Sunday Poster Session
Category: Biliary/Pancreas
P0220 - EUS-Guided Rendezvous for Pancreas Divisum in SPINK1-Related Hereditary Pancreatitis: A Complex Endoscopic Intervention
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Guneet Sidhu, MD
University of North Dakota, School of Medicine and Health Sciences
Fargo, ND
Presenting Author(s)
Award: ACG Presidential Poster Award
Guneet Sidhu, MD1, Ross Meidinger, MD2
1University of North Dakota, School of Medicine and Health Sciences, Fargo, ND; 2Sanford Health, Fargo, ND
Introduction: Pancreas divisum, a congenital anomaly resulting from the failure of fusion between the dorsal and ventral pancreatic ducts, is often asymptomatic but can predispose individuals to recurrent pancreatitis. In patients with genetic predispositions, such as SPINK1 mutations, the risk of pancreatitis increases. ERCP is a standard therapeutic approach; however, anatomical variations can pose significant challenges. The endoscopic ultrasound (EUS)-guided rendezvous technique has emerged as a valuable alternative
Case Description/
Methods: 42Y F with a history of SPINK1-related hereditary pancreatitis presented with acute abdominal pain. Imaging revealed a prominent main pancreatic duct measuring 5 mm and evidence of pancreas divisum. EUS demonstrated a heterogeneous pancreas with hyperechoic foci and strands, along with postobstructive inflammatory changes and ductal dilation. ERCP was attempted, but cannulation of the minor papilla was unsuccessful despite the use of a Jagtome, guidewire, and needle-knife precut. Subsequently, an EUS-guided FNA was performed through the gastric wall into the pancreatic duct, and contrast injection revealed a 5–6 mm stricture in the dorsal duct with a santorinicele at the minor papilla. A 0.018-inch guidewire was advanced through the FNA needle into the duodenum. Due to difficulties in removing the FNA needle over the guidewire, a wire cutter was used to sever the needle below the