Sunday Poster Session
Category: Esophagus
P0698 - Aggressive Gastric and Duodenal Metastasis of Esophageal Adenocarcinoma Associated With Esophageal Stent Migration
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Ali A. Mashadi, MD (he/him/his)
AdventHealth
Wellington, FL
Presenting Author(s)
Ali Mashadi, MD1, Mahmoud Abdallah, MD2, Michael D. Harris, MD2
1AdventHealth, Wellington, FL; 2AdventHealth, Tampa, FL
Introduction: Esophageal adenocarcinoma often necessitates stent placement for dysphagia due to luminal narrowing. While stent migration typically suggests tumor regression, rare cases suggest potential tumor seeding and metastasis. We report a case of rapid gastric and duodenal metastasis following esophageal adenocarcinoma treatment, possibly linked to stent migration.
Case Description/
Methods: A 55-year-old male with GERD presented with severe dysphagia and odynophagia. EGD revealed an 8 cm esophageal mass, confirmed as moderately to poorly differentiated adenocarcinoma on Barrett’s esophagus. Stomach and duodenal biopsies were initially negative. He underwent palliative stent placement and chemoradiation. Follow-up PET-CT showed marked tumor regression, likely allowing stent dislodgement into the stomach, which was retrieved endoscopically without complication.
Weeks later, the patient returned with acute-onset, intractable projectile vomiting and severe nausea. Suspecting gastric outlet obstruction, CT showed new thickening of the gastric antrum and duodenum with fat stranding, submucosal edema, and a possible antral ulceration. These findings raised concern for an infiltrative process. EGD revealed mild esophageal exudate and subepithelial hemorrhoids (post-treatment), with edematous, erythematous gastric and duodenal mucosa suggestive of a subepithelial or extramural lesion. Biopsies confirmed poorly differentiated adenocarcinoma matching the esophageal primary, despite previously negative findings, confirming malignant gastric outlet obstruction.
Endoscopic treatment involved overlapping uncovered stents, followed by a fully covered stent for obstruction. Despite this, symptoms persisted. Rapid spread to previously unaffected areas raised concern for tumor seeding from prior stent migration. The patient ultimately opted for palliative care.
Discussion: This case highlights an unusually rapid and extensive metastatic progression of esophageal adenocarcinoma despite initial remission, potentially linked to stent migration. While often benign, esophageal stent migration may theoretically allow tumor cell implantation, enabling aggressive downstream metastases. Literature notes rare cases of mechanical tumor seeding from migrated stents, particularly with mucosal injury or perforation. Clinicians should suspect recurrence or metastasis in previously treated esophageal cancer patients presenting with new GI obstructive symptoms, even when recent imaging appears benign.
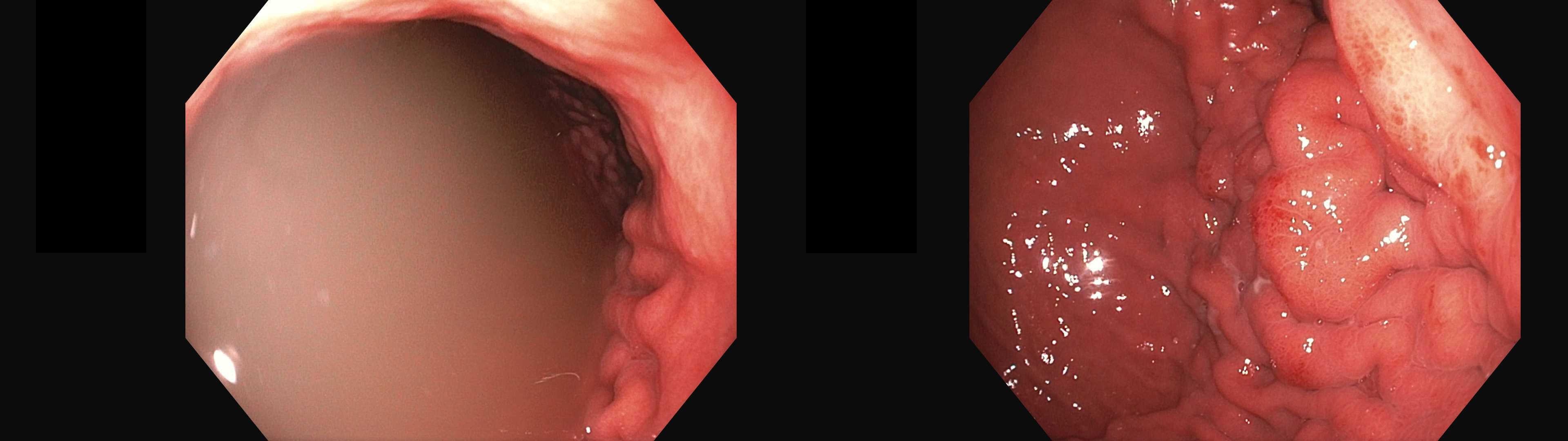
Figure: Axial contrast-enhanced CT images demonstrate prominent wall thickening of the gastric antrum and duodenum (right image), with surrounding fat stranding and submucosal edema. The left image highlights more prominent antral thickening.
