Sunday Poster Session
Category: Colon
P0446 - Antibiotic-Induced Ischemic Colitis: A Case of Amoxicillin-Associated Vascular Compromise

Frank Lin, DO
St. Luke's University Health Network
Bethlehem, PA
Presenting Author(s)
1St. Luke's University Health Network, Easton, PA; 2St. Luke's University Health Network, Bethlehem, PA
Introduction: Ischemic colitis typically affects older adults and commonly involves watershed areas like the splenic flexure and sigmoid colon. Drug-induced cases are rare, and amoxicillin is not a well-known cause. We present a rare case of amoxicillin-associated ischemic colitis involving the hepatic flexure in a previously healthy middle-aged man.
Case Description/
Methods:
A 49-year-old male initially presented for nausea, vomiting, epigastric abdominal pain, and diarrhea with hematochezia. Prior to presentation, the patient had been taking amoxicillin for four days for antibiotic prophylaxis after a dental extraction. Stool studies and infectious work-up were unremarkable.
After his first episode of colitis with suspicion for possible infectious etiology, the patient was placed on amoxicillin-clavulanate despite unremarkable infectious work-up. He was subsequently re-admitted to the hospital with recurrent symptoms of hematochezia, diarrhea, abdominal pain, and vomiting. Clostridium difficile testing was negative during the second admission. An ultrasound of the celiac and mesenteric vessels showed patency of the celiac, super mesenteric, inferior mesenteric, splenic, and common hepatic arteries. CT angiography of the abdomen and pelvis showed acute severe colitis with involvement of the rectosigmoid colon, which was spared on CT angiography during the initial admission.
Colonoscopy showed severe edematous and ulcerated mucosa with loss of vascular pattern in the hepatic flexure consistent with ischemic colitis (Figure 1). Biopsy of the colonic mucosa at the hepatic flexure was compatible with ischemic-type mucosal injury and colitis without evidence for dysplasia or malignancy (Figures 2). Autoimmune work-up was entirely unremarkable, hence there was low concern for vasculitis. A three-month follow-up colonoscopy showed complete resolution of ischemic colitis.
Discussion: Amoxicillin-clavulanate induced ischemic colitis is a rare condition and a diagnosis of exclusion after ruling out other etiologies including prothrombotic and hypercoagulable states, vascular compromise, sepsis, heart failure, vasculitis, infectious colitis, and inflammatory bowel disease. Ischemia is more common in watershed areas of the colon including the splenic flexure and sigmoid colon due to the dual blood supply in these regions, making involvement of the hepatic flexure much less common for ischemia. The increased use of antibiotics should prompt the inclusion of this condition to the differentials for ischemic colitis.
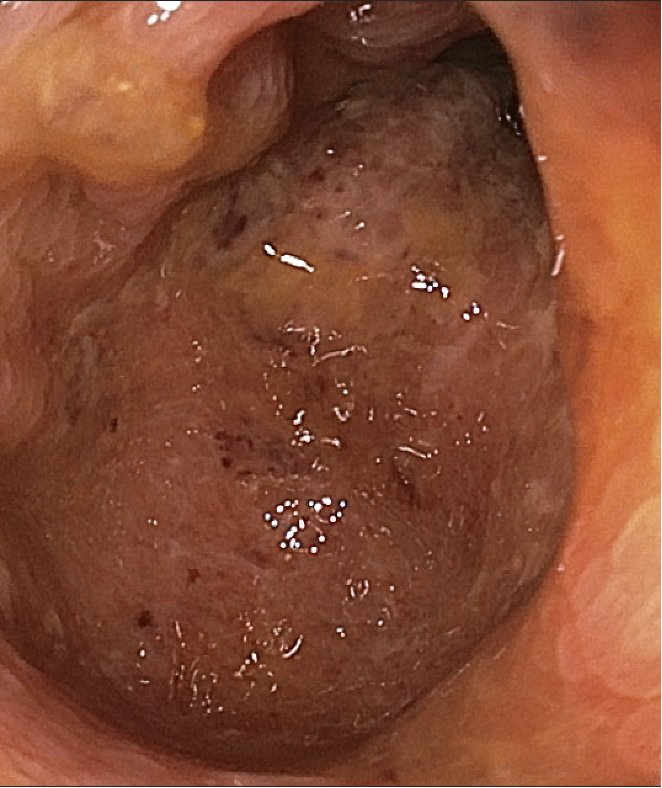
Figure: Figure 1. Colonoscopy showing severe edematous and ulcerated mucosa with loss of vascular pattern in the hepatic flexure consistent with ischemic colitis.

Figure: Figure 2. Early ischemic changes including mucosal edema, denudation (*) and vascular congestion (arrows) in top image. 10x: Acute inflammatory exudate (pseudomembranes) on the mucosa (*), superficial mucosal damage (arrows) with underlying crypt dropout (withering) in middle image. 20x: Acute inflammatory exudate (*) on the mucosa, mucosal surface damage, lamina propria hyalinization, mucosal necrosis and vascular congestion in bottom image.
Disclosures:
Frank Lin indicated no relevant financial relationships.
Ayah Obeid indicated no relevant financial relationships.
Anuraag Bandi indicated no relevant financial relationships.
Russell Plowman indicated no relevant financial relationships.
Loveleen Sidhu indicated no relevant financial relationships.
Rajesh Kuppuraju indicated no relevant financial relationships.
Frank Lin, DO1, Ayah Obeid, MD1, Anuraag Bandi, MD1, Russell Plowman, MD2, Loveleen Sidhu, MD1, Rajesh Kuppuraju, DO1. P0446 - Antibiotic-Induced Ischemic Colitis: A Case of Amoxicillin-Associated Vascular Compromise, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
