Sunday Poster Session
Category: Esophagus
P0609 - Bariatric Surgery Nearly Doubles 5-Year Reflux and Barrett’s Risk versus GLP-1 Agonists: A Propensity-Matched, 81 410-Patient Cohort Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Himsikhar Khataniar, MD (he/him/his)
Allegheny General Hospital
Pittsburgh, PA
Presenting Author(s)
Himsikhar Khataniar, MD1, Sameer Rao, MBBS2, Hany Habib, MD3, Rahul Karna, MD4, Shifa Umar, MD5
1Allegheny General Hospital, Pittsburgh, PA; 2Rutgers New Jersey Medical School, Newark, NJ; 3Allegheny Health Network Medicine Institute, Pittsburgh, PA; 4University of Minnesota Medical Center, Minneapolis, MN; 5Baylor College of Medicine, Houston, TX
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) have emerged as a pharmacologic alternative to bariatric surgery (BS) for weight reduction after U.S. Food and Drug Administration approval for obesity. Delayed gastric emptying with GLP-1 RAs and anatomic disruption after BS may each predispose to new onset esophageal disorders.
Methods: Using the TriNetX U.S. Collaborative Network, we identified adults with body-mass index ≥30 kg m⁻² who initiated FDA-approved weight-loss GLP-1 RAs (liraglutide, semaglutide, or tirzepatide) or underwent sleeve gastrectomy (SG) or Roux-en-Y gastric bypass (RYGB) from 2015–2020. Patients with prior GLP-1 RA exposure, previous BS, or any history of GERD, esophagitis, BE, esophageal cancer, scleroderma, pregnancy, or intensive-care admission were excluded. Propensity-score matching balanced 47 demographic, clinical, medication, and laboratory variables. Primary outcomes were de novo reflux esophagitis and GERD 5 years after the index event. Secondary outcomes were de novo BE, esophageal cancer, esophagogastroduodenoscopy (EGD) utilization, and new proton-pump inhibitor (PPI) or H₂-blocker prescriptions.
Results: Before matching, 89422 BS recipients (mean age 48.98±13.54 yr; 72.5% female) and 84689 GLP-1 RA users (52.99±12.84 yr; 56.2% female) were identified. Post-matching cohorts were well balanced (mean age 51.3±13.3 yr; 65.4% female each). At five years, BS conferred higher rates of reflux esophagitis (0.72% vs 0.36%; aOR 1.99, 1.63–2.42), GERD (16.92% vs 9.79%; aOR 1.88, 1.80–1.96), and BE (0.46% vs 0.23%; aOR 2.02, 1.57–2.59); esophageal cancer remained rare (0.03% each; aOR 1.18, 0.53–2.64). BS patients more frequently underwent EGD (8.82% vs 3.69%; aOR 2.53, 2.38–2.69), initiated PPIs (29.39% vs 20.83%; aOR 1.58, 1.53–1.63), and required H₂-blockers (15.57% vs 11.00%; aOR 1.49, 1.43–1.56). Subgroup analyses showed the lowest GERD incidence with tirzepatide (6.36%) and the highest with SG (19.14%) relative to GLP-1 RAs.
Discussion: In this large, real-world matched cohort, bariatric surgery—particularly sleeve gastrectomy—nearly doubled the five-year risk of de novo GERD, esophagitis, and BE compared with GLP-1 RA therapy, translating into greater endoscopic and pharmacologic reflux management. Clinicians should weigh durable weight-loss benefits against divergent esophageal risks when counseling patients, and future longitudinal work is warranted to clarify the comparative incidence of esophageal adenocarcinoma.
