Sunday Poster Session
Category: Colon
P0362 - Delayed Diagnosis of Collagenous Colitis in a Young Woman With Prior SARS-CoV-2 Infection
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Amy Yeung, DO (she/her/hers)
Valley Health System, Icahn School of Medicine at Mount Sinai
Paramus, NJ
Presenting Author(s)
Amy Yeung, DO1, Sugandha Bollu, BA2, Elizabeth Eapen, MD1, Sita Chokhavatia, MD, MACG1
1Valley Health System, Icahn School of Medicine at Mount Sinai, Paramus, NJ; 2Saint Louis University School of Medicine, Saint Louis, MO
Introduction: Collagenous colitis (CC) is a subtype of microscopic colitis characterized by chronic, watery, non-bloody diarrhea, commonly affecting individuals over the age of 60. Diagnosis can be challenging due to non-specific symptoms and often normal endoscopic appearance. While its pathogenesis is not fully understood, recent evidence suggests a possible association between CC and preceding SARS-CoV-2 infection. Patients with CC are also susceptible to superimposed infections. We present a case of delayed CC diagnosis in a woman with persistent diarrhea following SARS-CoV-2 infection, complicated by Clostridioides difficile (CD) infection.
Case Description/
Methods: A 61-year-old woman presented with seven-months of persistent watery diarrhea, a 7-kg weight loss, and decreased oral intake. She recalled a prior episode of severe diarrhea occurring 4 weeks after a SARS-CoV-2 infection. Initial esophagogastroduodenoscopy (EGD) and colonoscopy showed non-specific chronic colitis, and she was empirically treated with mesalamine without improvement.
She later presented to our hospital with diarrhea, myalgias, fever, and generalized weakness, attributed to a viral-like illness. Labs revealed positive stool leukocytes; CD polymerase chain reaction (PCR) and enteric stool studies were negative. Repeat colonoscopy and EGD were grossly normal, but biopsies revealed active colitis with crypt abscesses. Biopsies were sent to a tertiary center for further review. Her symptoms improved with supportive care, and she was discharged.
