Sunday Poster Session
Category: Esophagus
P0620 - Endoscopic Incisional Therapy for Benign Esophageal Strictures: A Systematic Review and Meta-Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Kobina Essilfie-Quaye, MD (he/him/his)
University of Central Florida, HCA Healthcare GME
Gainesville, FL
Presenting Author(s)
Kobina Essilfie-Quaye, MD1, Yizhong Wu, MD2, Andrew Ofosu, MD, MPH3, John Fang, MD4, Daryl Ramai, MD, MPH, MSc5
1University of Central Florida, HCA Healthcare GME, Gainesville, FL; 2Baylor Scott & White, Georgetown, TX; 3University of Colorado, Colorado, OH; 4University of Utah, Salt Lake City, UT; 5Brigham and Women’s Hospital, Harvard Medical School, Salt Lake City, UT
Introduction: Benign esophageal strictures (BES) are a significant source of morbidity, particularly in patients who fail to respond to conventional endoscopic dilation. Endoscopic Incisional Therapy (EIT) is a minimally invasive alternative, but its effectiveness, durability, and safety profile remain incompletely characterized. The objective of this systematic review and meta-analysis was to evaluate the efficacy and safety of EIT in the treatment of BES.
Methods: A systematic literature search was conducted in accordance with the PRISMA 2020 guidelines. The databases searched included PubMed, EMBASE, Cochrane Library, and Google Scholar. Studies were eligible for inclusion if they involved human subjects undergoing EIT for BES and reported relevant outcome data. Outcomes analyzed included technical success, clinical success at 1, 6, 12, and 24 months, recurrence, and adverse events. Pooled proportion estimates were calculated using the Freeman–Tukey double arcsine transformation and a random-effects model to account for study variability. Subgroup analyses were performed based on stricture type, comparing naïve versus refractory strictures.
Results: Fourteen studies comprising 396 patients were included. The pooled technical success rate was 99.0% (95% CI: 97.8%–99.8%; I² = 0%). Clinical success rates declined over time, with pooled proportions of: 88.7% at 1 month (95% CI: 75.5%–97.2%; I² = 60.9%), 63.6% at 6 months (95% CI: 48.6%–77.5%; I² = 84.2%), 52.0% at 12 months (95% CI: 35.7%–68.1%; I² = 78.4%), and 61.6% at 24 months (95% CI: 22.3%–93.5%; I² = 92.5%). Subgroup analysis by stricture type revealed greater efficacy of EIT in naive strictures, with a pooled clinical success rate of 77.1% (95% CI: 59.5%–90.8%; I² = 60.8%) at 12–24 months. In contrast, refractory strictures demonstrated a significantly lower success rate of 46.6% (95% CI: 24.8%–69.0%; I² = 87.3%) over the same interval. Adverse events were uncommon and included a small perforation, minor bleeding, pain, and fever, most of which were managed conservatively without surgical intervention. No procedure-related mortality was reported.
Discussion: EIT appears to be a highly effective and relatively safe treatment modality for benign esophageal strictures. It demonstrates excellent short-term clinical outcomes and a favorable safety profile, although long-term efficacy may decline, particularly in patients with refractory strictures.
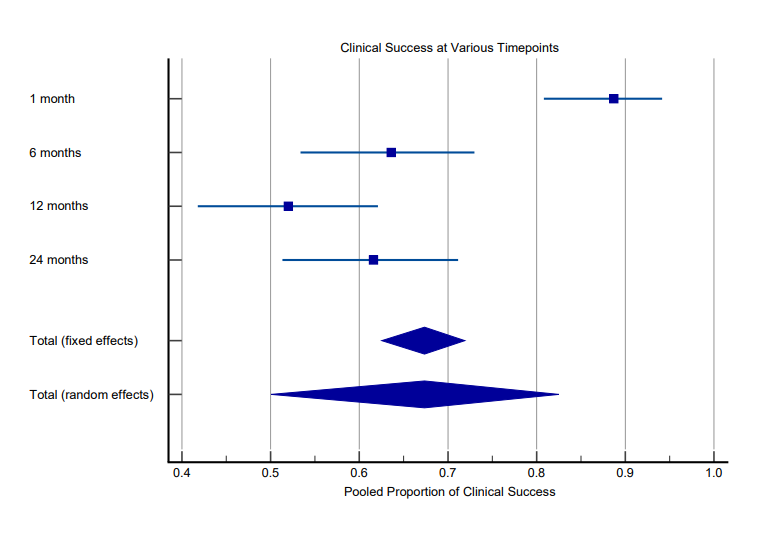
Figure: Forest plot displaying pooled proportions of clinical success at various follow-up timepoints (1, 6, 12, and 24 months).
