Sunday Poster Session
Category: Biliary/Pancreas
P0215 - From Drainage to Dilemma: A Complex Journey Through Pancreatic Pseudocyst Fistulization, Necrosis, and Duodenal Stenosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Varshita Goduguchinta, DO (she/her/hers)
Franciscan Health
Olympia Fields, IL
Presenting Author(s)
Varshita Goduguchinta, DO1, Komlan Guedze, MD1, Hardeep Ahdi, MD1, Raahi Patel, DO2, Zohair Ahmed, MD1, Mohammad Arfeen, DO3
1Franciscan Health, Olympia Fields, IL; 2Franciscan Health Olympia Fields, Olympia Fields, IL; 3Franciscan Health, Michigan City, IN
Introduction: Pancreatic pseudocysts are common sequelae of acute or chronic pancreatitis, occurring in up to 40% of cases. Endoscopic ultrasound (EUS)-guided cystogastrostomy using lumen-apposing metal stents (LAMS) has emerged as a minimally invasive, effective technique for symptomatic or infected collections. We describe a rare case of pancreatico-duodenal and pancreatico-colonic fistulization following EUS-guided drainage of walled-off pancreatic necrosis (WON).
Case Description/
Methods: A 59-year-old male with a history of type 2 diabetes mellitus, hypertriglyceridemia, non-alcoholic fatty liver disease, and prior pancreatitis presented with two months of epigastric pain, nausea, vomiting, and unintentional weight loss of 10 kilograms. MRI of the abdomen showed a complex fluid collection measuring 19.7 x 6.3 x 6.6 cm in the pancreatic body and tail, consistent with a pseudocyst. Upper endoscopy revealed a gastric phytobezoar and acquired duodenal stenosis. EUS-guided cystogastrostomy was performed using a 20 x 10 mm LAMS, dilated to 16.5 mm, with a 10 Fr x 4 cm double pigtail stent placed for internal drainage. Purulent material was observed, and the patient was discharged on empiric antibiotics. The patient was readmitted several days later with watery diarrhea and diffuse abdominal pain. Laboratory results showed leukocytosis, hyponatremia, hypokalemia, and elevated fecal elastase. CT revealed a reduction in the size of the collection to 9.1 x 2.4 cm with persistent multiloculated components and pancreatic head edema. Repeat endoscopy showed retained necrotic debris and a duodenal fistula, prompting endoscopic necrosectomy. Colonoscopy identified extrinsic stenosis in the splenic flexure. Follow-up imaging confirmed fistulous tracts between the peripancreatic collection and both the duodenum and colon. Serial imaging later demonstrated resolution of the collection. The stents were removed, and the patient showed clinical improvement with weight gain and symptom resolution.
Discussion: Pancreatico-enteric fistulization is a rare (3–10%) but serious complication of pancreatic pseudocysts and WON. This case illustrates the potential for fistula formation even with appropriate EUS-guided drainage and underscores the need for close monitoring. Endoscopic therapy remains a viable and effective strategy for managing such complex cases.

Figure: Axial CT of Abdomen and Pelvis with contrast highlighting fistula from the pancreatic fluid collection
