Sunday Poster Session
Category: Biliary/Pancreas
P0205 - When Glands and Squames Collide: Pancreatic Adenosquamous Carcinoma, an Uncommon Histologic Variant With Aggressive Behavior
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Abdullah Sultany, MD
Guthrie Robert Packer Hospital, Department of Internal Medicine
Sayre, PA
Presenting Author(s)
Abdullah Sultany, MD1, Raja Chandra Chakinala, MD2, Christopher D Manko, MD3, Cristina Aguilar, MD4, Thomas McDonald, MD5, Michael Georgetson, MD, FACG5
1Guthrie Robert Packer Hospital, Department of Internal Medicine, Sayre, PA; 2Guthrie Robert Packer Hospital, Sayre, PA, Sayre, PA; 3Geisinger Commonwealth School of Medicine, Sayre, PA; 4Guthrie Robert Packer Hospital, Department of Pathology, Sayre, PA; 5Guthrie Robert Packer Hospital, Department of Gastroenterology, Sayre, PA
Introduction: Pancreatic adenosquamous carcinoma (ASC) is a rare and highly aggressive subtype of pancreatic cancer, characterized by both glandular and squamous cell differentiation, accounting for 0.4% to 4% of all pancreatic malignancies. We present a case of ASC that underscores key clinical insights into its presentation, management, and potential treatment-related complications.
Case Description/
Methods: A 79-year-old gentleman originally from China presented with a three-month history of progressively worsening fatigue, belching, decreased appetite, and weight loss. Abdominal CT revealed a 5.1 × 6.5 × 5.4 cm enhancing mass with irregular margins centered in the pancreatic head/uncinate process, pancreatic duct dilation up to 1.1 cm, intrahepatic biliary dilation, CBD dilation to 2.1 cm, multiple hypodense liver lesions, and complete encasement of the SMA, portal vein, and SMV. Liver function tests were normal, but tumor markers were elevated: CA 19-9 at 648 U/mL and carcinoembryonic antigen (CEA) at 23.8 ng/mL. EUS-guided fine needle aspiration confirmed ASC (Figure 1). Due to extensive vascular involvement and metastases, surgery was not an option, and chemotherapy was planned. One month later, the patient returned to the emergency department with worsening fatigue and new-onset jaundice. ERCP revealed severe malignant strictures in the lower and middle thirds of the main bile duct. An uncovered metal biliary stent was placed in the CBD. However, the patient’s jaundice worsened, with bilirubin rising from 6.4 mg/dL to 9.3 mg/dL. A repeat ERCP showed partial occlusion of the initial stent due to tissue ingrowth and blood clots (Figure 2). The biliary tree was swept, and a covered metal stent was deployed within the pre-existing stent.
Discussion: ASC of the pancreas is a rare and highly aggressive malignancy, with reported 1- and 2-year survival rates of approximately 50% and 30%, respectively. Clinical presentations vary and may include abdominal pain, painless jaundice, weight loss, anorexia, back pain, steatorrhea, and pruritus. Radical surgical resection with negative margins is the main curative approach; however, only 15–20% of patients qualify for surgery. Neoadjuvant and adjuvant chemoradiation may improve resectability and survival. We report a rare case of inoperable pancreatic ASC managed with biliary stenting complicated by partial occlusion. Given the tumor’s aggressive nature, endoscopists should be alert to stent-related complications.