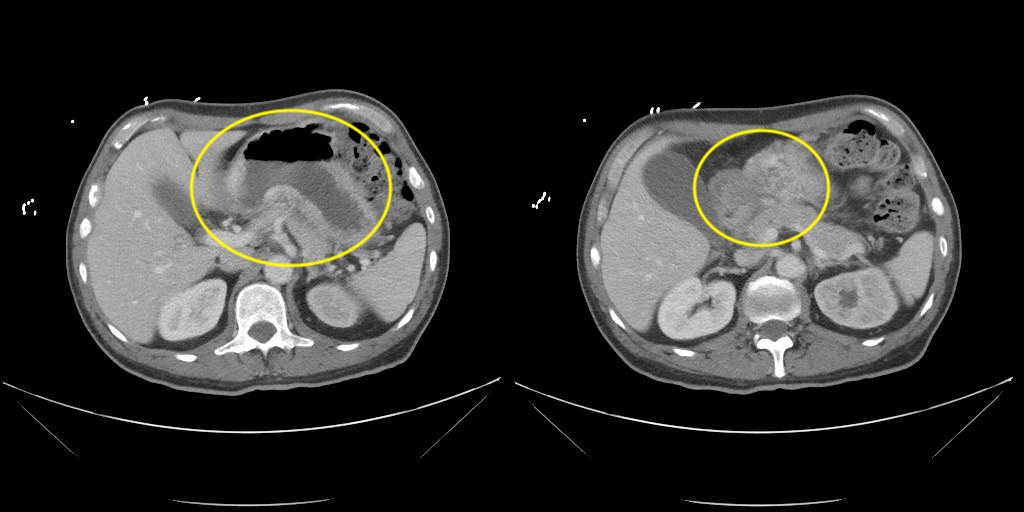
Figure: Endoscopic images showing the gastric antrum and proximal duodenum. The mucosa appears edematous and erythematous with areas of distortion and thickened folds, concerning for subepithelial or infiltrative pathology.
Disclosures:
Ali Mashadi indicated no relevant financial relationships.
Mahmoud Abdallah indicated no relevant financial relationships.
Michael Harris indicated no relevant financial relationships.
Ali Mashadi, MD1, Mahmoud Abdallah, MD2, Michael D. Harris, MD2. P0698 - Aggressive Gastric and Duodenal Metastasis of Esophageal Adenocarcinoma Associated With Esophageal Stent Migration, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1AdventHealth, Wellington, FL; 2AdventHealth, Tampa, FL
Introduction: Esophageal adenocarcinoma often necessitates stent placement for dysphagia due to luminal narrowing. While stent migration typically suggests tumor regression, rare cases suggest potential tumor seeding and metastasis. We report a case of rapid gastric and duodenal metastasis following esophageal adenocarcinoma treatment, possibly linked to stent migration.
Case Description/
Methods: A 55-year-old male with GERD presented with severe dysphagia and odynophagia. EGD revealed an 8 cm esophageal mass, confirmed as moderately to poorly differentiated adenocarcinoma on Barrett’s esophagus. Stomach and duodenal biopsies were initially negative. He underwent palliative stent placement and chemoradiation. Follow-up PET-CT showed marked tumor regression, likely allowing stent dislodgement into the stomach, which was retrieved endoscopically without complication.
Weeks later, the patient returned with acute-onset, intractable projectile vomiting and severe nausea. Suspecting gastric outlet obstruction, CT showed new thickening of the gastric antrum and duodenum with fat stranding, submucosal edema, and a possible antral ulceration. These findings raised concern for an infiltrative process. EGD revealed mild esophageal exudate and subepithelial hemorrhoids (post-treatment), with edematous, erythematous gastric and duodenal mucosa suggestive of a subepithelial or extramural lesion. Biopsies confirmed poorly differentiated adenocarcinoma matching the esophageal primary, despite previously negative findings, confirming malignant gastric outlet obstruction.
Endoscopic treatment involved overlapping uncovered stents, followed by a fully covered stent for obstruction. Despite this, symptoms persisted. Rapid spread to previously unaffected areas raised concern for tumor seeding from prior stent migration. The patient ultimately opted for palliative care.
Discussion: This case highlights an unusually rapid and extensive metastatic progression of esophageal adenocarcinoma despite initial remission, potentially linked to stent migration. While often benign, esophageal stent migration may theoretically allow tumor cell implantation, enabling aggressive downstream metastases. Literature notes rare cases of mechanical tumor seeding from migrated stents, particularly with mucosal injury or perforation. Clinicians should suspect recurrence or metastasis in previously treated esophageal cancer patients presenting with new GI obstructive symptoms, even when recent imaging appears benign.