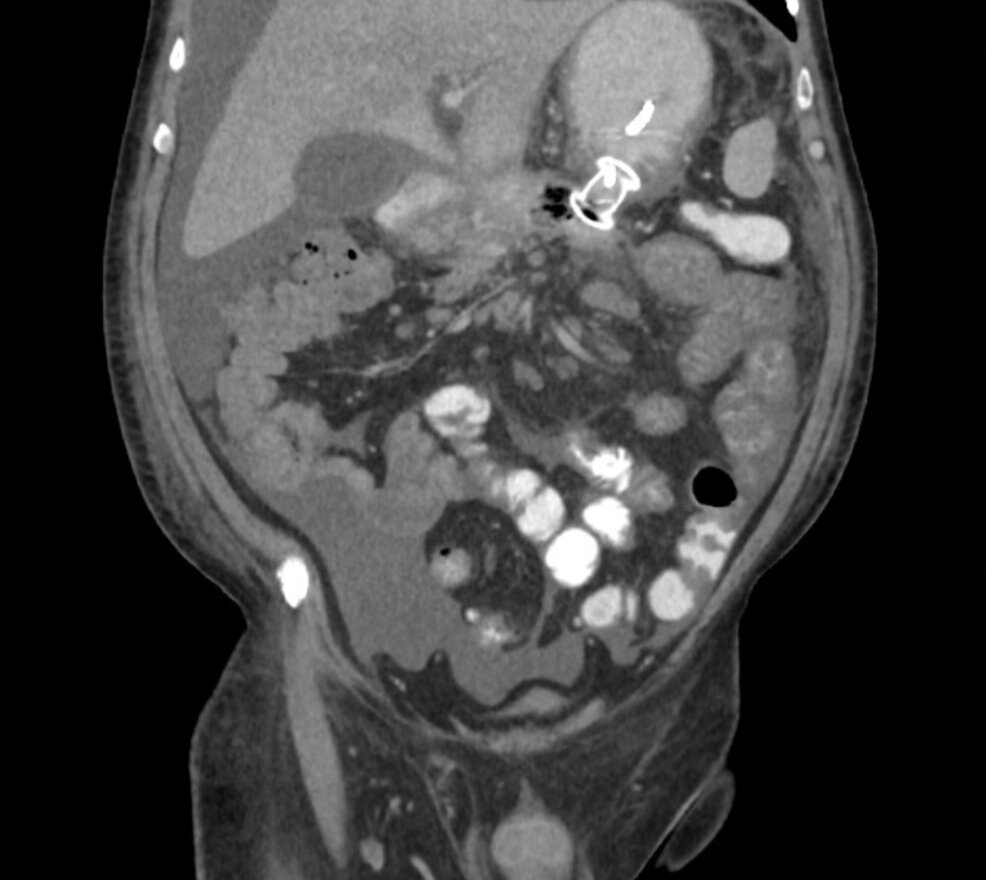
Figure: Coronal CT Abdomen Pelvis with contrast showing Axios stent placement between the pancreatic cyst and the stomach
Disclosures:
Varshita Goduguchinta indicated no relevant financial relationships.
Komlan Guedze indicated no relevant financial relationships.
Hardeep Ahdi indicated no relevant financial relationships.
Raahi Patel indicated no relevant financial relationships.
Zohair Ahmed indicated no relevant financial relationships.
Mohammad Arfeen indicated no relevant financial relationships.
Varshita Goduguchinta, DO1, Komlan Guedze, MD1, Hardeep Ahdi, MD1, Raahi Patel, DO2, Zohair Ahmed, MD1, Mohammad Arfeen, DO3. P0215 - From Drainage to Dilemma: A Complex Journey Through Pancreatic Pseudocyst Fistulization, Necrosis, and Duodenal Stenosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Franciscan Health, Olympia Fields, IL; 2Franciscan Health Olympia Fields, Olympia Fields, IL; 3Franciscan Health, Michigan City, IN
Introduction: Pancreatic pseudocysts are common sequelae of acute or chronic pancreatitis, occurring in up to 40% of cases. Endoscopic ultrasound (EUS)-guided cystogastrostomy using lumen-apposing metal stents (LAMS) has emerged as a minimally invasive, effective technique for symptomatic or infected collections. We describe a rare case of pancreatico-duodenal and pancreatico-colonic fistulization following EUS-guided drainage of walled-off pancreatic necrosis (WON).
Case Description/
Methods: A 59-year-old male with a history of type 2 diabetes mellitus, hypertriglyceridemia, non-alcoholic fatty liver disease, and prior pancreatitis presented with two months of epigastric pain, nausea, vomiting, and unintentional weight loss of 10 kilograms. MRI of the abdomen showed a complex fluid collection measuring 19.7 x 6.3 x 6.6 cm in the pancreatic body and tail, consistent with a pseudocyst. Upper endoscopy revealed a gastric phytobezoar and acquired duodenal stenosis. EUS-guided cystogastrostomy was performed using a 20 x 10 mm LAMS, dilated to 16.5 mm, with a 10 Fr x 4 cm double pigtail stent placed for internal drainage. Purulent material was observed, and the patient was discharged on empiric antibiotics. The patient was readmitted several days later with watery diarrhea and diffuse abdominal pain. Laboratory results showed leukocytosis, hyponatremia, hypokalemia, and elevated fecal elastase. CT revealed a reduction in the size of the collection to 9.1 x 2.4 cm with persistent multiloculated components and pancreatic head edema. Repeat endoscopy showed retained necrotic debris and a duodenal fistula, prompting endoscopic necrosectomy. Colonoscopy identified extrinsic stenosis in the splenic flexure. Follow-up imaging confirmed fistulous tracts between the peripancreatic collection and both the duodenum and colon. Serial imaging later demonstrated resolution of the collection. The stents were removed, and the patient showed clinical improvement with weight gain and symptom resolution.
