Sunday Poster Session
Category: Diet, Nutrition, and Obesity
P0540 - Micronutrient Sufficiency in Inflammatory Bowel Disease: A Cross-Sectional Study of Dietary Intake and Clinical Predictors
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Angela Minasyan, BS
David Geffen School of Medicine at UCLA
Los Angeles, CA
Presenting Author(s)
Angela Minasyan, BS, Jia Hui Hai, , Jaden Nguyen, , Brendan Field, , Sureya Hussani, MD, Christina Fasulo, MS, RD, Berkeley Limketkai, MD, PhD
David Geffen School of Medicine at UCLA, Los Angeles, CA
Introduction: Micronutrient deficiencies are frequently observed in patients with inflammatory bowel disease (IBD) and are driven by malabsorption, inflammation, and dietary restriction. Our study aims to assess the prevalence of adequate dietary micronutrient intake in patients with IBD, while also examining the impact of clinical and treatment-related predictors on nutritional adequacy.
Methods: We conducted a cross-sectional study of patients with confirmed IBD who received care at a tertiary care gastroenterology clinic. All participants completed a validated dietary intake survey. Individual micronutrient intake levels were compared to age- and sex-specific Recommended Dietary Allowances (RDA) published by the Institute of Medicine. Micronutrient adequacy was compared across IBD types and states of disease activity. Multivariable linear regression examined the association between different clinical factors and the number of micronutrients for which a patient met the RDA.
Results: Of the 279 patients who met our inclusion criteria, 148 (53.0%) participants had ulcerative colitis and 131 (47.0%) had Crohn’s disease. The mean age was 36.0 ± 15.1 years and 145 (52.0%) were female. Based on the RDA, the most common micronutrients with insufficient dietary intake included vitamin D (92.1%), vitamin E (77.4%), zinc (66.3%), vitamin A (62.7%), and folate (59.1%). The least common micronutrients with insufficient dietary intake were niacin (31.9%), riboflavin (28.0%), pyridoxine (25.4%), copper (24.0%), and vitamin B12 (20.4%). Although there was no difference in micronutrient intake when comparing IBD types, being in clinical remission (asymptomatic) was significantly associated with higher intake of vitamin K (p=0.037), zinc (p=0.027), and folate (p=0.023), but lower intake of vitamin D (p=0.009) (Figure). In multivariable regression, being in clinical remission was associated with a greater number of these micronutrients meeting RDA (β=0.32; 95% CI: 0.01–0.62; p=0.045).
Discussion: Inadequate dietary intake of micronutrients remains highly prevalent among patients with IBD, while further aggravated by active disease. These findings support regular dietary and biochemical screening in IBD care, particularly among micronutrients that are more commonly to be inadequately consumed (e.g., vitamin D, vitamin E, zinc, vitamin A, folate). Future efforts should explore malabsorption, supplement adherence, and dietary restriction to guide targeted interventions.
