Sunday Poster Session
Category: Esophagus
P0606 - Esophageal Lichen Planus: Hard to Swallow, Harder to Diagnose
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Makell S. Brown, BSPH (he/him/his)
Atrium Health Wake Forest Baptist
Winston-Salem, NC
Presenting Author(s)
Makell S. Brown, BSPH1, Robert M. Treadway, BS1, Isaiah J. Miller, BS1, Joseph Jorrizo, MD1, Steven B. Clayton, MD2
1Atrium Health Wake Forest Baptist, Winston-Salem, NC; 2Wake Forest University School of Medicine, Winston-Salem, NC
Introduction: Esophageal lichen planus (ELP) is a rare form of mucocutaneous lichen planus commonly seen in middle-aged women. Patients often present with dysphagia and odynophagia, due to the formation of esophageal lesions and strictures. Relative to other mucosal manifestations of lichen planus, ELP is less frequently reported and has no well-established prevalence. A general lack of knowledge of ELP impedes efficient treatment and diagnosis, resulting in increased time to diagnosis and misdiagnoses of gastrointestinal esophageal reflux disease (GERD), eosinophilic esophagitis, and more. To alleviate disease burden, mitigate misdiagnoses, and improve time to diagnosis, characterization and analysis of patients diagnosed with ELP is essential. This study aims to review 15 patients diagnosed with ELP to increase understanding and identify features that impede diagnosis.
Methods: This was a retrospective cohort study. Patients aged >18 with a diagnosis of ELP were included. Diagnoses were confirmed through chart review of EGD findings and pathology reports at our institution. Demographic data, treatment details, and histopathologic findings were also collected. Severity was assessed using the ELP Severity Score, developed by Keshav et al.
Results: 15 cases of esophageal lichen planus were reviewed (see Table 1 for demographic data). The median number of biopsies before diagnosis of ELP was 3, with a median time to diagnosis of 41 months. All patients were dilated during EGD, with 80% of patients found to have luminal stenosis (median ELP severity: 5). 60% of patients were treated with immunosuppressants (mycophenolate, methotrexate, tacrolimus, azathioprine), 40% were treated with a topical steroid (budesonide, triamcinolone injection), and 13% were treated with an anti-inflammatory (metronidazole). At the time of diagnosis, 47% of our patient cohort had thyroid disease. Following treatment, 67% reported symptomatic improvement with 47% also having luminal diameter improvement.
Discussion: In conclusion, ELP is a debilitating condition that is difficult to diagnose, requiring a median of 3 EGDs with biopsy. In a middle-aged female with dysphagia and diffuse esophageal narrowing, ELP should always be considered, despite a likely initial failure to make a histologic diagnosis. Therapy should be aimed at decreasing inflammation and dilating to restore esophageal luminal diameter, as this improved symptoms in most of our patient cohort. Future studies are needed to ameliorate histologic analysis.
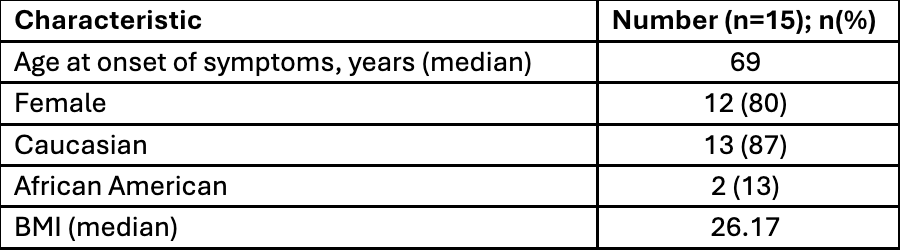
Figure: Table 1: Patient Demographics
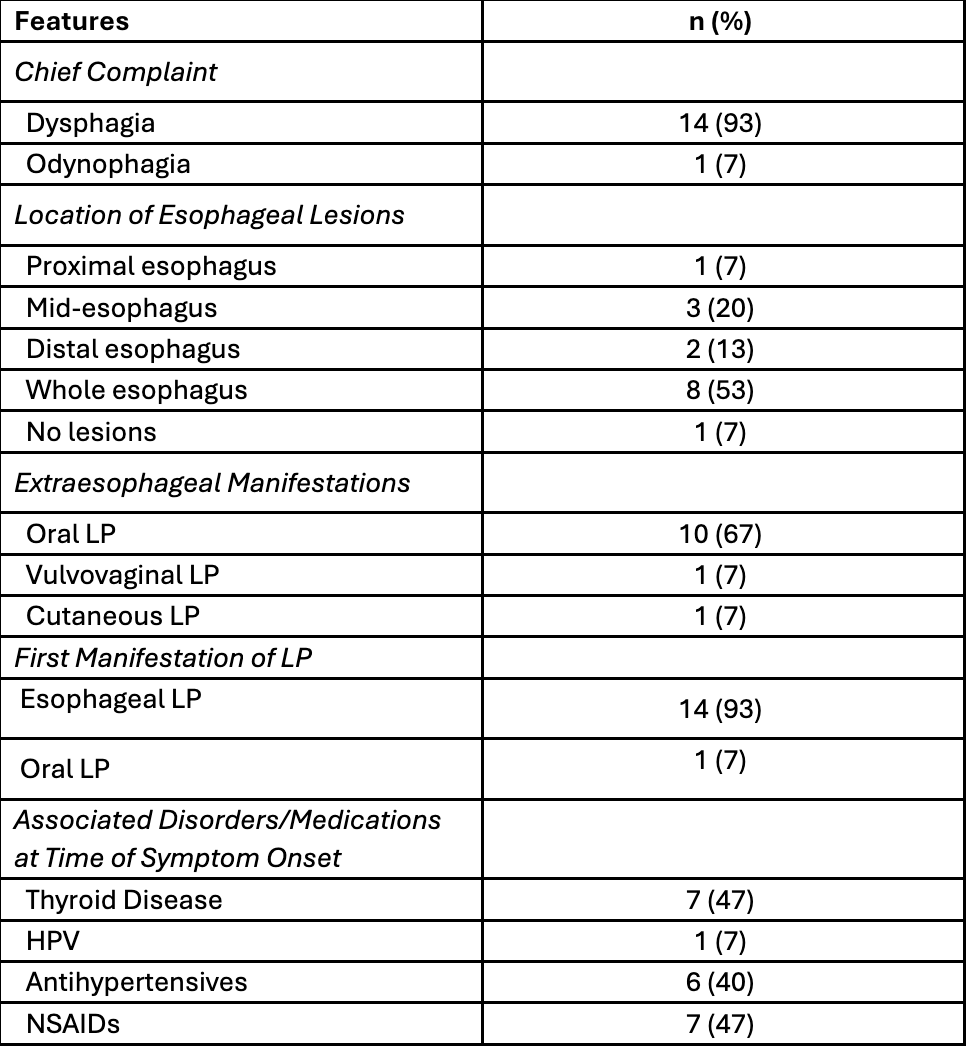
Figure: Table 2: Features of Esophageal Lichen Planus
