Sunday Poster Session
Category: Biliary/Pancreas
P0123 - Primary Budd-Chiari Syndrome: A Silent Threat
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- RX
Risheng Xu, DO (he/him/his)
Baylor College of Medicine
Houston, TX
Presenting Author(s)
Risheng Xu, DO, Joslyn Fisher, MD, Charles Trinh, MD, Sameh Aziz, MD, Shazia Sheikh, MD, Saleem Shamsee, MD
Baylor College of Medicine, Houston, TX
Introduction: Primary Budd-Chiari syndrome (PBCS) is a rare disorder characterized by hepatic venous outflow obstruction due to thrombosis or venous wall disease. Early recognition is crucial due to its high mortality rates. We present a PBCS case caused by essential thrombocythemia with JAK2V617 mutation.
Case Description/
Methods: A 29-year-old female with no medical history presented with progressive abdominal pain and distention over 6 weeks. She denied fever, nausea, vomiting, recent travel, or ill exposure. She had no family history of malignancy, hypercoagulable, or autoimmune disorders and was not on medication. Exam revealed jaundice, abdominal distension, tenderness, shifting dullness, and 2+ pitting edema. Labs: Hgb 14.6 mg/dL, PLT 650 x10^9/L, hepatitis panel negative, Total bilirubin 3.8 mg/dL, AST 71 U/L, ALT 58 U/L. CT showed caudate lobe enlargement, obliteration of the hepatic veins, severe compression of the intrahepatic inferior-vena-cava (IVC), ascites, and portal hypertension. MRI confirmed CT finding. Paracentesis showed no infection/malignancy. Trans-jugular liver biopsy indicated PBCS with chronic hepatic vein occlusion and intrahepatic IVC narrowing. Hypercoagulation evaluation revealed JAK2V617 mutation, diagnosing essential thrombocythemia. Due to her liver anatomy, she is not a candidate for TIPS procedure, and she was scheduled for outpatient routine paracentesis and listed for liver transplant and discharged with spironolactone, furosemide, enoxaparin, aspirin, and hydroxyurea.
Discussion: PBCS is extremely rare, ~ 1 case per million per year, more common in women 30-40s. About 75% of PBCS patients have a hypercoagulable state, with chronic myeloproliferative disorders causing up to 50% of cases. The JAK2V617 mutation is particularly significant in PBCS as it leads to uncontrolled blood cell production, increasing the risk of thrombosis. Chronic obstruction of hepatic venous outflow leads eventually cirrhosis. Symptoms vary with obstruction severity and rapidity. Doppler ultrasonography is preferred for initial investigation, with CT/MRI confirming diagnosis and aiding treatment planning. The importance of our case is early recognition and treatment are key, as 90% die in 3 years without treatment, and if treated early, survival at 5 years is 74%. Treatment aims to prevent clot propagation, restore vein patency, decompress the liver, and prevent complications, including anticoagulation, managing portal hypertension, thrombolysis, angioplasty/stenting, and liver transplantation.
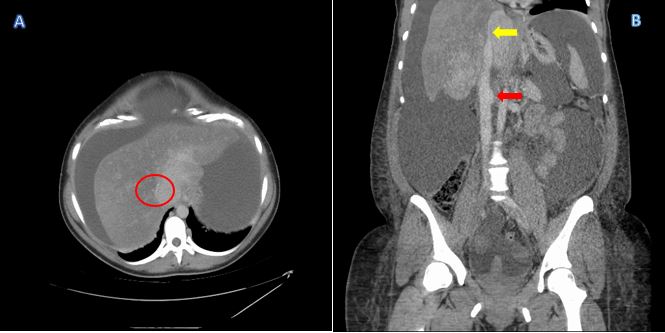
Figure: Figure 1. Findings on axial CT abdomen/pelvis include: (A) Compression of the intrahepatic inferior vena cava (IVC), as indicated by the red circle. (B) Tapering/compression of the intrahepatic IVC (yellow arrow) and engorgement of the distal IVC (red arrow)
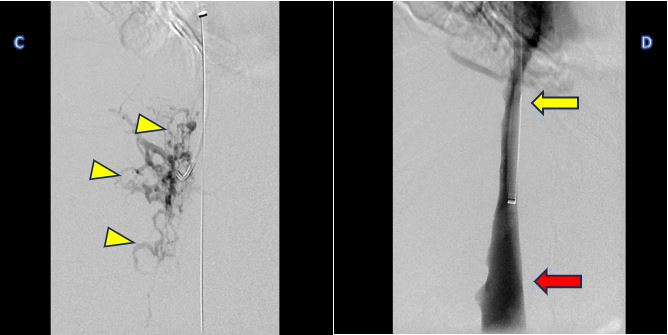
Figure: Figure 2. Trans-jugular biopsy with fluoroscopy. (C) Showing multiple collaterals from chronic hepatic vein occlusion. (D) Yellow arrow showing intrahepatic IVC narrowing and red arrow showing engorgement corresponding to the CT images.