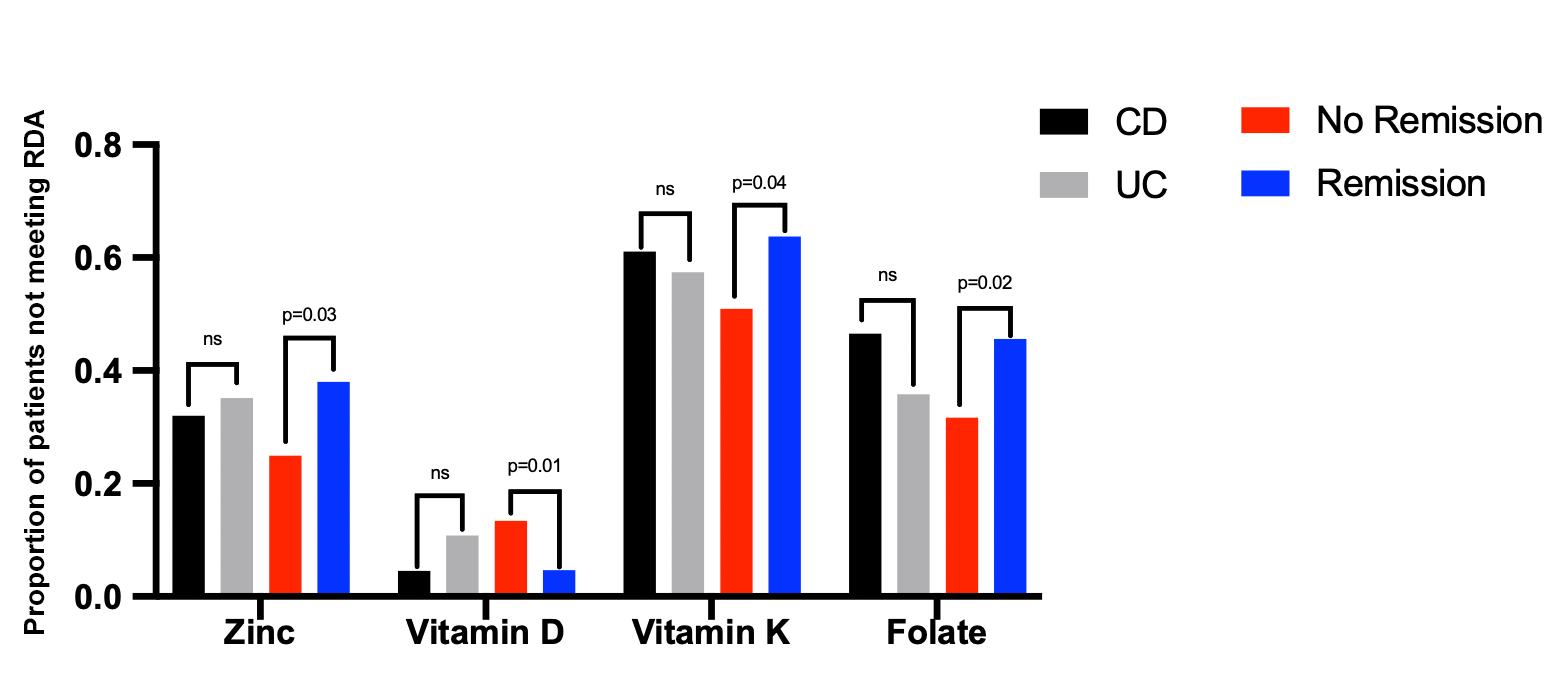
Figure: Adequate dietary intake of select micronutrients, stratified by IBD type or disease activity
Disclosures:
Angela Minasyan indicated no relevant financial relationships.
Jia Hui Hai indicated no relevant financial relationships.
Jaden Nguyen indicated no relevant financial relationships.
Brendan Field indicated no relevant financial relationships.
Sureya Hussani indicated no relevant financial relationships.
Christina Fasulo: Ironwood Pharmaceuticals – Consultant.
Berkeley Limketkai: Azora Therapeutics – Consultant, Stock-privately held company. Johnson & Johnson – Advisory Committee/Board Member, Speakers Bureau.
Angela Minasyan, BS, Jia Hui Hai, , Jaden Nguyen, , Brendan Field, , Sureya Hussani, MD, Christina Fasulo, MS, RD, Berkeley Limketkai, MD, PhD. P0540 - Micronutrient Sufficiency in Inflammatory Bowel Disease: A Cross-Sectional Study of Dietary Intake and Clinical Predictors, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
David Geffen School of Medicine at UCLA, Los Angeles, CA
Introduction: Micronutrient deficiencies are frequently observed in patients with inflammatory bowel disease (IBD) and are driven by malabsorption, inflammation, and dietary restriction. Our study aims to assess the prevalence of adequate dietary micronutrient intake in patients with IBD, while also examining the impact of clinical and treatment-related predictors on nutritional adequacy.
Methods: We conducted a cross-sectional study of patients with confirmed IBD who received care at a tertiary care gastroenterology clinic. All participants completed a validated dietary intake survey. Individual micronutrient intake levels were compared to age- and sex-specific Recommended Dietary Allowances (RDA) published by the Institute of Medicine. Micronutrient adequacy was compared across IBD types and states of disease activity. Multivariable linear regression examined the association between different clinical factors and the number of micronutrients for which a patient met the RDA.
Results: Of the 279 patients who met our inclusion criteria, 148 (53.0%) participants had ulcerative colitis and 131 (47.0%) had Crohn’s disease. The mean age was 36.0 ± 15.1 years and 145 (52.0%) were female. Based on the RDA, the most common micronutrients with insufficient dietary intake included vitamin D (92.1%), vitamin E (77.4%), zinc (66.3%), vitamin A (62.7%), and folate (59.1%). The least common micronutrients with insufficient dietary intake were niacin (31.9%), riboflavin (28.0%), pyridoxine (25.4%), copper (24.0%), and vitamin B12 (20.4%). Although there was no difference in micronutrient intake when comparing IBD types, being in clinical remission (asymptomatic) was significantly associated with higher intake of vitamin K (p=0.037), zinc (p=0.027), and folate (p=0.023), but lower intake of vitamin D (p=0.009) (Figure). In multivariable regression, being in clinical remission was associated with a greater number of these micronutrients meeting RDA (β=0.32; 95% CI: 0.01–0.62; p=0.045).