Four days later, she returned with worsening diarrhea. Fecal calprotectin was elevated at 646 μg/g and repeat CD PCR was now positive. She was treated with oral vancomycin, with subsequent improvement. Final pathology report revealed irregular epithelial injury and a thickened subepithelial collagen enveloping microvasculature, without increased intraepithelial lymphocytes (Figure 1a and 1b) consistent with CC. She was treated with oral budesonide and at 8 weeks follow-up, reported marked improvement.
Discussion: This case illustrates the diagnostic challenges of CC, particularly when obscured by nonspecific pathology and superimposed infections. A preceding SARS-CoV-2 infection may have triggered disease onset. Timely histopathologic confirmation is crucial, as early treatment can lead to rapid clinical resolution.
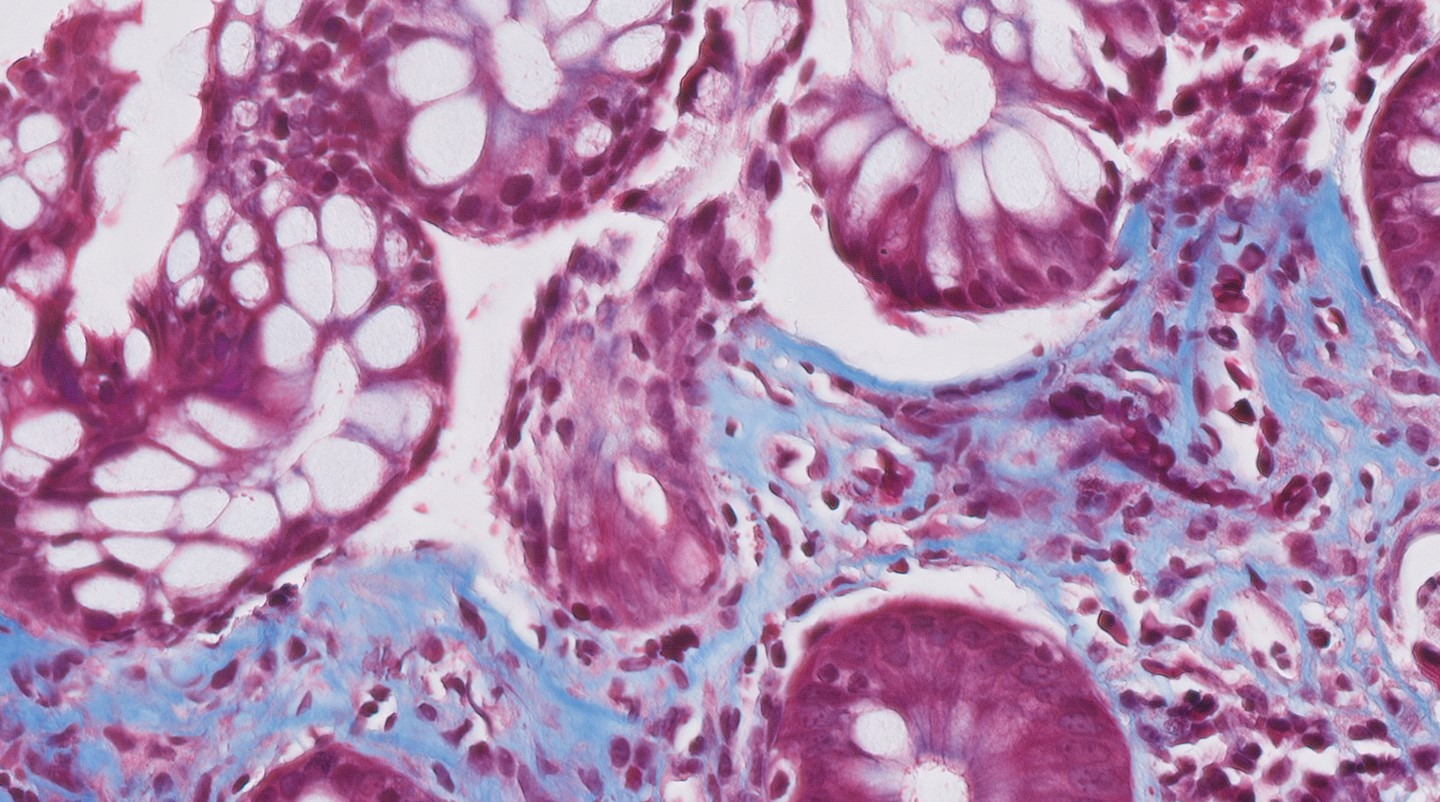
Figure: Figure 1a: Trichome stain, 20x magnification showing a thickened subepithelial collagen band.
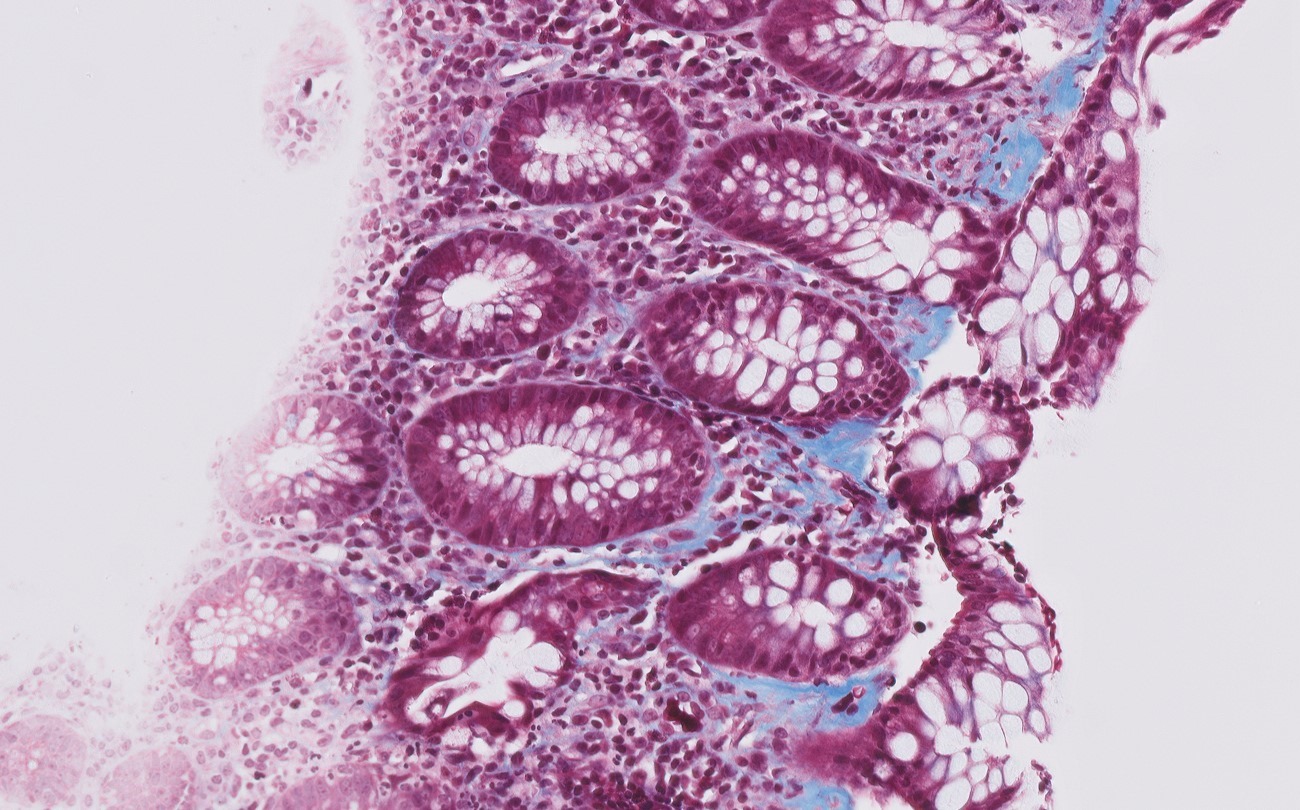
Figure: Figure 1b: Trichome stain, 40x magnification demonstrating collagen band around small capillaries. Notably, there is no significant increase in intraepithelial lymphocytes that are typically seen in CC.
Disclosures:
Amy Yeung indicated no relevant financial relationships.
Sugandha Bollu indicated no relevant financial relationships.
Elizabeth Eapen indicated no relevant financial relationships.
Sita Chokhavatia indicated no relevant financial relationships.
Amy Yeung, DO1, Sugandha Bollu, BA2, Elizabeth Eapen, MD1, Sita Chokhavatia, MD, MACG1. P0362 - Delayed Diagnosis of Collagenous Colitis in a Young Woman With Prior SARS-CoV-2 Infection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Valley Health System, Icahn School of Medicine at Mount Sinai, Paramus, NJ; 2Saint Louis University School of Medicine, Saint Louis, MO