hub, and forceps were employed to push the guidewire and needle through the endoscope's working channel while withdrawing the scope, maintaining guidewire access. The ERCP scope was reintroduced, and the rendezvous wire was visualized exiting the minor papilla. Using the Jagtome and a 0.025-inch guidewire, successful cannulation of the minor papilla was achieved. A 2 mm minor papillotomy was performed, and a 5 Fr × 7 cm pancreatic stent with an internal flange and external pigtail was placed through the minor papilla.
Discussion: This case underscores the complexities involved in managing pancreas divisum, particularly in patients with hereditary pancreatitis due to SPINK1 mutations. Traditional ERCP approaches may be hindered by anatomical variations, necessitating alternative techniques. The EUS-guided rendezvous method provided a viable solution for pancreatic duct access when standard cannulation methods failed. The innovative approach of cutting the FNA needle and maintaining guidewire access exemplifies the adaptability required in complex endoscopic procedures.
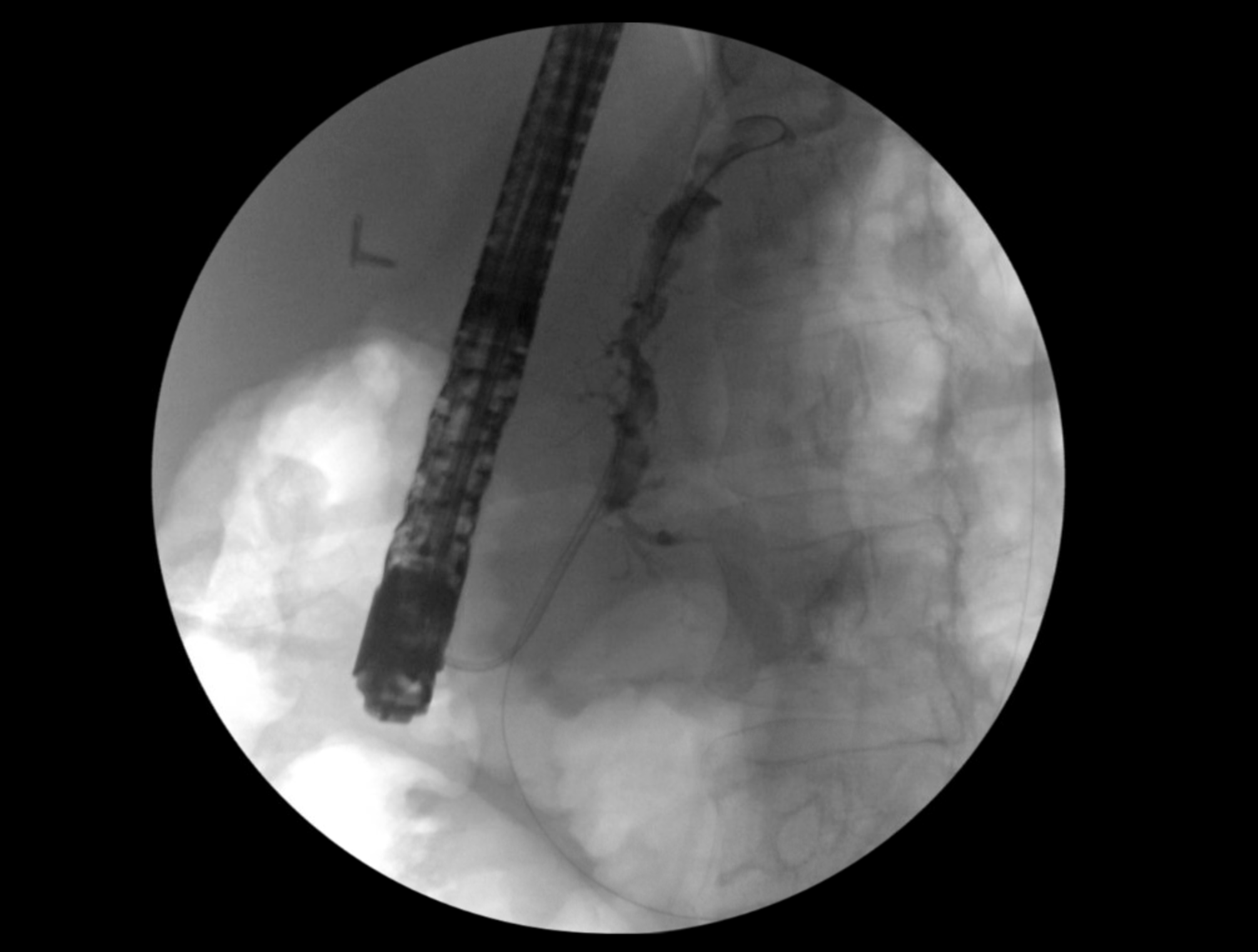
Figure: FNA needle was punctured through the gastric wall into the pancreatic duct in the body. A 0.018 guidewire was advanced through the FNA needle into the pancreatic duct and advanced into the duodenum.
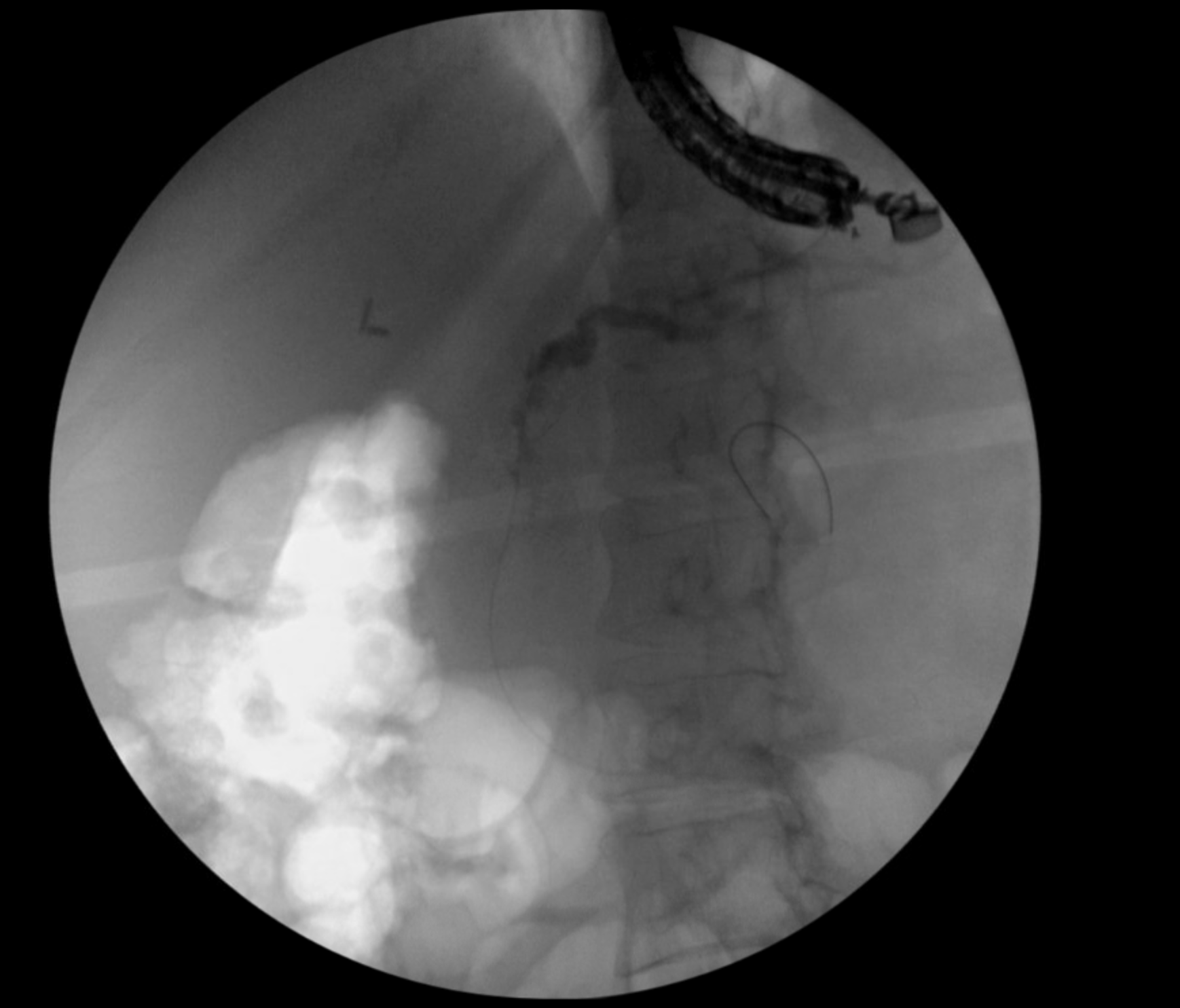
Figure: The rendezvous wire could be seen exiting the minor papilla in the second portion of the duodenum
Disclosures:
Guneet Sidhu indicated no relevant financial relationships.
Ross Meidinger indicated no relevant financial relationships.
Guneet Sidhu, MD1, Ross Meidinger, MD2. P0220 - EUS-Guided Rendezvous for Pancreas Divisum in SPINK1-Related Hereditary Pancreatitis: A Complex Endoscopic Intervention, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Guneet Sidhu, MD1, Ross Meidinger, MD2
1University of North Dakota, School of Medicine and Health Sciences, Fargo, ND; 2Sanford Health, Fargo, ND
