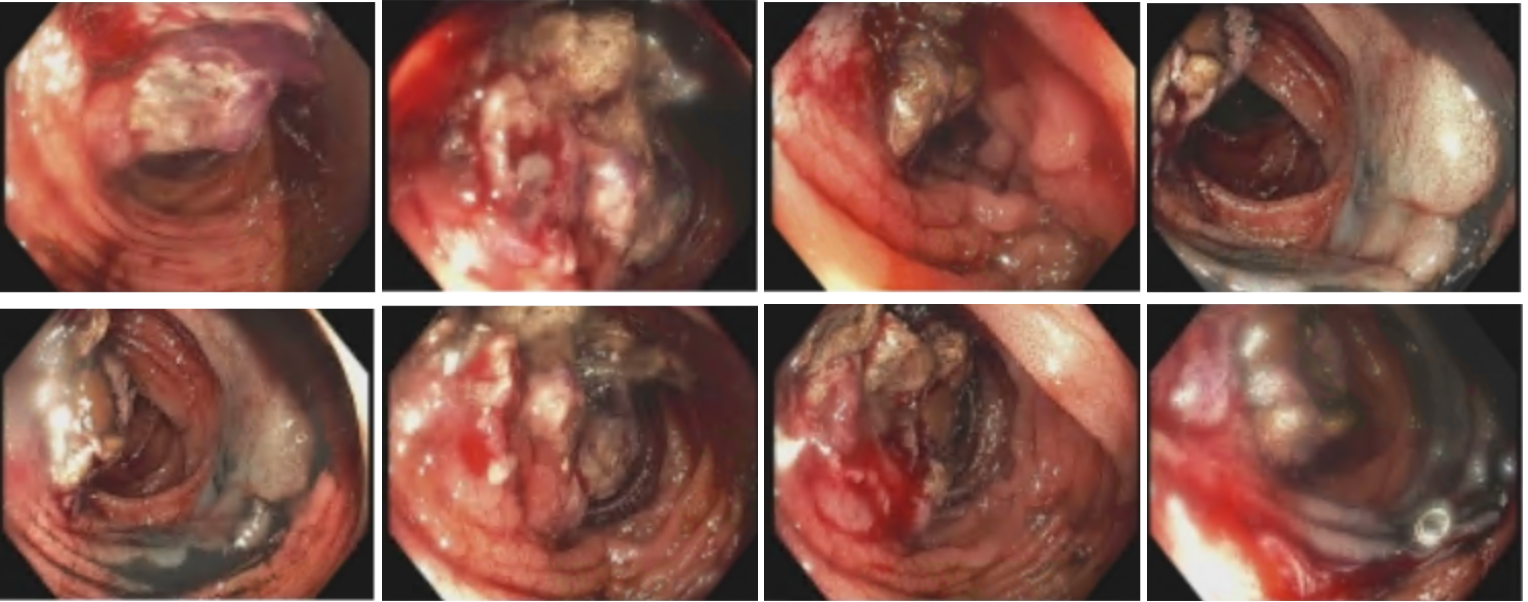
Figure: Figure 2. Severe necrotizing pancreatitis with walled off necrotic collections and involvement of the transverse colon seen on CT imaging.
Disclosures:
Samuel Wilcox indicated no relevant financial relationships.
Reid Herran indicated no relevant financial relationships.
Jeffrey Berinstein indicated no relevant financial relationships.
Samuel Wilcox, MD, Reid Herran, MD, Jeffrey Berinstein, MD, MS. P0129 - Fungating Colon Mass, Not Always Cancer: A Case Report of Fistulizing Infected Necrotizing Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