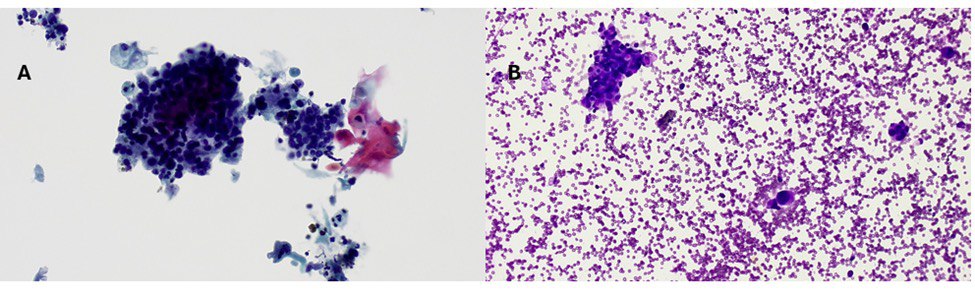
Figure: Figure 1. Cytology Showing Keratinizing Squamous Cell (A) and Adenocarcinoma (B) Components
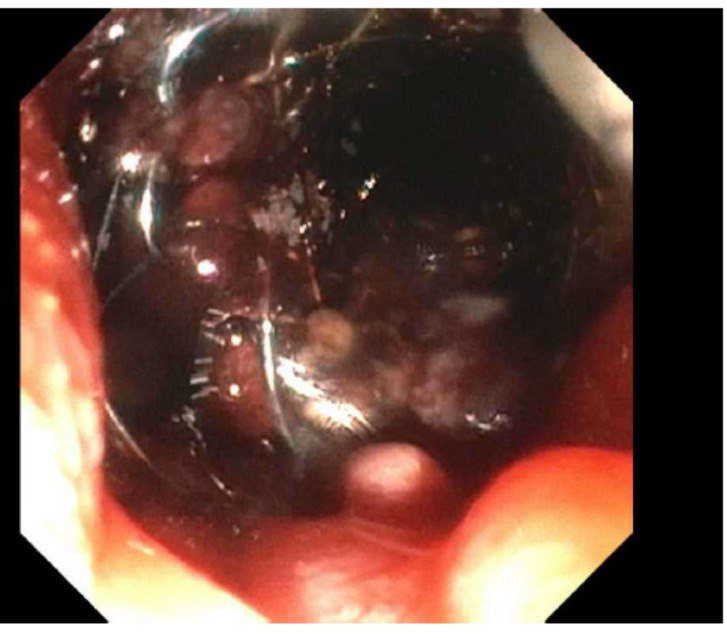
Figure: Figure 2. Partially occluded covered metal stent in the CBD
Disclosures:
Abdullah Sultany indicated no relevant financial relationships.
Raja Chandra Chakinala indicated no relevant financial relationships.
Christopher D Manko indicated no relevant financial relationships.
Cristina Aguilar indicated no relevant financial relationships.
Thomas McDonald indicated no relevant financial relationships.
Michael Georgetson indicated no relevant financial relationships.
Abdullah Sultany, MD1, Raja Chandra Chakinala, MD2, Christopher D Manko, MD3, Cristina Aguilar, MD4, Thomas McDonald, MD5, Michael Georgetson, MD, FACG5. P0205 - When Glands and Squames Collide: Pancreatic Adenosquamous Carcinoma, an Uncommon Histologic Variant With Aggressive Behavior, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Guthrie Robert Packer Hospital, Department of Internal Medicine, Sayre, PA; 2Guthrie Robert Packer Hospital, Sayre, PA, Sayre, PA; 3Geisinger Commonwealth School of Medicine, Sayre, PA; 4Guthrie Robert Packer Hospital, Department of Pathology, Sayre, PA; 5Guthrie Robert Packer Hospital, Department of Gastroenterology, Sayre, PA
Introduction: Pancreatic adenosquamous carcinoma (ASC) is a rare and highly aggressive subtype of pancreatic cancer, characterized by both glandular and squamous cell differentiation, accounting for 0.4% to 4% of all pancreatic malignancies. We present a case of ASC that underscores key clinical insights into its presentation, management, and potential treatment-related complications.
Case Description/
Methods: A 79-year-old gentleman originally from China presented with a three-month history of progressively worsening fatigue, belching, decreased appetite, and weight loss. Abdominal CT revealed a 5.1 × 6.5 × 5.4 cm enhancing mass with irregular margins centered in the pancreatic head/uncinate process, pancreatic duct dilation up to 1.1 cm, intrahepatic biliary dilation, CBD dilation to 2.1 cm, multiple hypodense liver lesions, and complete encasement of the SMA, portal vein, and SMV. Liver function tests were normal, but tumor markers were elevated: CA 19-9 at 648 U/mL and carcinoembryonic antigen (CEA) at 23.8 ng/mL. EUS-guided fine needle aspiration confirmed ASC (Figure 1). Due to extensive vascular involvement and metastases, surgery was not an option, and chemotherapy was planned. One month later, the patient returned to the emergency department with worsening fatigue and new-onset jaundice. ERCP revealed severe malignant strictures in the lower and middle thirds of the main bile duct. An uncovered metal biliary stent was placed in the CBD. However, the patient’s jaundice worsened, with bilirubin rising from 6.4 mg/dL to 9.3 mg/dL. A repeat ERCP showed partial occlusion of the initial stent due to tissue ingrowth and blood clots (Figure 2). The biliary tree was swept, and a covered metal stent was deployed within the pre-existing stent.