Introduction: Pancreas divisum, a congenital anomaly resulting from the failure of fusion between the dorsal and ventral pancreatic ducts, is often asymptomatic but can predispose individuals to recurrent pancreatitis. In patients with genetic predispositions, such as SPINK1 mutations, the risk of pancreatitis increases. ERCP is a standard therapeutic approach; however, anatomical variations can pose significant challenges. The endoscopic ultrasound (EUS)-guided rendezvous technique has emerged as a valuable alternative
Case Description/
Methods: 42Y F with a history of SPINK1-related hereditary pancreatitis presented with acute abdominal pain. Imaging revealed a prominent main pancreatic duct measuring 5 mm and evidence of pancreas divisum. EUS demonstrated a heterogeneous pancreas with hyperechoic foci and strands, along with postobstructive inflammatory changes and ductal dilation. ERCP was attempted, but cannulation of the minor papilla was unsuccessful despite the use of a Jagtome, guidewire, and needle-knife precut. Subsequently, an EUS-guided FNA was performed through the gastric wall into the pancreatic duct, and contrast injection revealed a 5–6 mm stricture in the dorsal duct with a santorinicele at the minor papilla. A 0.018-inch guidewire was advanced through the FNA needle into the duodenum. Due to difficulties in removing the FNA needle over the guidewire, a wire cutter was used to sever the needle below the hub, and forceps were employed to push the guidewire and needle through the endoscope's working channel while withdrawing the scope, maintaining guidewire access. The ERCP scope was reintroduced, and the rendezvous wire was visualized exiting the minor papilla. Using the Jagtome and a 0.025-inch guidewire, successful cannulation of the minor papilla was achieved. A 2 mm minor papillotomy was performed, and a 5 Fr × 7 cm pancreatic stent with an internal flange and external pigtail was placed through the minor papilla.