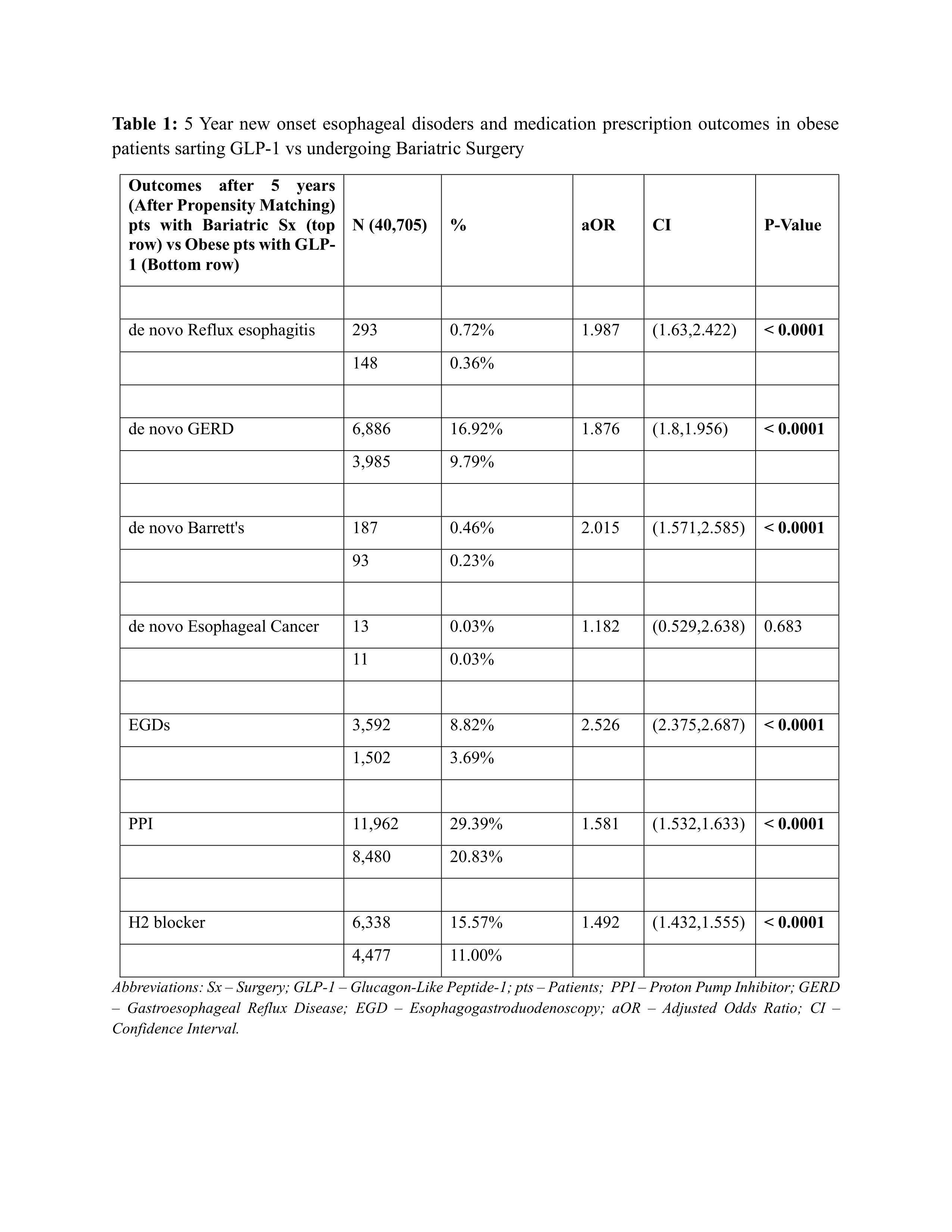
Figure: Table 1: 5 Year new onset esophageal disoders and medication prescription outcomes in obese patients sarting GLP-1 vs undergoing Bariatric Surgery
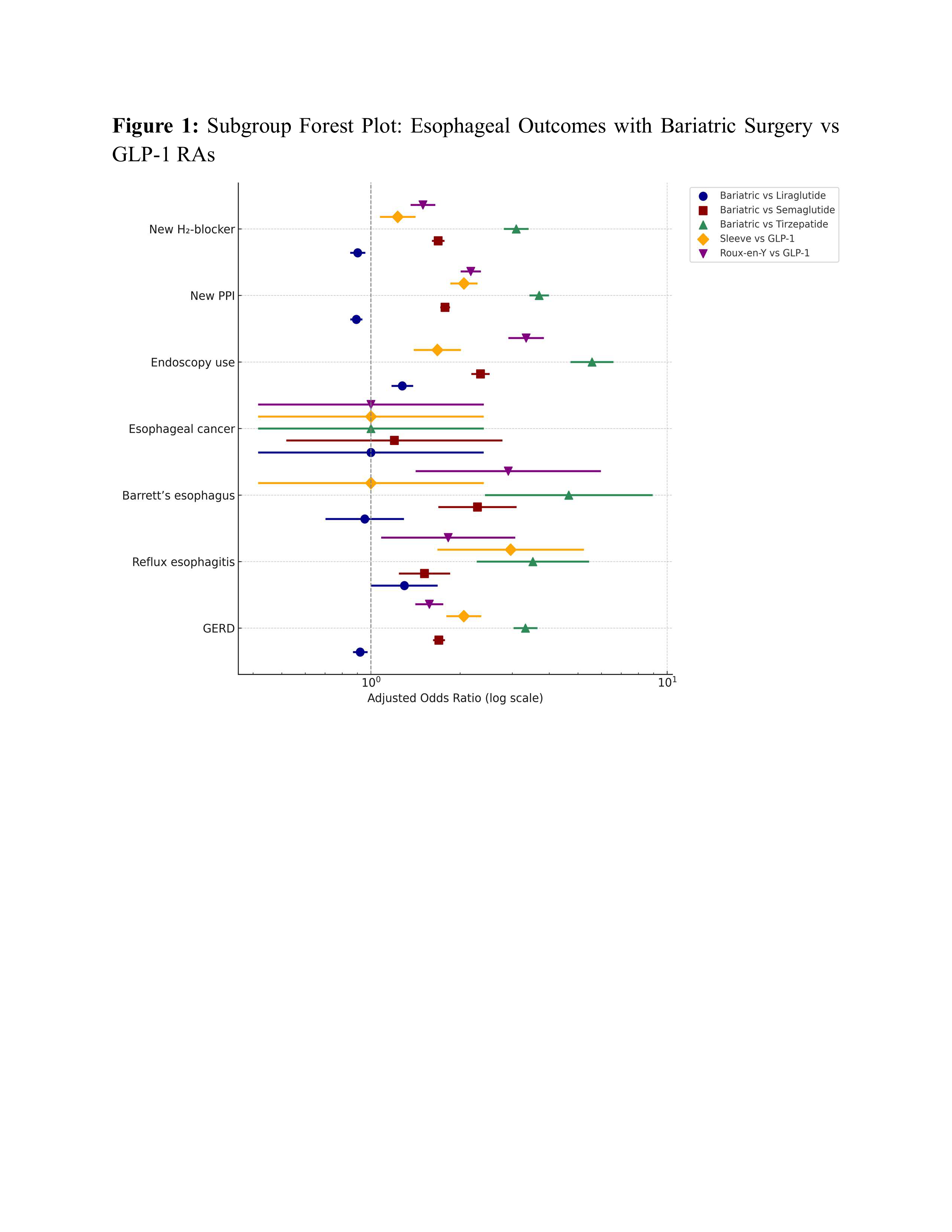
Figure: Figure 1: Subgroup Forest Plot: Esophageal Outcomes with Bariatric Surgery vs GLP-1 RAs
Disclosures:
Himsikhar Khataniar indicated no relevant financial relationships.
Sameer Rao indicated no relevant financial relationships.
Hany Habib indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Shifa Umar indicated no relevant financial relationships.