Introduction: Collagenous colitis (CC) is a subtype of microscopic colitis characterized by chronic, watery, non-bloody diarrhea, commonly affecting individuals over the age of 60. Diagnosis can be challenging due to non-specific symptoms and often normal endoscopic appearance. While its pathogenesis is not fully understood, recent evidence suggests a possible association between CC and preceding SARS-CoV-2 infection. Patients with CC are also susceptible to superimposed infections. We present a case of delayed CC diagnosis in a woman with persistent diarrhea following SARS-CoV-2 infection, complicated by Clostridioides difficile (CD) infection.
Case Description/
Methods: A 61-year-old woman presented with seven-months of persistent watery diarrhea, a 7-kg weight loss, and decreased oral intake. She recalled a prior episode of severe diarrhea occurring 4 weeks after a SARS-CoV-2 infection. Initial esophagogastroduodenoscopy (EGD) and colonoscopy showed non-specific chronic colitis, and she was empirically treated with mesalamine without improvement.
She later presented to our hospital with diarrhea, myalgias, fever, and generalized weakness, attributed to a viral-like illness. Labs revealed positive stool leukocytes; CD polymerase chain reaction (PCR) and enteric stool studies were negative. Repeat colonoscopy and EGD were grossly normal, but biopsies revealed active colitis with crypt abscesses. Biopsies were sent to a tertiary center for further review. Her symptoms improved with supportive care, and she was discharged.
Four days later, she returned with worsening diarrhea. Fecal calprotectin was elevated at 646 μg/g and repeat CD PCR was now positive. She was treated with oral vancomycin, with subsequent improvement. Final pathology report revealed irregular epithelial injury and a thickened subepithelial collagen enveloping microvasculature, without increased intraepithelial lymphocytes (Figure 1a and 1b) consistent with CC. She was treated with oral budesonide and at 8 weeks follow-up, reported marked improvement.
