Sunday Poster Session
Category: Biliary/Pancreas
P0209 - Pioneering Minimally Invasive Management of Pancreatic Neuroendocrine Tumor: The First Reported EUS-RFA Case in Colombia
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Renzo Pinto-Carta, MD (he/him/his)
Fundacion Santa Fe de Bogota
Bogotá, Distrito Capital de Bogota, Colombia
Presenting Author(s)
Renzo Pinto-Carta, MD, Camilo Humberto Soler Becerra, MD, Maria Alejandra Gomez-Gutierrez, MD, Laura Olarte, MD, Fernando Sierra-Arango, MD, MSc(Epi)
Fundacion Santa Fe de Bogota, Bogotá, Distrito Capital de Bogota, Colombia
Introduction: Pancreatic neuroendocrine tumors (PNETs) are rare neoplasms arising from pancreatic islet cells, representing 1-2% of all pancreatic tumors. Their incidence has increased due to enhanced imaging techniques and aging populations. Managing PNETs can be challenging, especially in patients with significant comorbidities. In Latin America, evidence regarding its use remains limited. This report presents the first documented case of EUS-guided radiofrequency ablation (EUS-RFA) for PNET in Colombia, offering a minimally invasive alternative.
Case Description/
Methods: A 47-year-old man with a history of Hodgkin’s lymphoma (treated with splenectomy, chemotherapy, and radiotherapy), metastatic pulmonary synovial sarcoma, Barrett's esophagus, and asymptomatic multiple gallstones presented with persistent liver enzyme elevation. MRCP/MRI revealed an 18 mm solid lesion in the pancreatic body. Endoscopic ultrasound (EUS) identified a well-defined, hypoechoic, hypervascular lesion. Fine-needle biopsy (FNB) confirmed a well-differentiated grade 1 PNET (Ki-67 1%). PET-CT 68Ga-DOTA showed focal uptake consistent with PNET. After a multidisciplinary discussion, EUS-RFA was chosen over surgical resection due to the patient's comorbidities, including previous thoracic surgeries and pulmonary sarcoma, which increased surgical risks. Under general anesthesia, a 19G radiofrequency needle (Starmed; Taewoong Medical, South Korea) delivered 30W in continuous mode until complete ablation. No immediate complications occurred. One-week follow-up imaging confirmed complete tumor ablation with no enhancement.
Discussion: This case represents the first reported use of EUS-RFA for PNET in Colombia, demonstrating a successful outcome consistent with international experiences. EUS-RFA was selected due to the patient's significant comorbidities, avoiding the risks of surgical resection. Our case aligns with international reports where EUS-RFA has shown high efficacy and low complication rates. However, EUS-RFA is not without risks, including pancreatitis, bleeding, or perforation, which were not observed in this patient. Our experience emphasizes the importance of careful patient selection, multidisciplinary decision-making, and close follow-up. Future studies comparing EUS-RFA with surgical outcomes in PNETs are warranted.
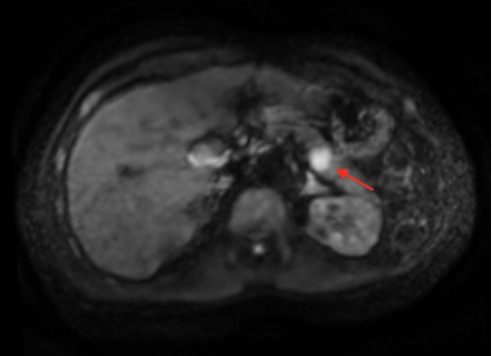
Figure: MRI showing an 18 mm solid lesion located on the posterior margin of the pancreatic body (red arrow).

Figure: Endoscopic ultrasound demonstrating a 18 mm hypervascular solid lesion, consistent with a pancreatic neuroendocrine tumor.
Disclosures:
Renzo Pinto-Carta indicated no relevant financial relationships.
Camilo Humberto Soler Becerra indicated no relevant financial relationships.
Maria Alejandra Gomez-Gutierrez indicated no relevant financial relationships.
Laura Olarte indicated no relevant financial relationships.
Fernando Sierra-Arango indicated no relevant financial relationships.