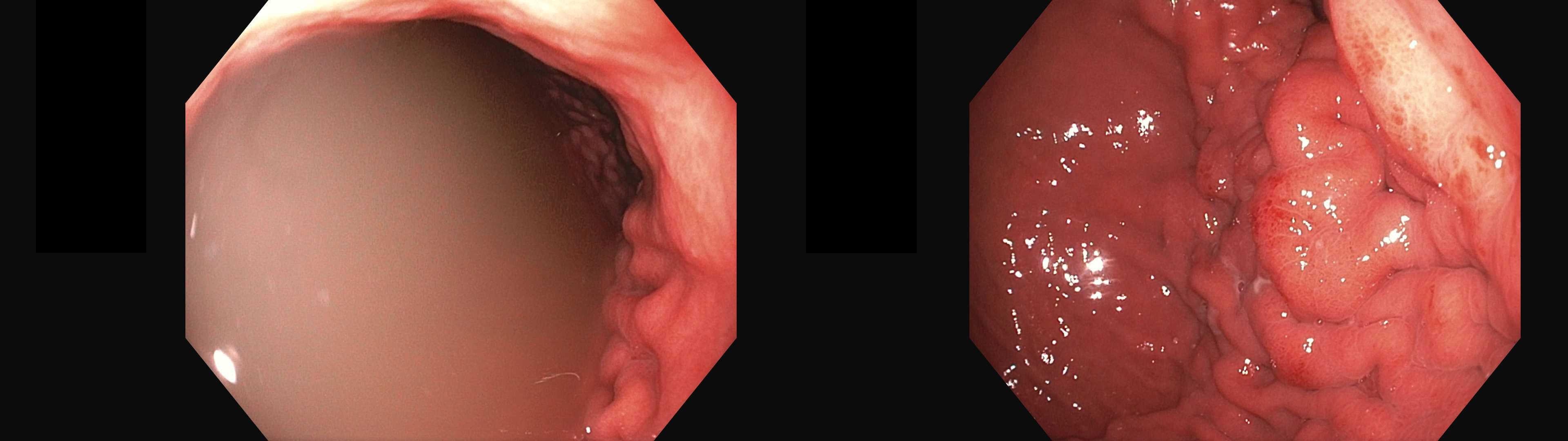
Figure: Axial contrast-enhanced CT images demonstrate prominent wall thickening of the gastric antrum and duodenum (right image), with surrounding fat stranding and submucosal edema. The left image highlights more prominent antral thickening.
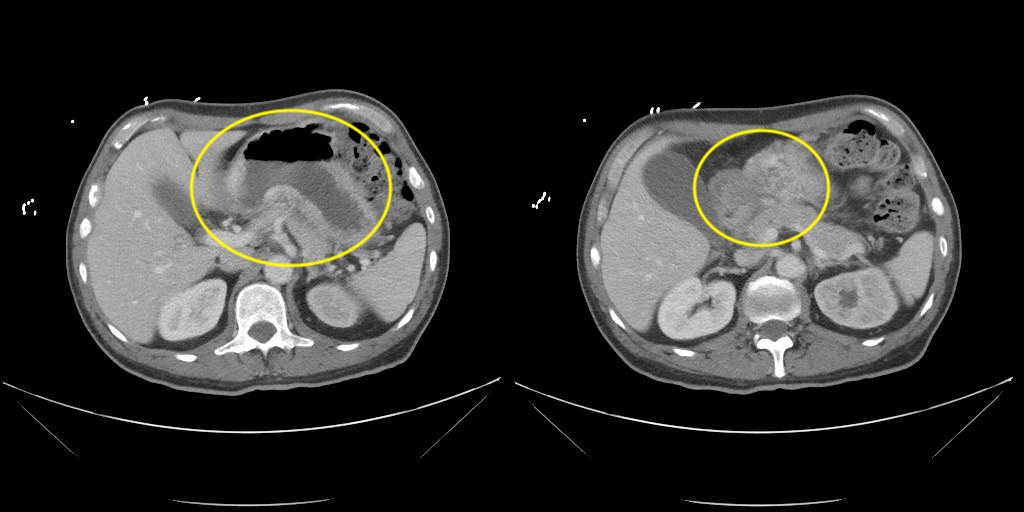
Figure: Endoscopic images showing the gastric antrum and proximal duodenum. The mucosa appears edematous and erythematous with areas of distortion and thickened folds, concerning for subepithelial or infiltrative pathology.
Disclosures:
Ali Mashadi indicated no relevant financial relationships.
Mahmoud Abdallah indicated no relevant financial relationships.
Michael Harris indicated no relevant financial relationships.
Ali Mashadi, MD1, Mahmoud Abdallah, MD2, Michael D. Harris, MD2. P0698 - Aggressive Gastric and Duodenal Metastasis of Esophageal Adenocarcinoma Associated With Esophageal Stent Migration, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
