Sunday Poster Session
Category: Esophagus
P0611 - Gluca-Gone: Role in Esophageal Food Bolus Obstruction
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- RM
Raakhi Menon, DO
University of Texas Medical Branch
Galveston, TX
Presenting Author(s)
Raakhi Menon, DO1, Kian Abdul-Baki, DO2, Muhammad Mushtaq, DO1, Anirudha Chatterjee, MD1, Eric Margulies, MD1, Brooke Corning, MD1
1University of Texas Medical Branch, Galveston, TX; 2University of Texas Medical Branch at Galveston, Galveston, TX
Introduction: Esophageal food bolus impactions are medical emergencies that require prompt endoscopic intervention. Current guidelines from the American Society for Gastrointestinal Endoscopy recommend performing esophagogastroduodenoscopy (EGD) within 24 hours to optimize outcomes and minimize risks, advising against significant delays for pharmacologic trials. This study aimed to assess the impact of glucagon administration on EGD duration, along with the influence of demographic factors, social history, body mass index (BMI), nonsteroidal anti-inflammatory drug (NSAID) use, and gastroesophageal reflux disease (GERD) history.
Methods: A retrospective chart review was conducted at a tertiary care center, identifying cases via ICD-10 codes for EGD with foreign body removal between 1/1/2018 and 11/20/2023. Exclusions included cases without food impaction, no EGD performed, transfers from outside hospitals, or incidental findings during unrelated EGDs. Of 448 procedures, 220 met inclusion criteria for final analysis.
Results: The median patient age was 58 years (IQR 44–70), with 149 males and 182 identifying as Caucasian. Median BMI was 27.93 (IQR 24.18–31.41). GERD was present in 109 patients; 71 had prior food bolus impactions, 95 reported alcohol use, 62 tobacco use, and 34 used NSAIDs. Glucagon was administered to 157 patients but showed no significant effect on EGD duration (p=0.343), with average procedure times of 39:16 without glucagon vs. 30:19 with it. BMI, GERD, alcohol, and NSAID use did not impact procedure length. However, tobacco use significantly prolonged EGD duration (p=0.025), averaging 37:53 vs. 30:19 in non-smokers.
Discussion: Glucagon, a pharmacologic agent that relaxes the smooth muscle at the lower esophageal sphincter, may facilitate the passage of food bolus impactions. However, it may not address underlying etiologies, such as structural abnormalities or eosinophilic esophagitis. This study found no statistically significant difference in EGD duration between patients who received glucagon and those who did not. Notably, tobacco use was associated with longer EGD durations, suggesting potential physiological or anatomical factors influencing endoscopic procedures in this population. Limitations include unmeasured pre-existing conditions that may have affected glucagon’s efficacy and the exclusion of patients whose food impactions resolved with glucagon and therefore did not require EGD.
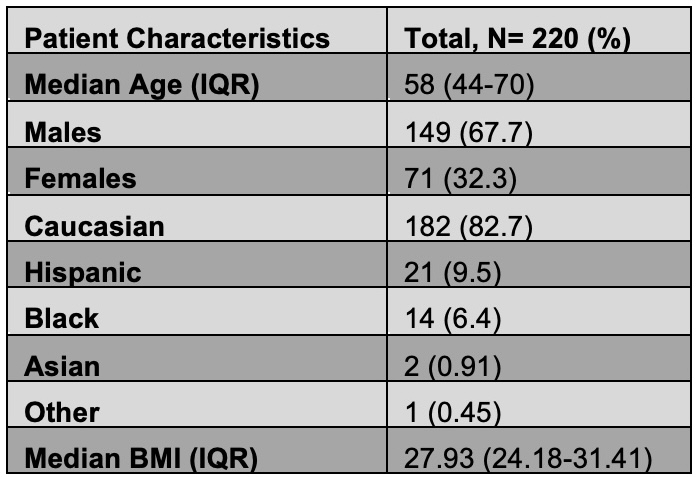
Figure: Table 1: Patient Characteristics
Disclosures:
Raakhi Menon indicated no relevant financial relationships.
Kian Abdul-Baki indicated no relevant financial relationships.
Muhammad Mushtaq indicated no relevant financial relationships.
Anirudha Chatterjee indicated no relevant financial relationships.
Eric Margulies indicated no relevant financial relationships.
Brooke Corning indicated no relevant financial relationships.