Renzo Pinto-Carta, MD, Camilo Humberto Soler Becerra, MD, Maria Alejandra Gomez-Gutierrez, MD, Laura Olarte, MD, Fernando Sierra-Arango, MD, MSc(Epi). P0209 - Pioneering Minimally Invasive Management of Pancreatic Neuroendocrine Tumor: The First Reported EUS-RFA Case in Colombia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Fundacion Santa Fe de Bogota, Bogotá, Distrito Capital de Bogota, Colombia
Introduction: Pancreatic neuroendocrine tumors (PNETs) are rare neoplasms arising from pancreatic islet cells, representing 1-2% of all pancreatic tumors. Their incidence has increased due to enhanced imaging techniques and aging populations. Managing PNETs can be challenging, especially in patients with significant comorbidities. In Latin America, evidence regarding its use remains limited. This report presents the first documented case of EUS-guided radiofrequency ablation (EUS-RFA) for PNET in Colombia, offering a minimally invasive alternative.
Case Description/
Methods: A 47-year-old man with a history of Hodgkin’s lymphoma (treated with splenectomy, chemotherapy, and radiotherapy), metastatic pulmonary synovial sarcoma, Barrett's esophagus, and asymptomatic multiple gallstones presented with persistent liver enzyme elevation. MRCP/MRI revealed an 18 mm solid lesion in the pancreatic body. Endoscopic ultrasound (EUS) identified a well-defined, hypoechoic, hypervascular lesion. Fine-needle biopsy (FNB) confirmed a well-differentiated grade 1 PNET (Ki-67 1%). PET-CT 68Ga-DOTA showed focal uptake consistent with PNET. After a multidisciplinary discussion, EUS-RFA was chosen over surgical resection due to the patient's comorbidities, including previous thoracic surgeries and pulmonary sarcoma, which increased surgical risks. Under general anesthesia, a 19G radiofrequency needle (Starmed; Taewoong Medical, South Korea) delivered 30W in continuous mode until complete ablation. No immediate complications occurred. One-week follow-up imaging confirmed complete tumor ablation with no enhancement.
Discussion: This case represents the first reported use of EUS-RFA for PNET in Colombia, demonstrating a successful outcome consistent with international experiences. EUS-RFA was selected due to the patient's significant comorbidities, avoiding the risks of surgical resection. Our case aligns with international reports where EUS-RFA has shown high efficacy and low complication rates. However, EUS-RFA is not without risks, including pancreatitis, bleeding, or perforation, which were not observed in this patient. Our experience emphasizes the importance of careful patient selection, multidisciplinary decision-making, and close follow-up. Future studies comparing EUS-RFA with surgical outcomes in PNETs are warranted.
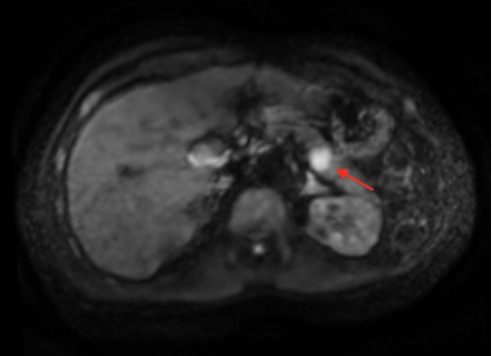
Figure: MRI showing an 18 mm solid lesion located on the posterior margin of the pancreatic body (red arrow).

Figure: Endoscopic ultrasound demonstrating a 18 mm hypervascular solid lesion, consistent with a pancreatic neuroendocrine tumor.
Disclosures:
Renzo Pinto-Carta indicated no relevant financial relationships.
Camilo Humberto Soler Becerra indicated no relevant financial relationships.
Maria Alejandra Gomez-Gutierrez indicated no relevant financial relationships.
Laura Olarte indicated no relevant financial relationships.
Fernando Sierra-Arango indicated no relevant financial relationships.
Renzo Pinto-Carta, MD, Camilo Humberto Soler Becerra, MD, Maria Alejandra Gomez-Gutierrez, MD, Laura Olarte, MD, Fernando Sierra-Arango, MD, MSc(Epi). P0209 - Pioneering Minimally Invasive Management of Pancreatic Neuroendocrine Tumor: The First Reported EUS-RFA Case in Colombia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