Discussion: Inadequate dietary intake of micronutrients remains highly prevalent among patients with IBD, while further aggravated by active disease. These findings support regular dietary and biochemical screening in IBD care, particularly among micronutrients that are more commonly to be inadequately consumed (e.g., vitamin D, vitamin E, zinc, vitamin A, folate). Future efforts should explore malabsorption, supplement adherence, and dietary restriction to guide targeted interventions.
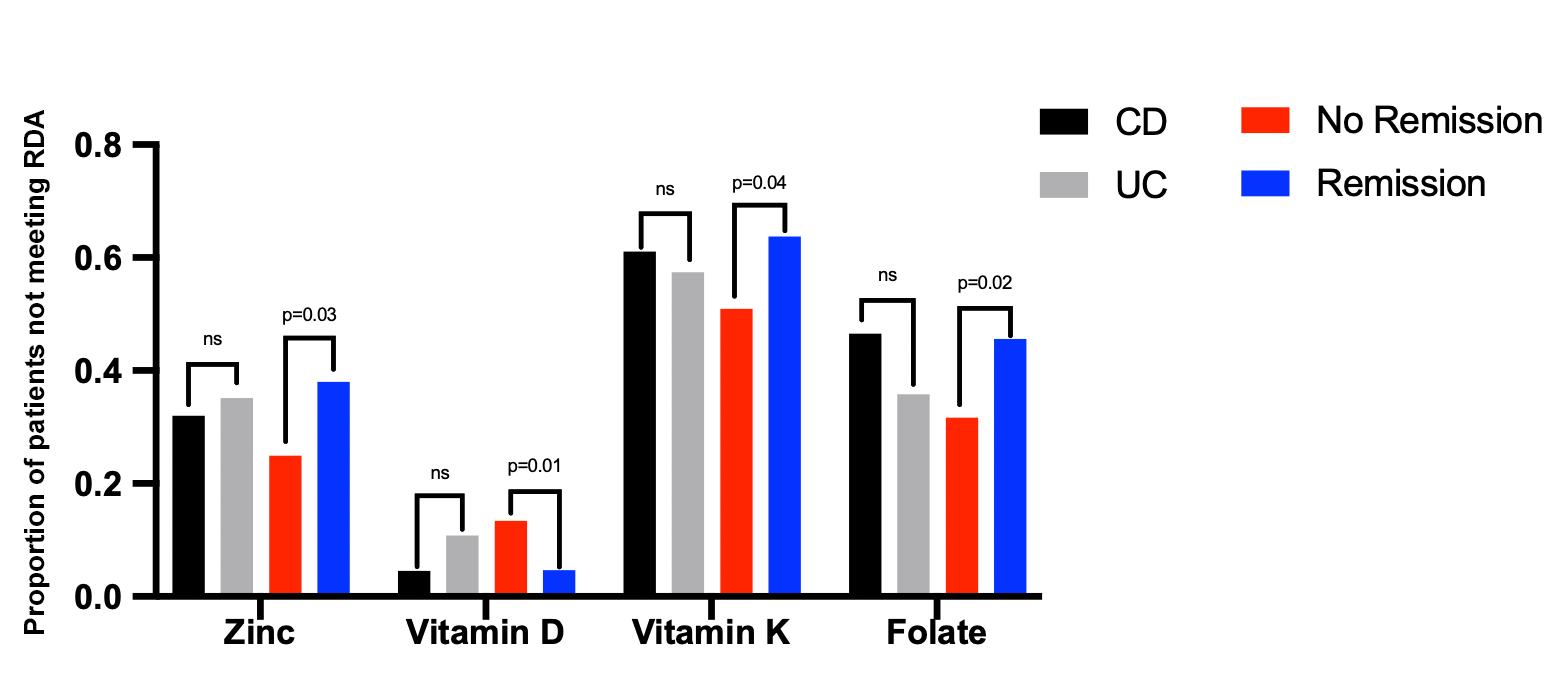
Figure: Adequate dietary intake of select micronutrients, stratified by IBD type or disease activity
Disclosures:
Angela Minasyan indicated no relevant financial relationships.
Jia Hui Hai indicated no relevant financial relationships.
Jaden Nguyen indicated no relevant financial relationships.
Brendan Field indicated no relevant financial relationships.
Sureya Hussani indicated no relevant financial relationships.
Christina Fasulo: Ironwood Pharmaceuticals – Consultant.
Berkeley Limketkai: Azora Therapeutics – Consultant, Stock-privately held company. Johnson & Johnson – Advisory Committee/Board Member, Speakers Bureau.
Angela Minasyan, BS, Jia Hui Hai, , Jaden Nguyen, , Brendan Field, , Sureya Hussani, MD, Christina Fasulo, MS, RD, Berkeley Limketkai, MD, PhD. P0540 - Micronutrient Sufficiency in Inflammatory Bowel Disease: A Cross-Sectional Study of Dietary Intake and Clinical Predictors, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

