Sunday Poster Session
Category: Colon
P0457 - Doing Something When There Is Nothing — A Case of Colonic Pseudo-Obstruction
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Angiela Sivakumar, MD
Midwestern University
Mesa, AZ
Presenting Author(s)
Angiela Sivakumar, MD1, Howard Chung, MD1, Jae Kim, MD2
1Midwestern University, Mesa, AZ; 2Mountain Vista Medical Center, Mesa, AZ
Introduction: Colonic pseudo-obstruction refers to intestinal dysmotility in the absence of a mechanical cause that results in signs, symptoms, and imaging typically found in the setting of bowel obstruction. Here, we present a case of a geriatric patient suspected to have colonic blockage from a structural etiology with endoscopy revealing lack thereof.
Case Description/
Methods: An 80 year old male with history of squamous cell carcinoma s/p Mohs surgery + chemotherapy + immunotherapy, coronary artery disease and myocardial infarction s/p 3 stents, SBO s/p lysis of adhesions, tubular adenoma, diabetes with neuropathy, degenerative joint disease, and depression presented with severe abdominal pain + distention and no bowel movement or flatus x 1 week. Initial Contrast CT A/P was reported as diffuse descending colon wall thickening suggestive of colitis, though review of images yielded diffuse bowel dilation concerning for obstruction. General Surgery was consulted and ordered a repeat study with rectal contrast which was read as 1) interval opening of large bowel obstruction transition point in the proximal sigmoid at the left lower abdomen 2) interval mildly progressive distention of the transverse and ascending colon 3) interval development of mild fluid distention along the mid to distal small bowel loops. Labs on admission were all within normal limits. Physical exam was pertinent for severely distended abdomen with high-pitched, tinkling bowel sounds.
GI was consulted for colonoscopy and possible colonic stent. The entire colon was significantly dilated endoscopically, but no stricture was seen. A colonic decompression tube was placed, traversing cecum to anus. Patient underwent decompression with this and NGT x 4 days with 1500-2700 mL output each day. In this time, he had liquid bowel movements with labs notable for hypokalemia requiring repletion. Spouse brought in his medication list including opioids and stimulant laxatives which were discontinued. Given improvement in clinical exam and appetite, he was started on a liquid diet which was advanced to regular before discharge.
Discussion: Treatment for colonic pseudo-obstruction may involve bowel rest, intravenous fluids, and decompression, which this patient received. It is also integral to correct electrolyte abnormalities and avoid agents which may adversely affect contractile tone and propulsion of the bowels. Neostigmine was deferred given cardiovascular comorbidities though can be used to increase colonic contractility and transit otherwise.
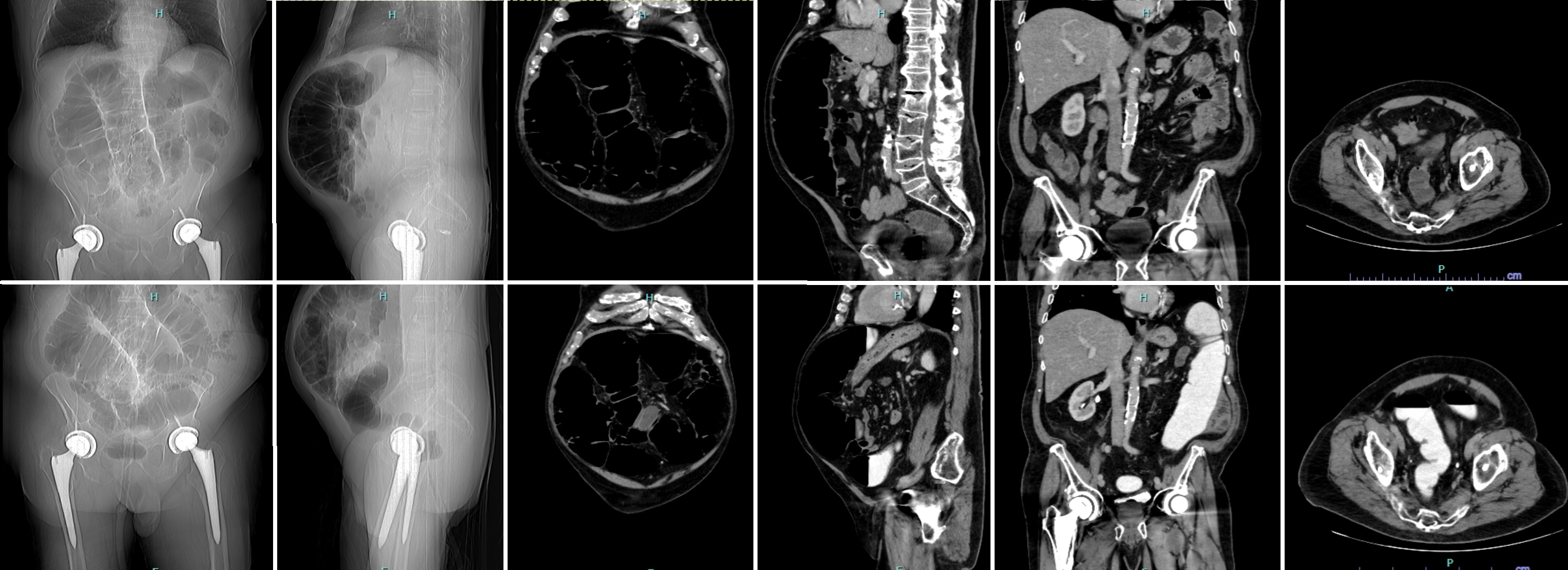
Figure: Figure 1: Initial CT Abdomen & Pelvis With IV Contrast (top row) Versus Repeat CT Abdomen & Pelvis With IV and Rectal Contrast (bottom row).