Discussion: This case underscores the complexities involved in managing pancreas divisum, particularly in patients with hereditary pancreatitis due to SPINK1 mutations. Traditional ERCP approaches may be hindered by anatomical variations, necessitating alternative techniques. The EUS-guided rendezvous method provided a viable solution for pancreatic duct access when standard cannulation methods failed. The innovative approach of cutting the FNA needle and maintaining guidewire access exemplifies the adaptability required in complex endoscopic procedures.
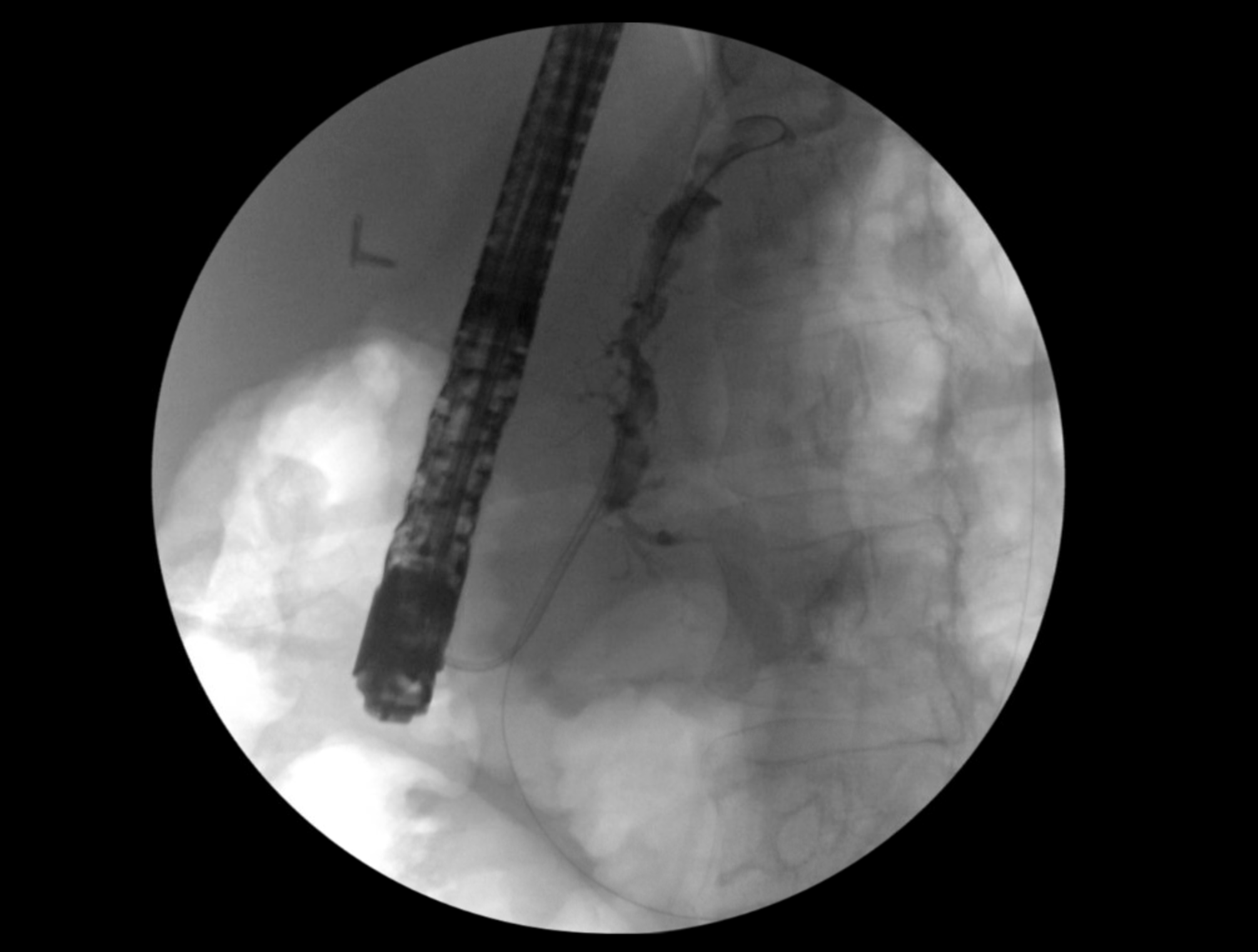
Figure: FNA needle was punctured through the gastric wall into the pancreatic duct in the body. A 0.018 guidewire was advanced through the FNA needle into the pancreatic duct and advanced into the duodenum.