Discussion: This case illustrates the diagnostic challenges of CC, particularly when obscured by nonspecific pathology and superimposed infections. A preceding SARS-CoV-2 infection may have triggered disease onset. Timely histopathologic confirmation is crucial, as early treatment can lead to rapid clinical resolution.
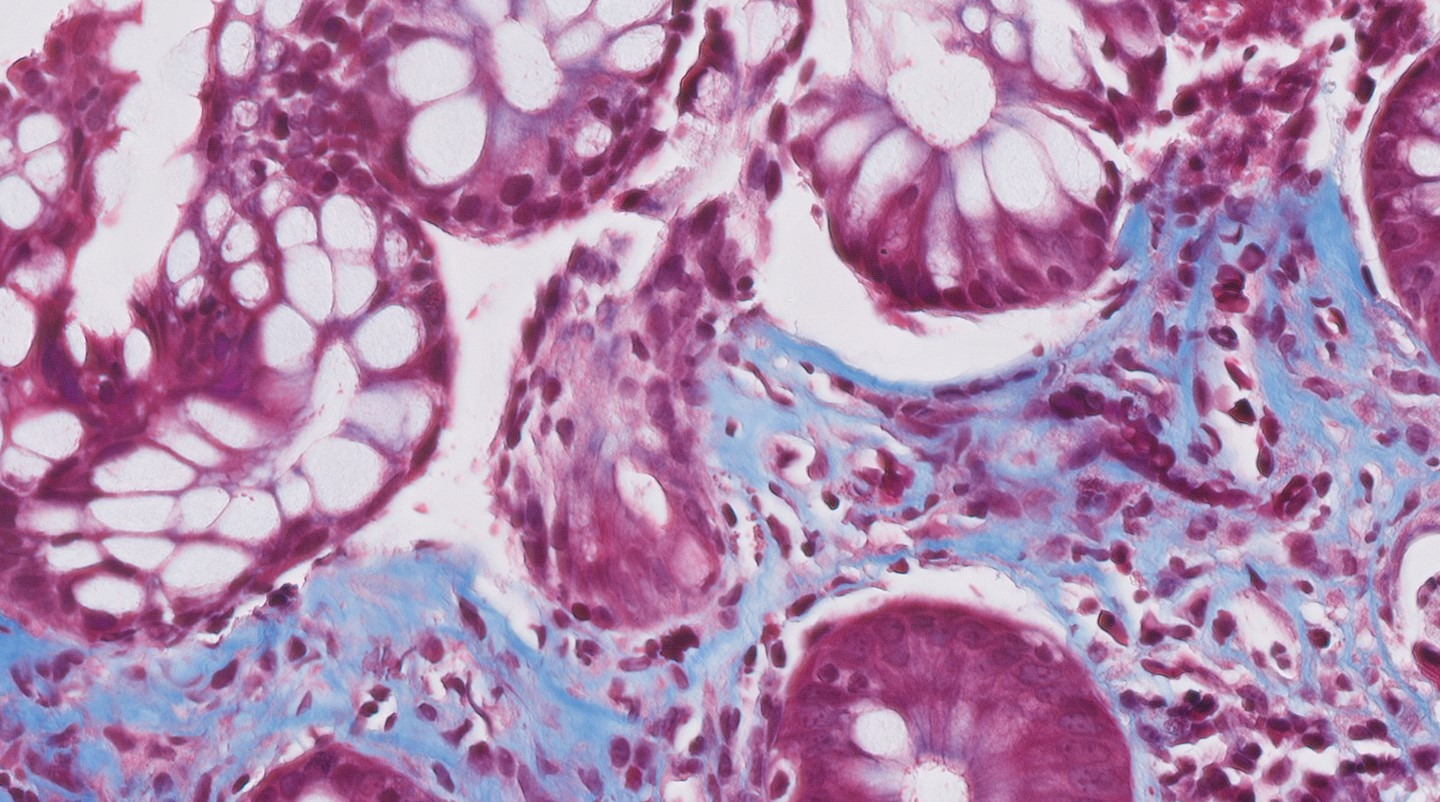
Figure: Figure 1a: Trichome stain, 20x magnification showing a thickened subepithelial collagen band.