Himsikhar Khataniar, MD1, Sameer Rao, MBBS2, Hany Habib, MD3, Rahul Karna, MD4, Shifa Umar, MD5. P0609 - Bariatric Surgery Nearly Doubles 5-Year Reflux and Barrett’s Risk versus GLP-1 Agonists: A Propensity-Matched, 81 410-Patient Cohort Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Allegheny General Hospital, Pittsburgh, PA; 2Rutgers New Jersey Medical School, Newark, NJ; 3Allegheny Health Network Medicine Institute, Pittsburgh, PA; 4University of Minnesota Medical Center, Minneapolis, MN; 5Baylor College of Medicine, Houston, TX
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) have emerged as a pharmacologic alternative to bariatric surgery (BS) for weight reduction after U.S. Food and Drug Administration approval for obesity. Delayed gastric emptying with GLP-1 RAs and anatomic disruption after BS may each predispose to new onset esophageal disorders.
Methods: Using the TriNetX U.S. Collaborative Network, we identified adults with body-mass index ≥30 kg m⁻² who initiated FDA-approved weight-loss GLP-1 RAs (liraglutide, semaglutide, or tirzepatide) or underwent sleeve gastrectomy (SG) or Roux-en-Y gastric bypass (RYGB) from 2015–2020. Patients with prior GLP-1 RA exposure, previous BS, or any history of GERD, esophagitis, BE, esophageal cancer, scleroderma, pregnancy, or intensive-care admission were excluded. Propensity-score matching balanced 47 demographic, clinical, medication, and laboratory variables. Primary outcomes were de novo reflux esophagitis and GERD 5 years after the index event. Secondary outcomes were de novo BE, esophageal cancer, esophagogastroduodenoscopy (EGD) utilization, and new proton-pump inhibitor (PPI) or H₂-blocker prescriptions.
Results: Before matching, 89422 BS recipients (mean age 48.98±13.54 yr; 72.5% female) and 84689 GLP-1 RA users (52.99±12.84 yr; 56.2% female) were identified. Post-matching cohorts were well balanced (mean age 51.3±13.3 yr; 65.4% female each). At five years, BS conferred higher rates of reflux esophagitis (0.72% vs 0.36%; aOR 1.99, 1.63–2.42), GERD (16.92% vs 9.79%; aOR 1.88, 1.80–1.96), and BE (0.46% vs 0.23%; aOR 2.02, 1.57–2.59); esophageal cancer remained rare (0.03% each; aOR 1.18, 0.53–2.64). BS patients more frequently underwent EGD (8.82% vs 3.69%; aOR 2.53, 2.38–2.69), initiated PPIs (29.39% vs 20.83%; aOR 1.58, 1.53–1.63), and required H₂-blockers (15.57% vs 11.00%; aOR 1.49, 1.43–1.56). Subgroup analyses showed the lowest GERD incidence with tirzepatide (6.36%) and the highest with SG (19.14%) relative to GLP-1 RAs.
Discussion: In this large, real-world matched cohort, bariatric surgery—particularly sleeve gastrectomy—nearly doubled the five-year risk of de novo GERD, esophagitis, and BE compared with GLP-1 RA therapy, translating into greater endoscopic and pharmacologic reflux management. Clinicians should weigh durable weight-loss benefits against divergent esophageal risks when counseling patients, and future longitudinal work is warranted to clarify the comparative incidence of esophageal adenocarcinoma.