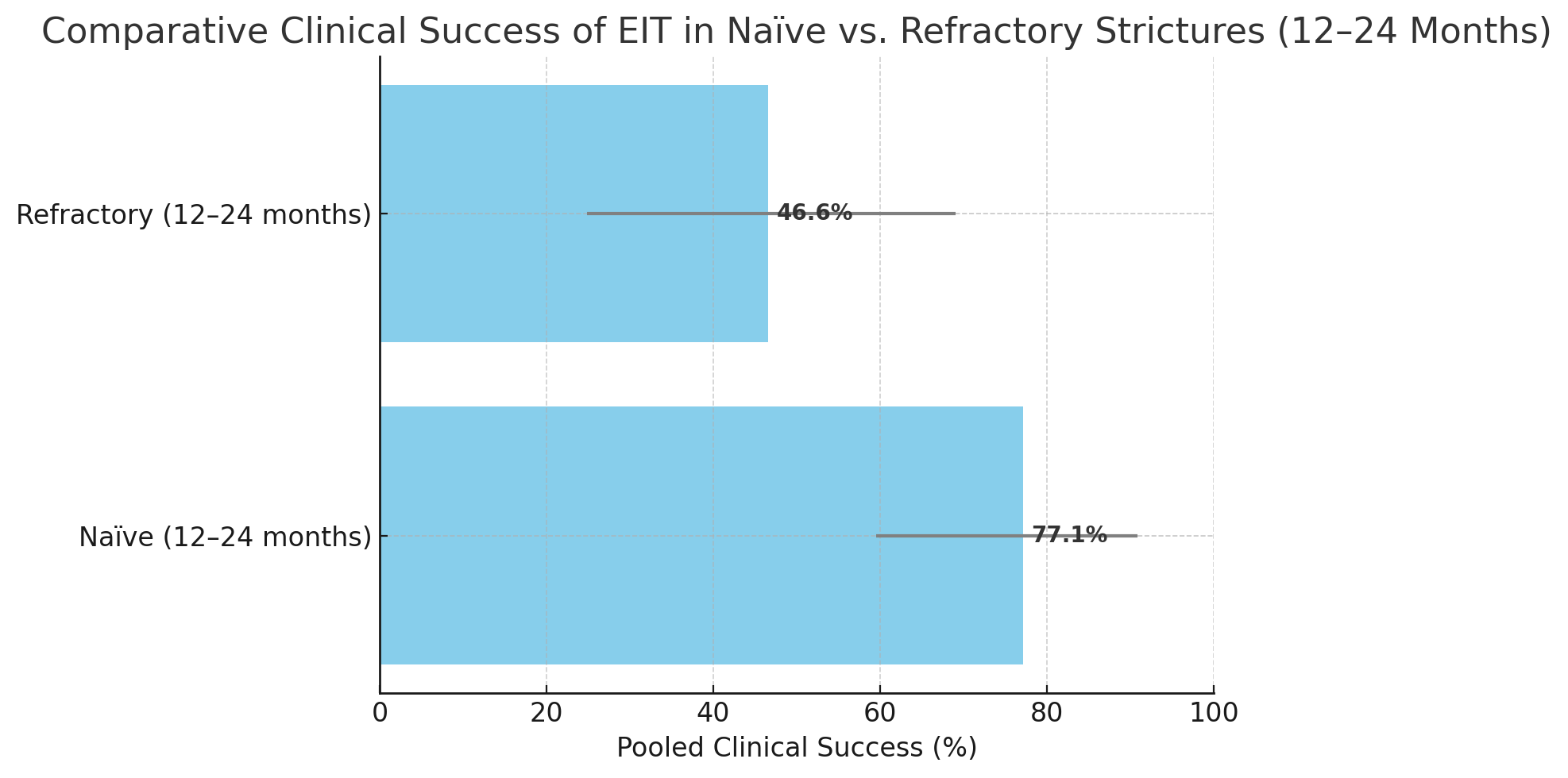
Figure: Comparative Clinical Success of EIT in Naive vs Refractory Strictures (12-24 Months)
Disclosures:
Kobina Essilfie-Quaye indicated no relevant financial relationships.
Yizhong Wu indicated no relevant financial relationships.
Andrew Ofosu indicated no relevant financial relationships.
John Fang: Aspero Medical – Consultant. Circa Scientific – Consultant. Merit – Consultant.
Daryl Ramai indicated no relevant financial relationships.