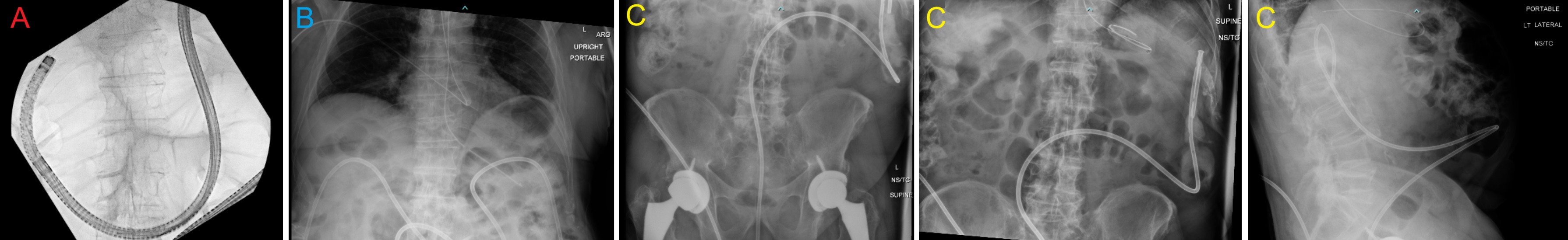
Figure: Figure 2: Colonoscopy and Post-Procedure Images. A) Colonoscope and wire over which colonic decompression tube was placed within the dilated colon, terminating in the cecum. B) KUB post-NGT insertion, demonstrating the presence of both decompressive tubes. C) Abdominal films done the day prior to discharge.
Disclosures:
Angiela Sivakumar indicated no relevant financial relationships.
Howard Chung indicated no relevant financial relationships.
Jae Kim indicated no relevant financial relationships.
Angiela Sivakumar, MD1, Howard Chung, MD1, Jae Kim, MD2. P0457 - Doing Something When There Is Nothing — A Case of Colonic Pseudo-Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Midwestern University, Mesa, AZ; 2Mountain Vista Medical Center, Mesa, AZ
Introduction: Colonic pseudo-obstruction refers to intestinal dysmotility in the absence of a mechanical cause that results in signs, symptoms, and imaging typically found in the setting of bowel obstruction. Here, we present a case of a geriatric patient suspected to have colonic blockage from a structural etiology with endoscopy revealing lack thereof.
Case Description/
Methods: An 80 year old male with history of squamous cell carcinoma s/p Mohs surgery + chemotherapy + immunotherapy, coronary artery disease and myocardial infarction s/p 3 stents, SBO s/p lysis of adhesions, tubular adenoma, diabetes with neuropathy, degenerative joint disease, and depression presented with severe abdominal pain + distention and no bowel movement or flatus x 1 week. Initial Contrast CT A/P was reported as diffuse descending colon wall thickening suggestive of colitis, though review of images yielded diffuse bowel dilation concerning for obstruction. General Surgery was consulted and ordered a repeat study with rectal contrast which was read as 1) interval opening of large bowel obstruction transition point in the proximal sigmoid at the left lower abdomen 2) interval mildly progressive distention of the transverse and ascending colon 3) interval development of mild fluid distention along the mid to distal small bowel loops. Labs on admission were all within normal limits. Physical exam was pertinent for severely distended abdomen with high-pitched, tinkling bowel sounds.
GI was consulted for colonoscopy and possible colonic stent. The entire colon was significantly dilated endoscopically, but no stricture was seen. A colonic decompression tube was placed, traversing cecum to anus. Patient underwent decompression with this and NGT x 4 days with 1500-2700 mL output each day. In this time, he had liquid bowel movements with labs notable for hypokalemia requiring repletion. Spouse brought in his medication list including opioids and stimulant laxatives which were discontinued. Given improvement in clinical exam and appetite, he was started on a liquid diet which was advanced to regular before discharge.
Discussion: Treatment for colonic pseudo-obstruction may involve bowel rest, intravenous fluids, and decompression, which this patient received. It is also integral to correct electrolyte abnormalities and avoid agents which may adversely affect contractile tone and propulsion of the bowels. Neostigmine was deferred given cardiovascular comorbidities though can be used to increase colonic contractility and transit otherwise.