Disclosures:
Makell Brown indicated no relevant financial relationships.
Robert Treadway indicated no relevant financial relationships.
Isaiah Miller indicated no relevant financial relationships.
Joseph Jorrizo indicated no relevant financial relationships.
Steven Clayton indicated no relevant financial relationships.
Makell S. Brown, BSPH1, Robert M. Treadway, BS1, Isaiah J. Miller, BS1, Joseph Jorrizo, MD1, Steven B. Clayton, MD2. P0606 - Esophageal Lichen Planus: Hard to Swallow, Harder to Diagnose, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Atrium Health Wake Forest Baptist, Winston-Salem, NC; 2Wake Forest University School of Medicine, Winston-Salem, NC
Introduction: Esophageal lichen planus (ELP) is a rare form of mucocutaneous lichen planus commonly seen in middle-aged women. Patients often present with dysphagia and odynophagia, due to the formation of esophageal lesions and strictures. Relative to other mucosal manifestations of lichen planus, ELP is less frequently reported and has no well-established prevalence. A general lack of knowledge of ELP impedes efficient treatment and diagnosis, resulting in increased time to diagnosis and misdiagnoses of gastrointestinal esophageal reflux disease (GERD), eosinophilic esophagitis, and more. To alleviate disease burden, mitigate misdiagnoses, and improve time to diagnosis, characterization and analysis of patients diagnosed with ELP is essential. This study aims to review 15 patients diagnosed with ELP to increase understanding and identify features that impede diagnosis.
Methods: This was a retrospective cohort study. Patients aged >18 with a diagnosis of ELP were included. Diagnoses were confirmed through chart review of EGD findings and pathology reports at our institution. Demographic data, treatment details, and histopathologic findings were also collected. Severity was assessed using the ELP Severity Score, developed by Keshav et al.
Results: 15 cases of esophageal lichen planus were reviewed (see Table 1 for demographic data). The median number of biopsies before diagnosis of ELP was 3, with a median time to diagnosis of 41 months. All patients were dilated during EGD, with 80% of patients found to have luminal stenosis (median ELP severity: 5). 60% of patients were treated with immunosuppressants (mycophenolate, methotrexate, tacrolimus, azathioprine), 40% were treated with a topical steroid (budesonide, triamcinolone injection), and 13% were treated with an anti-inflammatory (metronidazole). At the time of diagnosis, 47% of our patient cohort had thyroid disease. Following treatment, 67% reported symptomatic improvement with 47% also having luminal diameter improvement.
Discussion: In conclusion, ELP is a debilitating condition that is difficult to diagnose, requiring a median of 3 EGDs with biopsy. In a middle-aged female with dysphagia and diffuse esophageal narrowing, ELP should always be considered, despite a likely initial failure to make a histologic diagnosis. Therapy should be aimed at decreasing inflammation and dilating to restore esophageal luminal diameter, as this improved symptoms in most of our patient cohort. Future studies are needed to ameliorate histologic analysis.