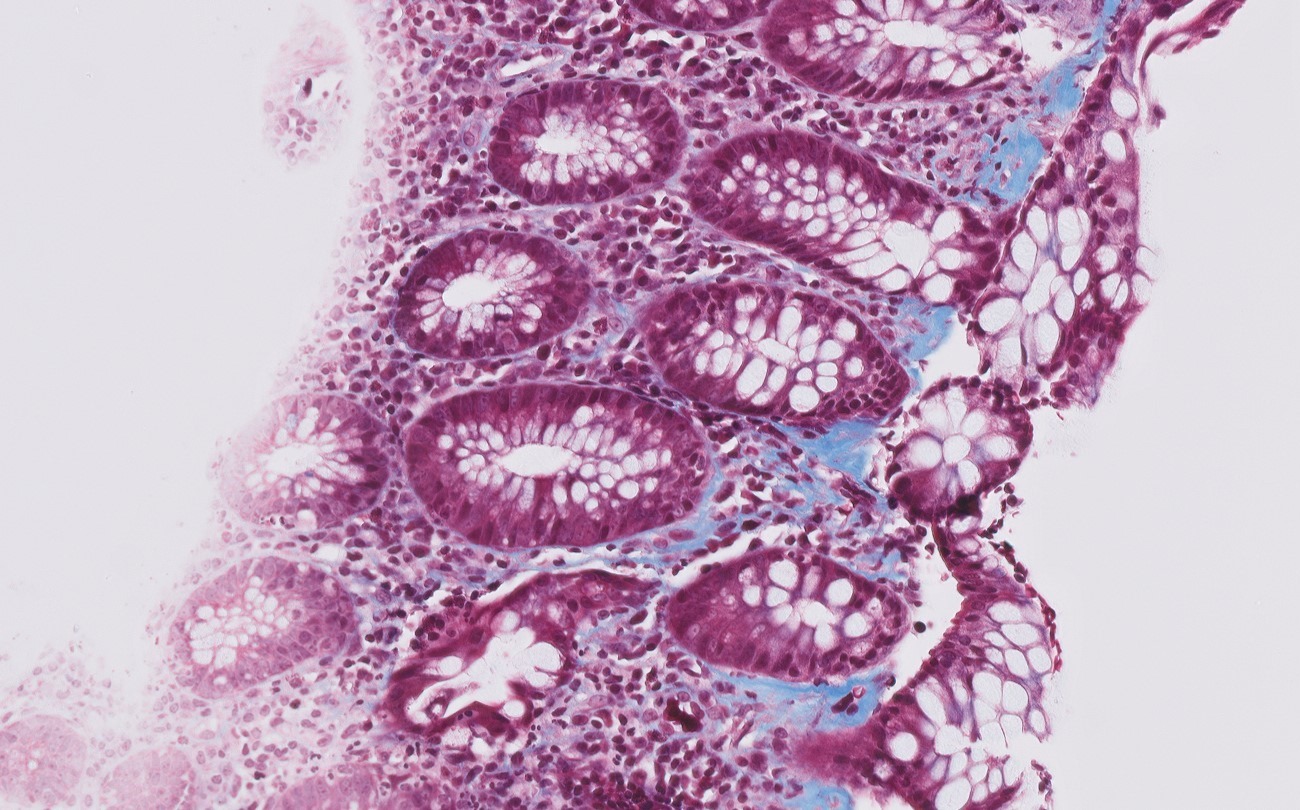
Figure: Figure 1b: Trichome stain, 40x magnification demonstrating collagen band around small capillaries. Notably, there is no significant increase in intraepithelial lymphocytes that are typically seen in CC.
Disclosures:
Amy Yeung indicated no relevant financial relationships.
Sugandha Bollu indicated no relevant financial relationships.
Elizabeth Eapen indicated no relevant financial relationships.
Sita Chokhavatia indicated no relevant financial relationships.
Amy Yeung, DO1, Sugandha Bollu, BA2, Elizabeth Eapen, MD1, Sita Chokhavatia, MD, MACG1. P0362 - Delayed Diagnosis of Collagenous Colitis in a Young Woman With Prior SARS-CoV-2 Infection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