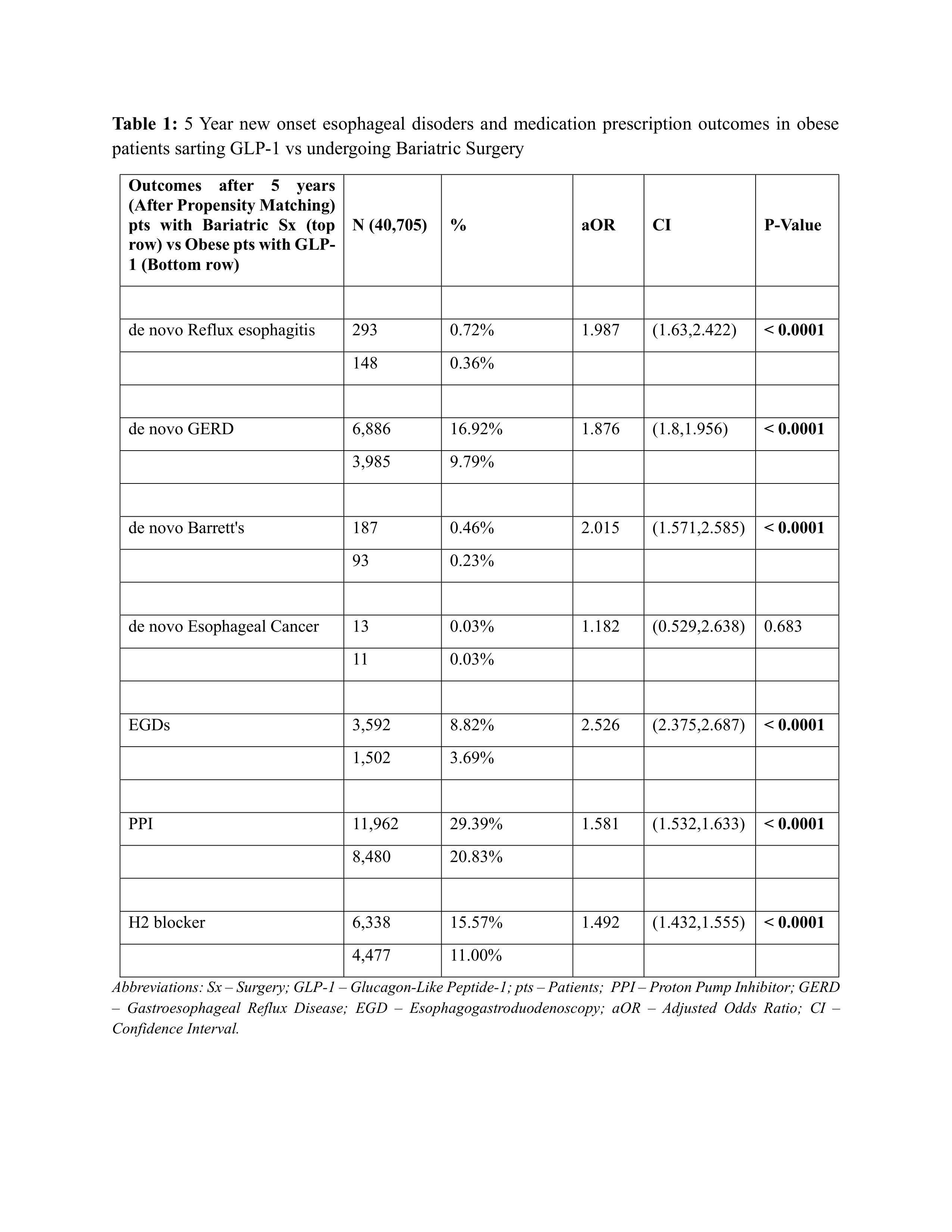
Figure: Table 1: 5 Year new onset esophageal disoders and medication prescription outcomes in obese patients sarting GLP-1 vs undergoing Bariatric Surgery
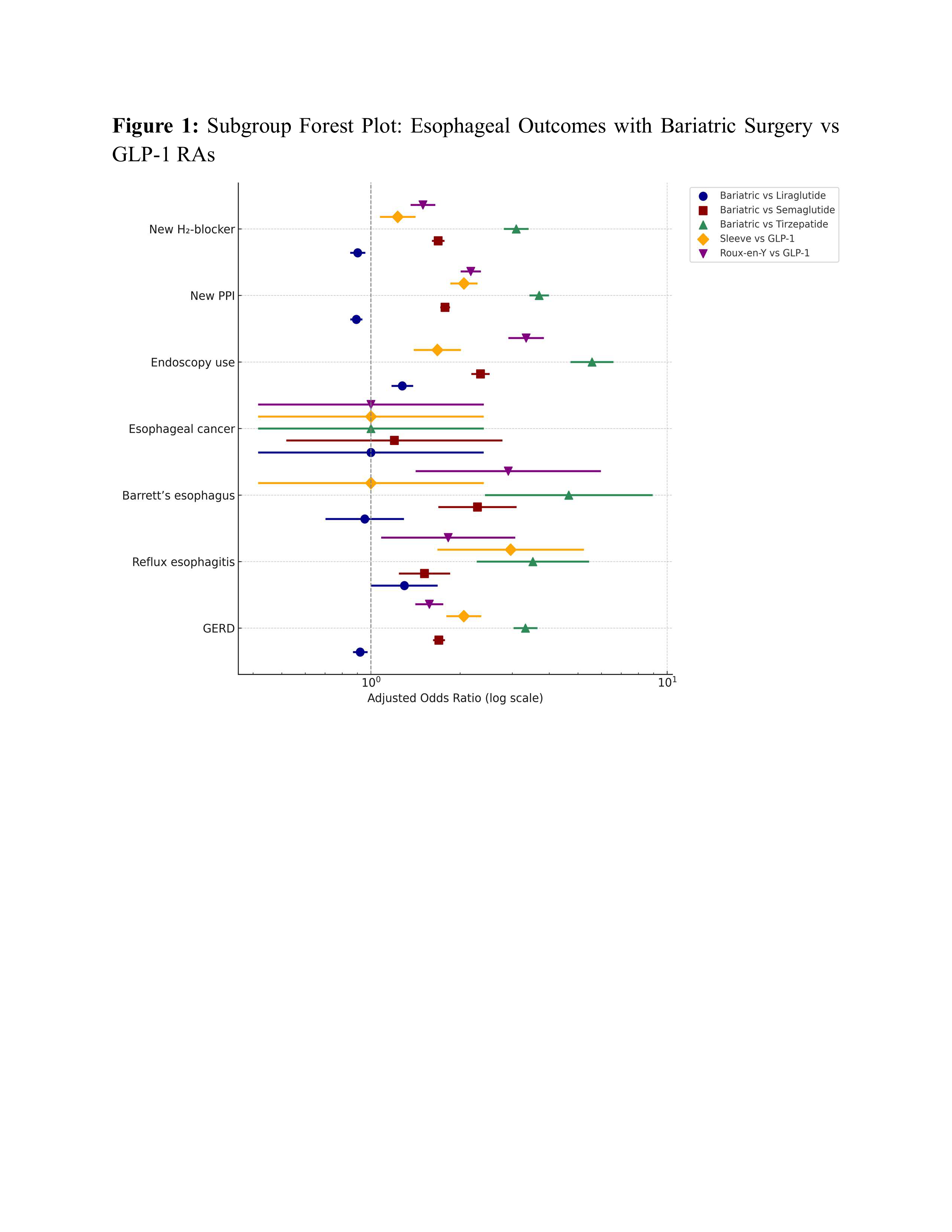
Figure: Figure 1: Subgroup Forest Plot: Esophageal Outcomes with Bariatric Surgery vs GLP-1 RAs
Disclosures:
Himsikhar Khataniar indicated no relevant financial relationships.
Sameer Rao indicated no relevant financial relationships.
Hany Habib indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Shifa Umar indicated no relevant financial relationships.
Himsikhar Khataniar, MD1, Sameer Rao, MBBS2, Hany Habib, MD3, Rahul Karna, MD4, Shifa Umar, MD5. P0609 - Bariatric Surgery Nearly Doubles 5-Year Reflux and Barrett’s Risk versus GLP-1 Agonists: A Propensity-Matched, 81 410-Patient Cohort Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
