Sunday Poster Session
Category: Biliary/Pancreas
P0208 - Candida in the Biliary Tree: Diagnostic and Clinical Implications of a Rare Finding
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Varun Vemulapalli, MD
McGovern Medical School at UTHealth
Houston, TX
Presenting Author(s)
Varun Vemulapalli, MD1, Cristina Natha, MD1, Abdullah Aleem, MD1, Eric D. Yoon, MD2, Nirav Thosani, MD3
1McGovern Medical School at UTHealth, Houston, TX; 2McGovern Medical School at UTHealth Houston, Houston, TX; 3University of Texas Health, McGovern Medical School, Houston, TX
Introduction: Fungal infections of the biliary tree are exceedingly rare but may present with cholestasis, obstructive jaundice, and imaging findings that complicate diagnosis. Candida species, in particular, have been reported in critically ill or immunocompromised patients, typically after biliary instrumentation and may lead to biliary cast formation and progressive bile duct injury.
Case Description/
Methods: A 68-year-old male with recently diagnosed prostate cancer (not on therapy) was hospitalized for multifocal pneumonia complicated by septic shock, intubation, and acute tubular necrosis requiring hemodialysis. His course was further complicated by cholestatic liver injury. Magnetic resonance cholangiopancreatography revealed hepatomegaly and a nondilated common bile duct. Hepatobiliary iminodiacetic acid scan suggested cystic duct obstruction, prompting cholecystectomy. Intraoperative cholangiogram was normal; however, rising liver enzymes led to endoscopic retrograde cholangiopancreatography (ERCP), which revealed common bile duct filling defects with mucus and stones. Brushings were negative for malignancy but demonstrated fungal elements consistent with Candida species. Infectious disease was consulted, and he was treated with fluconazole. Liver enzymes peaked with total bilirubin 11.2 mg/dL (direct 10.0, indirect 1.2), alkaline phosphatase 1024 U/L, AST 140 U/L, ALT 255 U/L, and INR 1.84. Repeat ERCP with cholangioscopy revealed friable mucosa, extensive biliary casts, and a migrated stent. Liver biopsy showed bile infarcts, cholestasis, ductular proliferation, and early fibrosis. IgG was elevated (1706 mg/dL) with normal IgG4. Imaging ruled out extrahepatic obstruction, but intrahepatic ducts appeared pruned. Findings were consistent with secondary sclerosing cholangitis likely from ischemic cholangiopathy in the setting of septic shock, with concurrent biliary candidiasis. The patient was referred to hepatology for liver transplant evaluation.
Discussion: Biliary tract candidiasis is exceptionally rare and often underrecognized. This case is unique in that the patient also presented for sepsis of a non-biliary source and developed SSC as a result. While it is unclear if Candida was pathogenic and contributing to SSC in this case, fungal involvement in the biliary system in the absence of GI malignancy and prior instrumentation is unusual. In patients with persistent cholestasis and risk factors, fungal infection should remain on the differential to ensure prompt recognition and treatment.