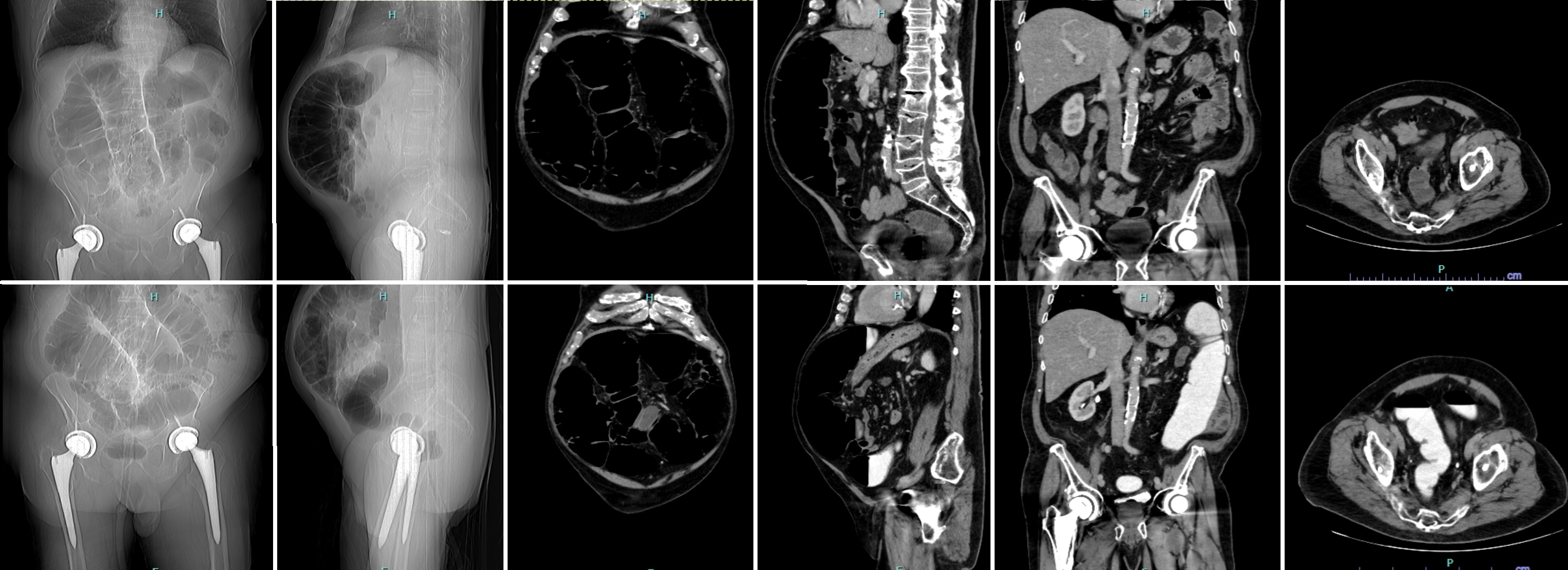
Figure: Figure 1: Initial CT Abdomen & Pelvis With IV Contrast (top row) Versus Repeat CT Abdomen & Pelvis With IV and Rectal Contrast (bottom row).
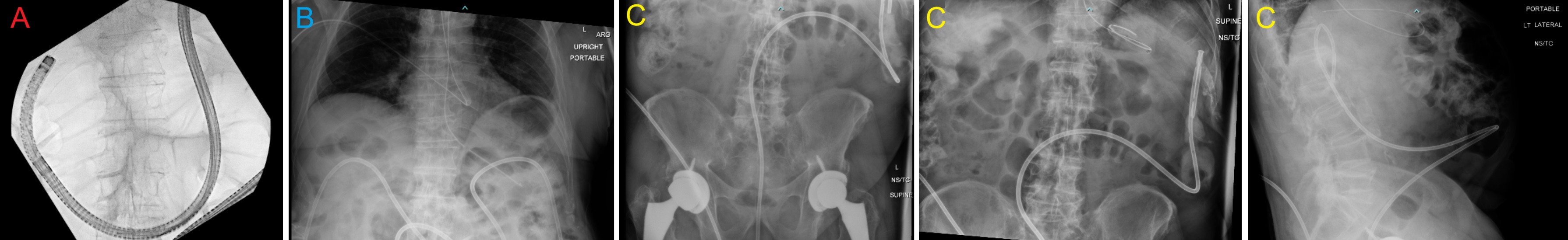
Figure: Figure 2: Colonoscopy and Post-Procedure Images. A) Colonoscope and wire over which colonic decompression tube was placed within the dilated colon, terminating in the cecum. B) KUB post-NGT insertion, demonstrating the presence of both decompressive tubes. C) Abdominal films done the day prior to discharge.
Disclosures:
Angiela Sivakumar indicated no relevant financial relationships.
Howard Chung indicated no relevant financial relationships.
Jae Kim indicated no relevant financial relationships.
Angiela Sivakumar, MD1, Howard Chung, MD1, Jae Kim, MD2. P0457 - Doing Something When There Is Nothing — A Case of Colonic Pseudo-Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