Discussion: ASC of the pancreas is a rare and highly aggressive malignancy, with reported 1- and 2-year survival rates of approximately 50% and 30%, respectively. Clinical presentations vary and may include abdominal pain, painless jaundice, weight loss, anorexia, back pain, steatorrhea, and pruritus. Radical surgical resection with negative margins is the main curative approach; however, only 15–20% of patients qualify for surgery. Neoadjuvant and adjuvant chemoradiation may improve resectability and survival. We report a rare case of inoperable pancreatic ASC managed with biliary stenting complicated by partial occlusion. Given the tumor’s aggressive nature, endoscopists should be alert to stent-related complications.
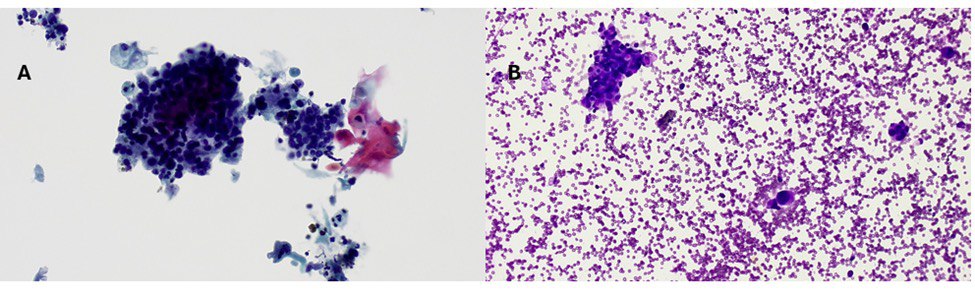
Figure: Figure 1. Cytology Showing Keratinizing Squamous Cell (A) and Adenocarcinoma (B) Components
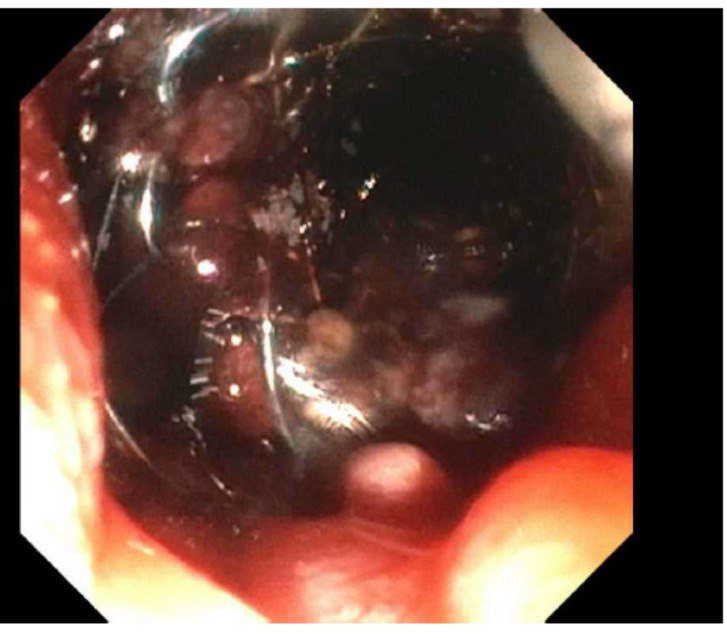
Figure: Figure 2. Partially occluded covered metal stent in the CBD
Disclosures:
Abdullah Sultany indicated no relevant financial relationships.
Raja Chandra Chakinala indicated no relevant financial relationships.
Christopher D Manko indicated no relevant financial relationships.
Cristina Aguilar indicated no relevant financial relationships.
Thomas McDonald indicated no relevant financial relationships.
Michael Georgetson indicated no relevant financial relationships.
Abdullah Sultany, MD1, Raja Chandra Chakinala, MD2, Christopher D Manko, MD3, Cristina Aguilar, MD4, Thomas McDonald, MD5, Michael Georgetson, MD, FACG5. P0205 - When Glands and Squames Collide: Pancreatic Adenosquamous Carcinoma, an Uncommon Histologic Variant With Aggressive Behavior, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