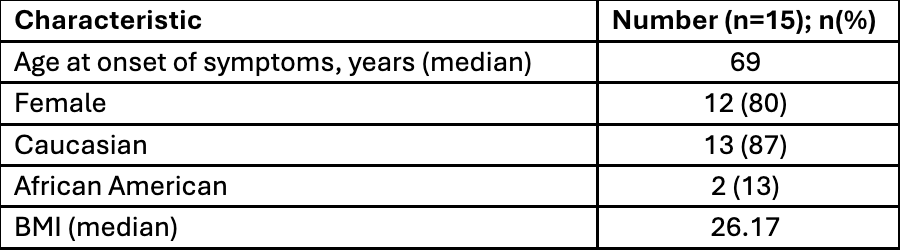
Figure: Table 1: Patient Demographics
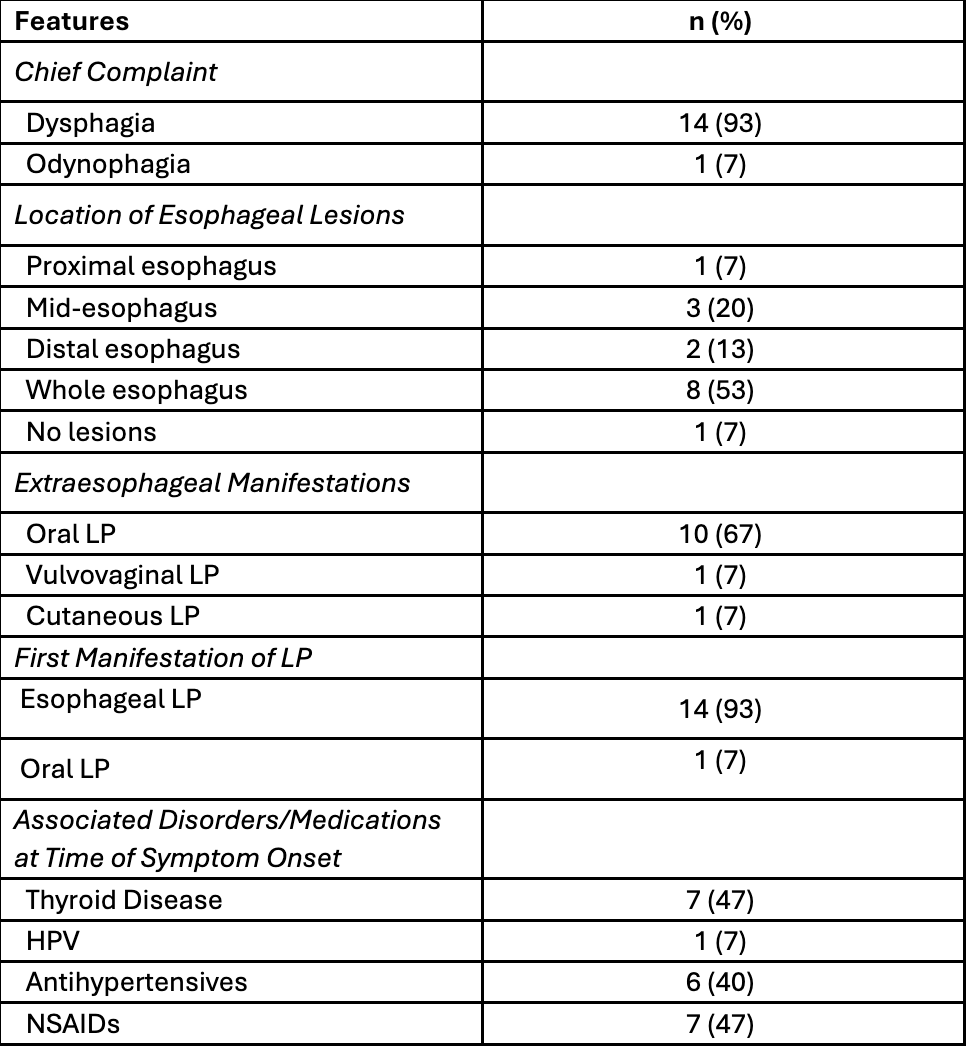
Figure: Table 2: Features of Esophageal Lichen Planus
Disclosures:
Makell Brown indicated no relevant financial relationships.
Robert Treadway indicated no relevant financial relationships.
Isaiah Miller indicated no relevant financial relationships.
Joseph Jorrizo indicated no relevant financial relationships.
Steven Clayton indicated no relevant financial relationships.
Makell S. Brown, BSPH1, Robert M. Treadway, BS1, Isaiah J. Miller, BS1, Joseph Jorrizo, MD1, Steven B. Clayton, MD2. P0606 - Esophageal Lichen Planus: Hard to Swallow, Harder to Diagnose, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
