Sunday Poster Session
Category: Esophagus
P0696 - Acute Onset of Achalasia in a Patient With Metoprolol Initiation
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- MS
Michelle Shi, MD
Northwell Health
Manhasset, NY
Presenting Author(s)
Michelle Shi, MD, Mary Cheung, MD
Northwell Health, Manhasset, NY
Introduction: Beta-blocker (BB) was shown to elevate the lower esophageal sphincter (LES) pressure in healthy volunteers, but the effect of BB on esophagogastric junction outflow obstruction (EGJOO) is insufficient. We described a case of acute dysphagia in a patient with new BB therapy.
Case Description/
Methods: A 72-year-old female developed new dysphagia to solids/liquids one day post percutaneous coronary intervention (PCI) for myocardial infarction, necessitating nasogastric tube feeding. An esophagram showed distal esophageal obstruction. Esophagogastroduodenoscopy (EGD) revealed dilation of the proximal esophagus without other structural abnormalities. The patient was transferred to our center on hospital day 16 for further motility workup.
Upon transfer, the patient had stable hemodynamics with unremarkable physical exam and laboratory workup. A repeat esophagram showed proximal esophageal dilation with disordered peristalsis, and the 13-mm barium tablet remained near the gastroesophageal junction 10 minutes after swallowing (Figure 1). It was discovered that metoprolol tartrate was initiated after the PCI. The patient was switched to carvedilol, which she previously tolerated without symptoms. The last dose of metoprolol was on day 17. High resolution manometry on day 18 (Figure 2) showed high LES integrated relaxation pressure (48.2 mmHg), with 60% of supine and 100% of upright swallows demonstrated spastic contractions with a shortened distal latency (< 4.5 seconds). Incomplete bolus clearance was demonstrated in 100% of the supine swallows. The patient had no esophageal muscle reserve and had incomplete relaxation of LES on the rapid bolus challenge. The patient was diagnosed with type III achalasia based on the Chicago Classification 4.0 scheme. Peroral endoscopic myotomy was deferred for the need of uninterrupted dual antiplatelet therapy and a repeat EGD with botulinum toxin treatment was initially planned.
Fortunately, the patient tolerated clear liquids on day 21 and a regular diet on day 22. She was discharged on day 23 without endoscopic interventions. The patient did not report further episodes of dysphagia while on carvedilol during her 2-month outpatient follow up. The patient declined repeat manometry.
Discussion: This case described a patient with acute onset of type III achalasia after initiation of metoprolol tartrate, with complete resolution after switching to carvedilol. Further studies are warranted to explore the effects of different BB formulations on EGJOO.
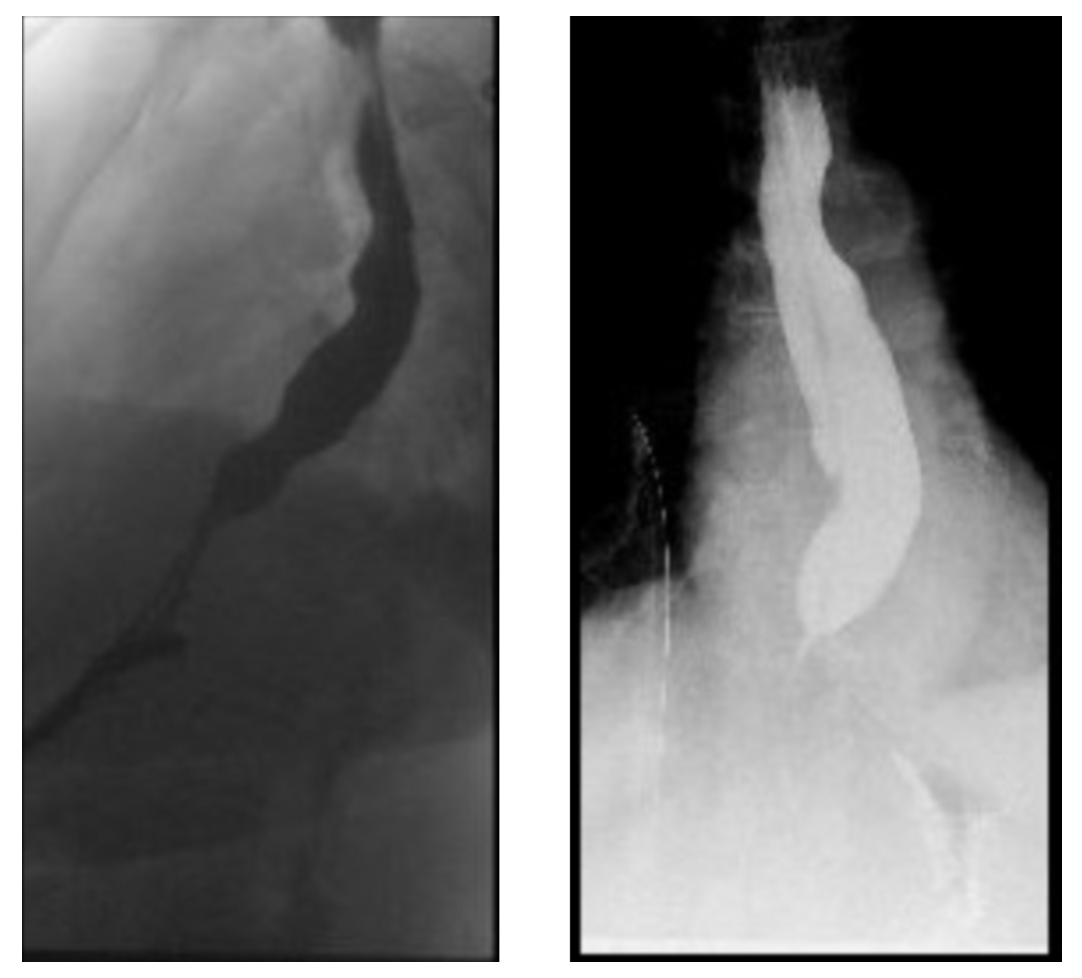
Figure: Figure 1 – Repeat Barium Esophagram on day 17 with dilated esophagus and disorganized peristalsis.
