Sunday Poster Session
Category: Biliary/Pancreas
P0207 - Optimizing WOPN Management: Multimodal Endoscopic Intervention Leading to Early Resolution
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Tanvi Gupta, MD
University of Texas Health Science Center
Houston, TX
Presenting Author(s)
Tanvi Gupta, MD1, Clay Smithhart, MD2, Aastha Bharwad, MD3, Sruthi Subramanian, MD4
1University of Texas Health Science Center, Houston, TX; 2University of Texas Health, McGovern Medical School, Houston, TX; 3University of Texas at Houston, Houston, TX; 4University of Texas Health Sciences Center in Houston, Houston, TX
Introduction: Walled-off pancreatic necrosis (WOPN) is a late complication of acute necrotizing pancreatitis with high morbidity. Management can include interventional radiology-guided drain placement, endoscopic ultrasound (EUS)-guided transmural drainage, or surgical debridement. EUS-guided cystogastrostomy with a lumen-apposing metal stent (LAMS) placement is preferred due to its superior safety profile and lower complication rates, however recovery can be delayed when infection or extensive necrotic burden persists. Direct endoscopic necrosectomy may then be required through the LAMS. Adjunctive therapies, including hydrogen peroxide lavage and nasocystic irrigation, can improve debris clearance, however data on their combined use remains limited. We present a complex case of a large WOPN successfully managed through a multimodal endoscopic approach, leading to early resolution.
Case Description/
Methods: A 64-year-old male with chronic alcohol-related necrotizing pancreatitis presented in septic shock with worsening abdominal pain, diarrhea, and fevers. Cross-sectional imaging revealed a large, gas-containing WOPN measuring 17.6 × 9 × 8 cm. EUS confirmed a mature WOPN. Cystogastrostomy was performed with deployment of a 20mm LAMS, draining thick fluid and necrotic debris. Over 1 month, the patient underwent 4 necrosectomies with hydrogen peroxide lavage to facilitate debridement (figure 1). An 8 French nasojejunal tube was also positioned within the necrotic cavity to deliver continuous saline irrigation at 50 mL/hour. The patient's clinical condition steadily improved in the ICU. The final necrosectomy showed complete endoscopic clearance of necrotic material (figure 2). The LAMS was removed, and 2 double pigtail plastic stents were placed to maintain drainage. Follow-up imaging 3 days later demonstrated significant reduction in the size of the collection (10.2 × 4 × 3 cm). Repeat imaging 1 month later confirmed complete resolution.
Discussion: In this case, a combined endoscopic approach (EUS-guided cystogastrostomy, serial necrosectomies with hydrogen peroxide lavage, and continuous saline irrigation via nasocystic drainage) allowed for complete and accelerated resolution of the necrotic collection and fewer necrosectomies than typically required. This synergistic approach may enhance treatment efficiency and patient outcomes in complex cases of WOPN. Further studies are warranted to assess long-term outcomes and to directly compare this multimodal strategy with standard endoscopic necrosectomy alone.
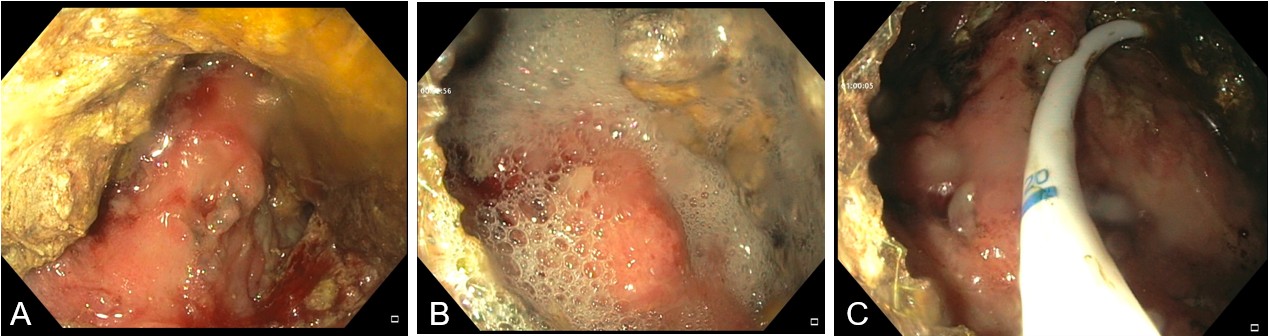
Figure: Figure 1: Large amounts of necrotic material seen within the WOPN cavity (A), treated with hydrogen peroxide lavage to facilitate debridement (B) and placement of an 8 French nasojejunal within the necrotic cavity to deliver continuous saline irrigation at 50 mL/hour (C).

Figure: Figure 2: Complete endoscopic clearance of necrotic material after utilizing the multimodal approach.
Disclosures:
Tanvi Gupta indicated no relevant financial relationships.
Clay Smithhart indicated no relevant financial relationships.
Aastha Bharwad indicated no relevant financial relationships.
Sruthi Subramanian indicated no relevant financial relationships.