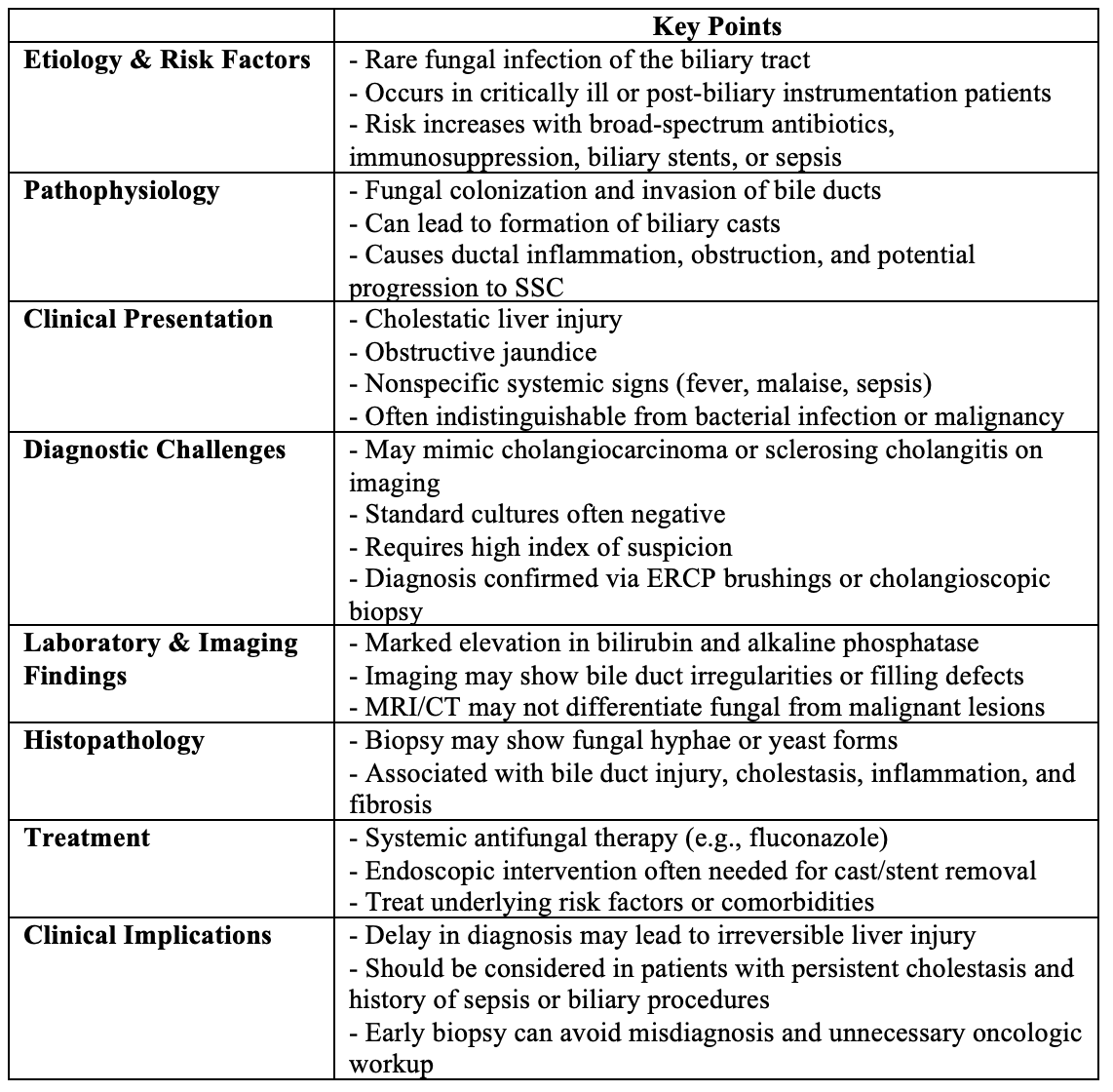
Figure: Clinical Considerations in Biliary Tract Candidiasis
Disclosures:
Varun Vemulapalli indicated no relevant financial relationships.
Cristina Natha indicated no relevant financial relationships.
Abdullah Aleem indicated no relevant financial relationships.
Eric Yoon indicated no relevant financial relationships.
Nirav Thosani: Alpfa medical – Consultant. Roseaid – Creatorship rights.
Varun Vemulapalli, MD1, Cristina Natha, MD1, Abdullah Aleem, MD1, Eric D. Yoon, MD2, Nirav Thosani, MD3. P0208 - Candida in the Biliary Tree: Diagnostic and Clinical Implications of a Rare Finding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1McGovern Medical School at UTHealth, Houston, TX; 2McGovern Medical School at UTHealth Houston, Houston, TX; 3University of Texas Health, McGovern Medical School, Houston, TX
Introduction: Fungal infections of the biliary tree are exceedingly rare but may present with cholestasis, obstructive jaundice, and imaging findings that complicate diagnosis. Candida species, in particular, have been reported in critically ill or immunocompromised patients, typically after biliary instrumentation and may lead to biliary cast formation and progressive bile duct injury.
Case Description/
Methods: A 68-year-old male with recently diagnosed prostate cancer (not on therapy) was hospitalized for multifocal pneumonia complicated by septic shock, intubation, and acute tubular necrosis requiring hemodialysis. His course was further complicated by cholestatic liver injury. Magnetic resonance cholangiopancreatography revealed hepatomegaly and a nondilated common bile duct. Hepatobiliary iminodiacetic acid scan suggested cystic duct obstruction, prompting cholecystectomy. Intraoperative cholangiogram was normal; however, rising liver enzymes led to endoscopic retrograde cholangiopancreatography (ERCP), which revealed common bile duct filling defects with mucus and stones. Brushings were negative for malignancy but demonstrated fungal elements consistent with Candida species. Infectious disease was consulted, and he was treated with fluconazole. Liver enzymes peaked with total bilirubin 11.2 mg/dL (direct 10.0, indirect 1.2), alkaline phosphatase 1024 U/L, AST 140 U/L, ALT 255 U/L, and INR 1.84. Repeat ERCP with cholangioscopy revealed friable mucosa, extensive biliary casts, and a migrated stent. Liver biopsy showed bile infarcts, cholestasis, ductular proliferation, and early fibrosis. IgG was elevated (1706 mg/dL) with normal IgG4. Imaging ruled out extrahepatic obstruction, but intrahepatic ducts appeared pruned. Findings were consistent with secondary sclerosing cholangitis likely from ischemic cholangiopathy in the setting of septic shock, with concurrent biliary candidiasis. The patient was referred to hepatology for liver transplant evaluation.