Kobina Essilfie-Quaye, MD1, Yizhong Wu, MD2, Andrew Ofosu, MD, MPH3, John Fang, MD4, Daryl Ramai, MD, MPH, MSc5. P0620 - Endoscopic Incisional Therapy for Benign Esophageal Strictures: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Central Florida, HCA Healthcare GME, Gainesville, FL; 2Baylor Scott & White, Georgetown, TX; 3University of Colorado, Colorado, OH; 4University of Utah, Salt Lake City, UT; 5Brigham and Women’s Hospital, Harvard Medical School, Salt Lake City, UT
Introduction: Benign esophageal strictures (BES) are a significant source of morbidity, particularly in patients who fail to respond to conventional endoscopic dilation. Endoscopic Incisional Therapy (EIT) is a minimally invasive alternative, but its effectiveness, durability, and safety profile remain incompletely characterized. The objective of this systematic review and meta-analysis was to evaluate the efficacy and safety of EIT in the treatment of BES.
Methods: A systematic literature search was conducted in accordance with the PRISMA 2020 guidelines. The databases searched included PubMed, EMBASE, Cochrane Library, and Google Scholar. Studies were eligible for inclusion if they involved human subjects undergoing EIT for BES and reported relevant outcome data. Outcomes analyzed included technical success, clinical success at 1, 6, 12, and 24 months, recurrence, and adverse events. Pooled proportion estimates were calculated using the Freeman–Tukey double arcsine transformation and a random-effects model to account for study variability. Subgroup analyses were performed based on stricture type, comparing naïve versus refractory strictures.
Results: Fourteen studies comprising 396 patients were included. The pooled technical success rate was 99.0% (95% CI: 97.8%–99.8%; I² = 0%). Clinical success rates declined over time, with pooled proportions of: 88.7% at 1 month (95% CI: 75.5%–97.2%; I² = 60.9%), 63.6% at 6 months (95% CI: 48.6%–77.5%; I² = 84.2%), 52.0% at 12 months (95% CI: 35.7%–68.1%; I² = 78.4%), and 61.6% at 24 months (95% CI: 22.3%–93.5%; I² = 92.5%). Subgroup analysis by stricture type revealed greater efficacy of EIT in naive strictures, with a pooled clinical success rate of 77.1% (95% CI: 59.5%–90.8%; I² = 60.8%) at 12–24 months. In contrast, refractory strictures demonstrated a significantly lower success rate of 46.6% (95% CI: 24.8%–69.0%; I² = 87.3%) over the same interval. Adverse events were uncommon and included a small perforation, minor bleeding, pain, and fever, most of which were managed conservatively without surgical intervention. No procedure-related mortality was reported.
Discussion: EIT appears to be a highly effective and relatively safe treatment modality for benign esophageal strictures. It demonstrates excellent short-term clinical outcomes and a favorable safety profile, although long-term efficacy may decline, particularly in patients with refractory strictures.
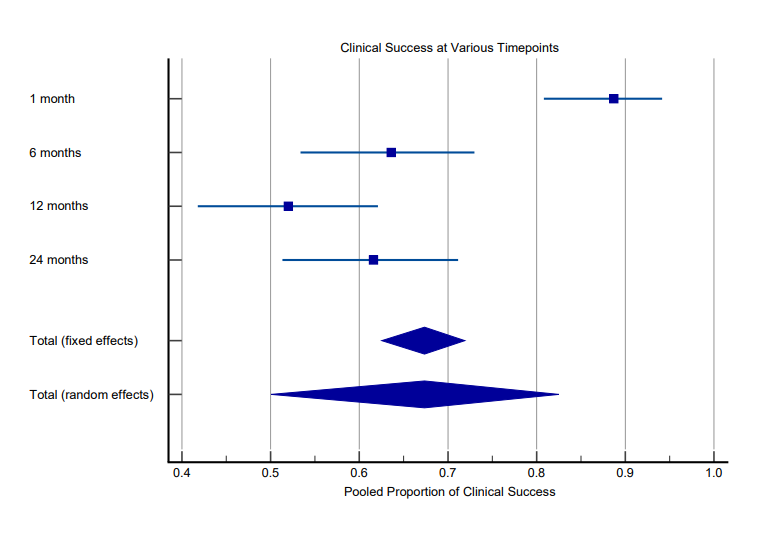
Figure: Forest plot displaying pooled proportions of clinical success at various follow-up timepoints (1, 6, 12, and 24 months).