Tanvi Gupta, MD1, Clay Smithhart, MD2, Aastha Bharwad, MD3, Sruthi Subramanian, MD4. P0207 - Optimizing WOPN Management: Multimodal Endoscopic Intervention Leading to Early Resolution, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas Health Science Center, Houston, TX; 2University of Texas Health, McGovern Medical School, Houston, TX; 3University of Texas at Houston, Houston, TX; 4University of Texas Health Sciences Center in Houston, Houston, TX
Introduction: Walled-off pancreatic necrosis (WOPN) is a late complication of acute necrotizing pancreatitis with high morbidity. Management can include interventional radiology-guided drain placement, endoscopic ultrasound (EUS)-guided transmural drainage, or surgical debridement. EUS-guided cystogastrostomy with a lumen-apposing metal stent (LAMS) placement is preferred due to its superior safety profile and lower complication rates, however recovery can be delayed when infection or extensive necrotic burden persists. Direct endoscopic necrosectomy may then be required through the LAMS. Adjunctive therapies, including hydrogen peroxide lavage and nasocystic irrigation, can improve debris clearance, however data on their combined use remains limited. We present a complex case of a large WOPN successfully managed through a multimodal endoscopic approach, leading to early resolution.
Case Description/
Methods: A 64-year-old male with chronic alcohol-related necrotizing pancreatitis presented in septic shock with worsening abdominal pain, diarrhea, and fevers. Cross-sectional imaging revealed a large, gas-containing WOPN measuring 17.6 × 9 × 8 cm. EUS confirmed a mature WOPN. Cystogastrostomy was performed with deployment of a 20mm LAMS, draining thick fluid and necrotic debris. Over 1 month, the patient underwent 4 necrosectomies with hydrogen peroxide lavage to facilitate debridement (figure 1). An 8 French nasojejunal tube was also positioned within the necrotic cavity to deliver continuous saline irrigation at 50 mL/hour. The patient's clinical condition steadily improved in the ICU. The final necrosectomy showed complete endoscopic clearance of necrotic material (figure 2). The LAMS was removed, and 2 double pigtail plastic stents were placed to maintain drainage. Follow-up imaging 3 days later demonstrated significant reduction in the size of the collection (10.2 × 4 × 3 cm). Repeat imaging 1 month later confirmed complete resolution.
Discussion: In this case, a combined endoscopic approach (EUS-guided cystogastrostomy, serial necrosectomies with hydrogen peroxide lavage, and continuous saline irrigation via nasocystic drainage) allowed for complete and accelerated resolution of the necrotic collection and fewer necrosectomies than typically required. This synergistic approach may enhance treatment efficiency and patient outcomes in complex cases of WOPN. Further studies are warranted to assess long-term outcomes and to directly compare this multimodal strategy with standard endoscopic necrosectomy alone.
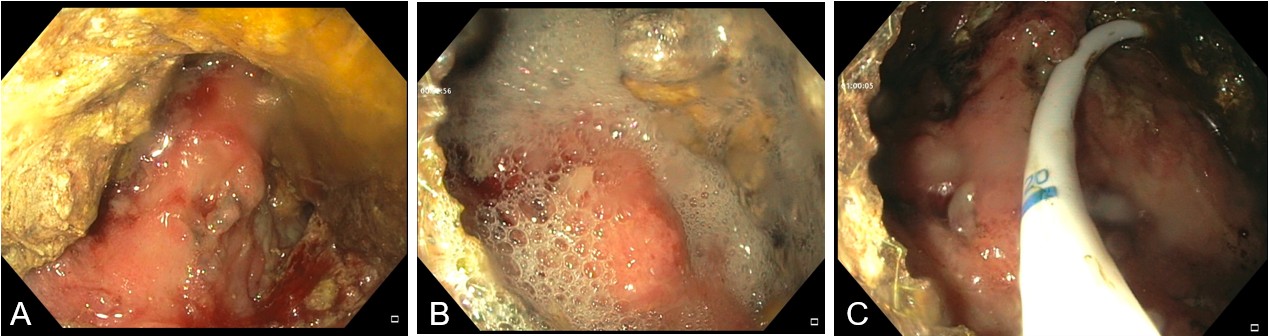
Figure: Figure 1: Large amounts of necrotic material seen within the WOPN cavity (A), treated with hydrogen peroxide lavage to facilitate debridement (B) and placement of an 8 French nasojejunal within the necrotic cavity to deliver continuous saline irrigation at 50 mL/hour (C).

Figure: Figure 2: Complete endoscopic clearance of necrotic material after utilizing the multimodal approach.
Disclosures:
Tanvi Gupta indicated no relevant financial relationships.
Clay Smithhart indicated no relevant financial relationships.
Aastha Bharwad indicated no relevant financial relationships.
Sruthi Subramanian indicated no relevant financial relationships.
Tanvi Gupta, MD1, Clay Smithhart, MD2, Aastha Bharwad, MD3, Sruthi Subramanian, MD4. P0207 - Optimizing WOPN Management: Multimodal Endoscopic Intervention Leading to Early Resolution, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