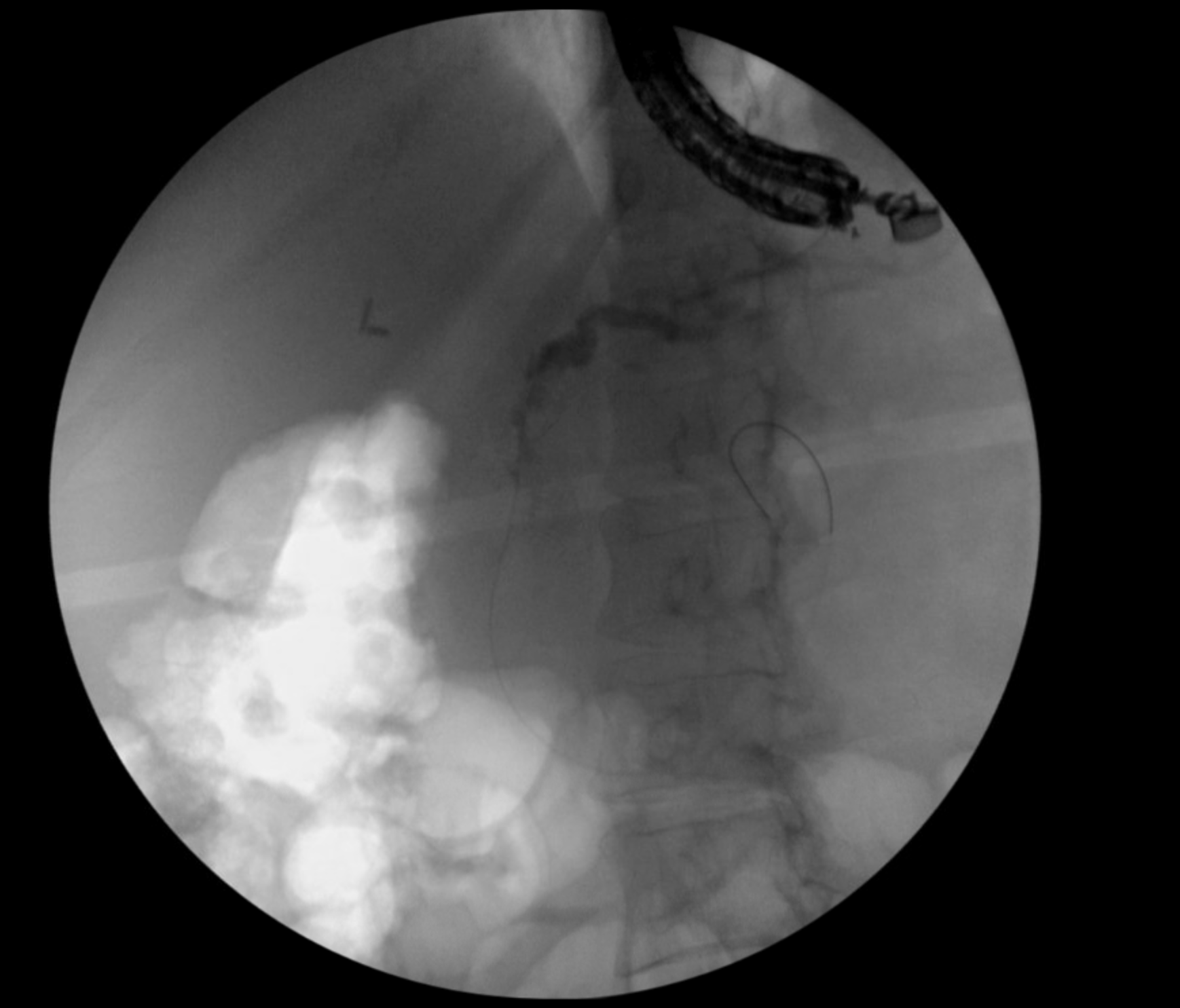
Figure: The rendezvous wire could be seen exiting the minor papilla in the second portion of the duodenum
Disclosures:
Guneet Sidhu indicated no relevant financial relationships.
Ross Meidinger indicated no relevant financial relationships.
Guneet Sidhu, MD1, Ross Meidinger, MD2. P0220 - EUS-Guided Rendezvous for Pancreas Divisum in SPINK1-Related Hereditary Pancreatitis: A Complex Endoscopic Intervention, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