Raakhi Menon, DO1, Kian Abdul-Baki, DO2, Muhammad Mushtaq, DO1, Anirudha Chatterjee, MD1, Eric Margulies, MD1, Brooke Corning, MD1. P0611 - Gluca-Gone: Role in Esophageal Food Bolus Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas Medical Branch, Galveston, TX; 2University of Texas Medical Branch at Galveston, Galveston, TX
Introduction: Esophageal food bolus impactions are medical emergencies that require prompt endoscopic intervention. Current guidelines from the American Society for Gastrointestinal Endoscopy recommend performing esophagogastroduodenoscopy (EGD) within 24 hours to optimize outcomes and minimize risks, advising against significant delays for pharmacologic trials. This study aimed to assess the impact of glucagon administration on EGD duration, along with the influence of demographic factors, social history, body mass index (BMI), nonsteroidal anti-inflammatory drug (NSAID) use, and gastroesophageal reflux disease (GERD) history.
Methods: A retrospective chart review was conducted at a tertiary care center, identifying cases via ICD-10 codes for EGD with foreign body removal between 1/1/2018 and 11/20/2023. Exclusions included cases without food impaction, no EGD performed, transfers from outside hospitals, or incidental findings during unrelated EGDs. Of 448 procedures, 220 met inclusion criteria for final analysis.
Results: The median patient age was 58 years (IQR 44–70), with 149 males and 182 identifying as Caucasian. Median BMI was 27.93 (IQR 24.18–31.41). GERD was present in 109 patients; 71 had prior food bolus impactions, 95 reported alcohol use, 62 tobacco use, and 34 used NSAIDs. Glucagon was administered to 157 patients but showed no significant effect on EGD duration (p=0.343), with average procedure times of 39:16 without glucagon vs. 30:19 with it. BMI, GERD, alcohol, and NSAID use did not impact procedure length. However, tobacco use significantly prolonged EGD duration (p=0.025), averaging 37:53 vs. 30:19 in non-smokers.
Discussion: Glucagon, a pharmacologic agent that relaxes the smooth muscle at the lower esophageal sphincter, may facilitate the passage of food bolus impactions. However, it may not address underlying etiologies, such as structural abnormalities or eosinophilic esophagitis. This study found no statistically significant difference in EGD duration between patients who received glucagon and those who did not. Notably, tobacco use was associated with longer EGD durations, suggesting potential physiological or anatomical factors influencing endoscopic procedures in this population. Limitations include unmeasured pre-existing conditions that may have affected glucagon’s efficacy and the exclusion of patients whose food impactions resolved with glucagon and therefore did not require EGD.
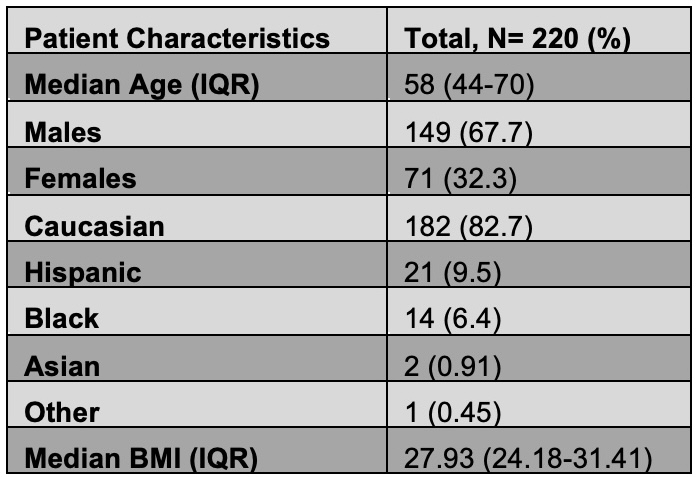
Figure: Table 1: Patient Characteristics
Disclosures:
Raakhi Menon indicated no relevant financial relationships.
Kian Abdul-Baki indicated no relevant financial relationships.
Muhammad Mushtaq indicated no relevant financial relationships.
Anirudha Chatterjee indicated no relevant financial relationships.
Eric Margulies indicated no relevant financial relationships.
Brooke Corning indicated no relevant financial relationships.
Raakhi Menon, DO1, Kian Abdul-Baki, DO2, Muhammad Mushtaq, DO1, Anirudha Chatterjee, MD1, Eric Margulies, MD1, Brooke Corning, MD1. P0611 - Gluca-Gone: Role in Esophageal Food Bolus Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