Disclosures:
Risheng Xu indicated no relevant financial relationships.
Joslyn Fisher indicated no relevant financial relationships.
Charles Trinh indicated no relevant financial relationships.
Sameh Aziz indicated no relevant financial relationships.
Shazia Sheikh indicated no relevant financial relationships.
Saleem Shamsee indicated no relevant financial relationships.
Risheng Xu, DO, Joslyn Fisher, MD, Charles Trinh, MD, Sameh Aziz, MD, Shazia Sheikh, MD, Saleem Shamsee, MD. P0123 - Primary Budd-Chiari Syndrome: A Silent Threat, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Baylor College of Medicine, Houston, TX
Introduction: Primary Budd-Chiari syndrome (PBCS) is a rare disorder characterized by hepatic venous outflow obstruction due to thrombosis or venous wall disease. Early recognition is crucial due to its high mortality rates. We present a PBCS case caused by essential thrombocythemia with JAK2V617 mutation.
Case Description/
Methods: A 29-year-old female with no medical history presented with progressive abdominal pain and distention over 6 weeks. She denied fever, nausea, vomiting, recent travel, or ill exposure. She had no family history of malignancy, hypercoagulable, or autoimmune disorders and was not on medication. Exam revealed jaundice, abdominal distension, tenderness, shifting dullness, and 2+ pitting edema. Labs: Hgb 14.6 mg/dL, PLT 650 x10^9/L, hepatitis panel negative, Total bilirubin 3.8 mg/dL, AST 71 U/L, ALT 58 U/L. CT showed caudate lobe enlargement, obliteration of the hepatic veins, severe compression of the intrahepatic inferior-vena-cava (IVC), ascites, and portal hypertension. MRI confirmed CT finding. Paracentesis showed no infection/malignancy. Trans-jugular liver biopsy indicated PBCS with chronic hepatic vein occlusion and intrahepatic IVC narrowing. Hypercoagulation evaluation revealed JAK2V617 mutation, diagnosing essential thrombocythemia. Due to her liver anatomy, she is not a candidate for TIPS procedure, and she was scheduled for outpatient routine paracentesis and listed for liver transplant and discharged with spironolactone, furosemide, enoxaparin, aspirin, and hydroxyurea.
Discussion: PBCS is extremely rare, ~ 1 case per million per year, more common in women 30-40s. About 75% of PBCS patients have a hypercoagulable state, with chronic myeloproliferative disorders causing up to 50% of cases. The JAK2V617 mutation is particularly significant in PBCS as it leads to uncontrolled blood cell production, increasing the risk of thrombosis. Chronic obstruction of hepatic venous outflow leads eventually cirrhosis. Symptoms vary with obstruction severity and rapidity. Doppler ultrasonography is preferred for initial investigation, with CT/MRI confirming diagnosis and aiding treatment planning. The importance of our case is early recognition and treatment are key, as 90% die in 3 years without treatment, and if treated early, survival at 5 years is 74%. Treatment aims to prevent clot propagation, restore vein patency, decompress the liver, and prevent complications, including anticoagulation, managing portal hypertension, thrombolysis, angioplasty/stenting, and liver transplantation.
Figure: Figure 1. Findings on axial CT abdomen/pelvis include: (A) Compression of the intrahepatic inferior vena cava (IVC), as indicated by the red circle. (B) Tapering/compression of the intrahepatic IVC (yellow arrow) and engorgement of the distal IVC (red arrow)
Figure: Figure 2. Trans-jugular biopsy with fluoroscopy. (C) Showing multiple collaterals from chronic hepatic vein occlusion. (D) Yellow arrow showing intrahepatic IVC narrowing and red arrow showing engorgement corresponding to the CT images.
Disclosures:
Risheng Xu indicated no relevant financial relationships.
Joslyn Fisher indicated no relevant financial relationships.
Charles Trinh indicated no relevant financial relationships.
Sameh Aziz indicated no relevant financial relationships.
Shazia Sheikh indicated no relevant financial relationships.
Saleem Shamsee indicated no relevant financial relationships.
Risheng Xu, DO, Joslyn Fisher, MD, Charles Trinh, MD, Sameh Aziz, MD, Shazia Sheikh, MD, Saleem Shamsee, MD. P0123 - Primary Budd-Chiari Syndrome: A Silent Threat, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