Discussion: Biliary tract candidiasis is exceptionally rare and often underrecognized. This case is unique in that the patient also presented for sepsis of a non-biliary source and developed SSC as a result. While it is unclear if Candida was pathogenic and contributing to SSC in this case, fungal involvement in the biliary system in the absence of GI malignancy and prior instrumentation is unusual. In patients with persistent cholestasis and risk factors, fungal infection should remain on the differential to ensure prompt recognition and treatment.
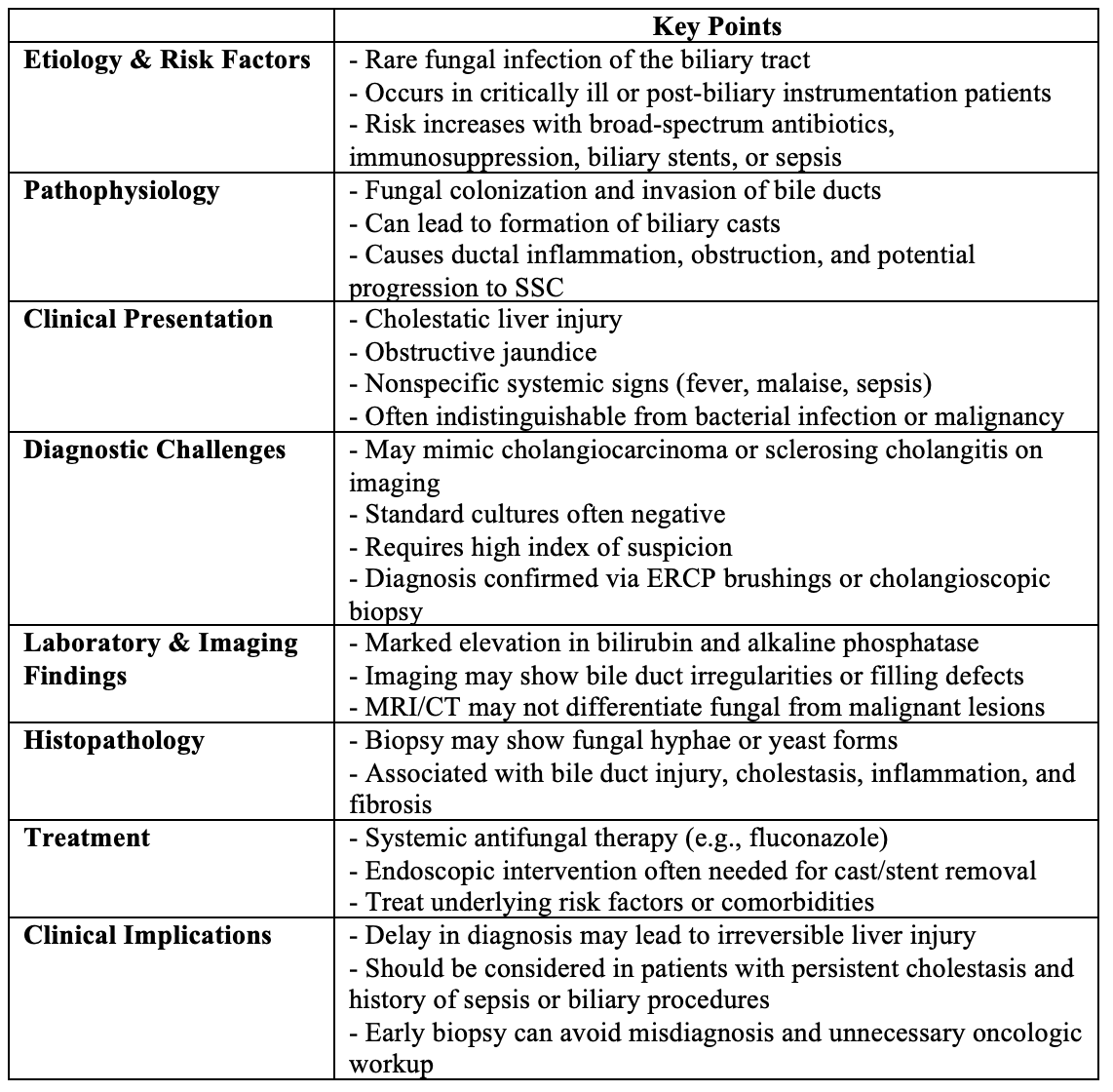
Figure: Clinical Considerations in Biliary Tract Candidiasis
Disclosures:
Varun Vemulapalli indicated no relevant financial relationships.
Cristina Natha indicated no relevant financial relationships.
Abdullah Aleem indicated no relevant financial relationships.
Eric Yoon indicated no relevant financial relationships.
Nirav Thosani: Alpfa medical – Consultant. Roseaid – Creatorship rights.
Varun Vemulapalli, MD1, Cristina Natha, MD1, Abdullah Aleem, MD1, Eric D. Yoon, MD2, Nirav Thosani, MD3. P0208 - Candida in the Biliary Tree: Diagnostic and Clinical Implications of a Rare Finding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