Discussion: Pancreatico-enteric fistulization is a rare (3–10%) but serious complication of pancreatic pseudocysts and WON. This case illustrates the potential for fistula formation even with appropriate EUS-guided drainage and underscores the need for close monitoring. Endoscopic therapy remains a viable and effective strategy for managing such complex cases.

Figure: Axial CT of Abdomen and Pelvis with contrast highlighting fistula from the pancreatic fluid collection
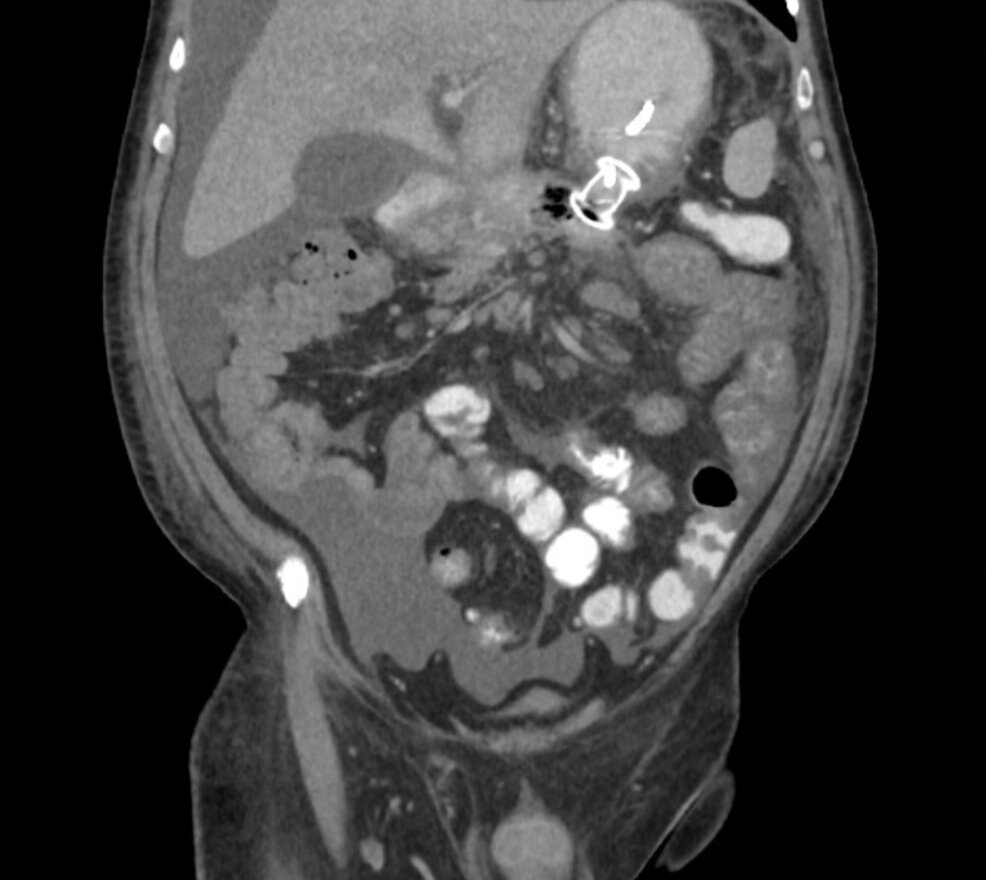
Figure: Coronal CT Abdomen Pelvis with contrast showing Axios stent placement between the pancreatic cyst and the stomach
Disclosures:
Varshita Goduguchinta indicated no relevant financial relationships.
Komlan Guedze indicated no relevant financial relationships.
Hardeep Ahdi indicated no relevant financial relationships.
Raahi Patel indicated no relevant financial relationships.
Zohair Ahmed indicated no relevant financial relationships.
Mohammad Arfeen indicated no relevant financial relationships.
Varshita Goduguchinta, DO1, Komlan Guedze, MD1, Hardeep Ahdi, MD1, Raahi Patel, DO2, Zohair Ahmed, MD1, Mohammad Arfeen, DO3. P0215 - From Drainage to Dilemma: A Complex Journey Through Pancreatic Pseudocyst Fistulization, Necrosis, and Duodenal Stenosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