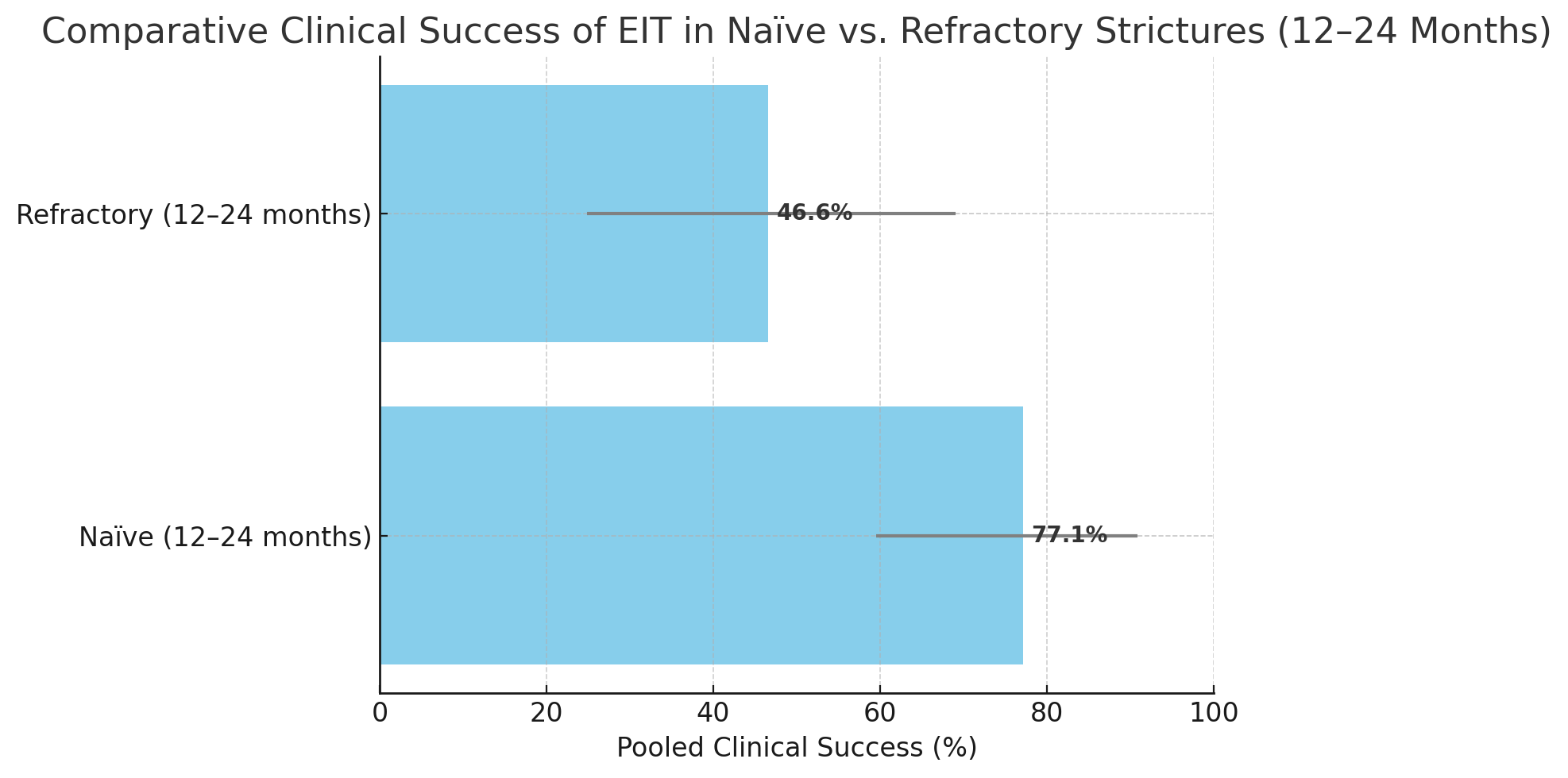
Figure: Comparative Clinical Success of EIT in Naive vs Refractory Strictures (12-24 Months)
Disclosures:
Kobina Essilfie-Quaye indicated no relevant financial relationships.
Yizhong Wu indicated no relevant financial relationships.
Andrew Ofosu indicated no relevant financial relationships.
John Fang: Aspero Medical – Consultant. Circa Scientific – Consultant. Merit – Consultant.
Daryl Ramai indicated no relevant financial relationships.
Kobina Essilfie-Quaye, MD1, Yizhong Wu, MD2, Andrew Ofosu, MD, MPH3, John Fang, MD4, Daryl Ramai, MD, MPH, MSc5. P0620 - Endoscopic Incisional Therapy for Benign Esophageal Strictures: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