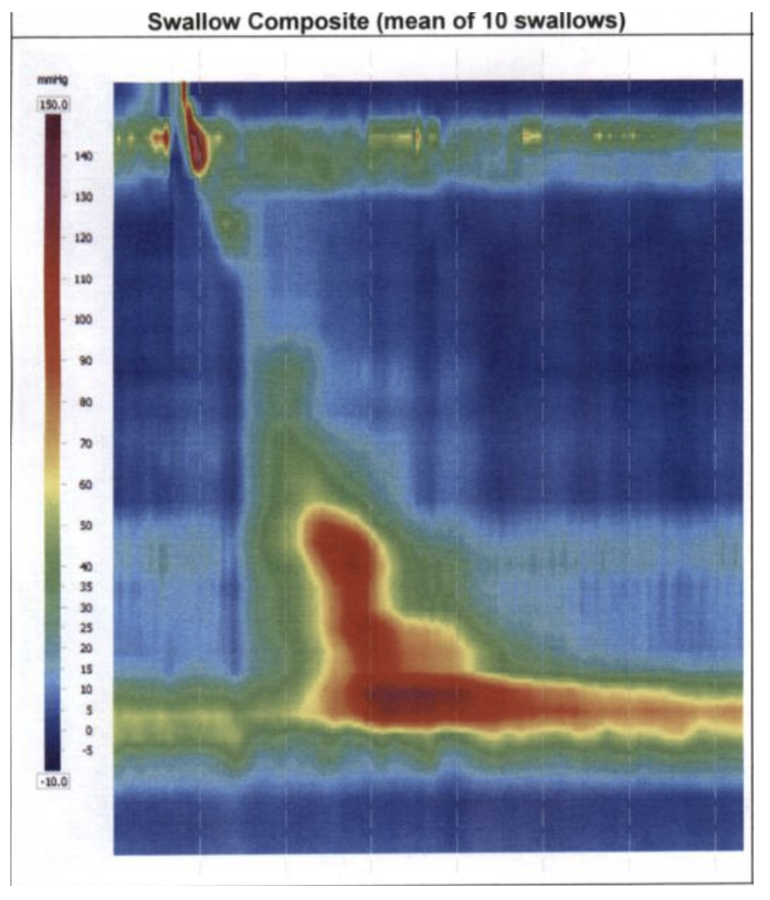
Figure: Figure 2 - High Resolution Manometry Performed on Day 18 Showed Elevated LES Integrated Relaxation Pressure and Shortened Distal Latency.
Disclosures:
Michelle Shi indicated no relevant financial relationships.
Mary Cheung indicated no relevant financial relationships.
Michelle Shi, MD, Mary Cheung, MD. P0696 - Acute Onset of Achalasia in a Patient With Metoprolol Initiation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Northwell Health, Manhasset, NY
Introduction: Beta-blocker (BB) was shown to elevate the lower esophageal sphincter (LES) pressure in healthy volunteers, but the effect of BB on esophagogastric junction outflow obstruction (EGJOO) is insufficient. We described a case of acute dysphagia in a patient with new BB therapy.
Case Description/
Methods: A 72-year-old female developed new dysphagia to solids/liquids one day post percutaneous coronary intervention (PCI) for myocardial infarction, necessitating nasogastric tube feeding. An esophagram showed distal esophageal obstruction. Esophagogastroduodenoscopy (EGD) revealed dilation of the proximal esophagus without other structural abnormalities. The patient was transferred to our center on hospital day 16 for further motility workup.
Upon transfer, the patient had stable hemodynamics with unremarkable physical exam and laboratory workup. A repeat esophagram showed proximal esophageal dilation with disordered peristalsis, and the 13-mm barium tablet remained near the gastroesophageal junction 10 minutes after swallowing (Figure 1). It was discovered that metoprolol tartrate was initiated after the PCI. The patient was switched to carvedilol, which she previously tolerated without symptoms. The last dose of metoprolol was on day 17. High resolution manometry on day 18 (Figure 2) showed high LES integrated relaxation pressure (48.2 mmHg), with 60% of supine and 100% of upright swallows demonstrated spastic contractions with a shortened distal latency (< 4.5 seconds). Incomplete bolus clearance was demonstrated in 100% of the supine swallows. The patient had no esophageal muscle reserve and had incomplete relaxation of LES on the rapid bolus challenge. The patient was diagnosed with type III achalasia based on the Chicago Classification 4.0 scheme. Peroral endoscopic myotomy was deferred for the need of uninterrupted dual antiplatelet therapy and a repeat EGD with botulinum toxin treatment was initially planned.
Fortunately, the patient tolerated clear liquids on day 21 and a regular diet on day 22. She was discharged on day 23 without endoscopic interventions. The patient did not report further episodes of dysphagia while on carvedilol during her 2-month outpatient follow up. The patient declined repeat manometry.
Discussion: This case described a patient with acute onset of type III achalasia after initiation of metoprolol tartrate, with complete resolution after switching to carvedilol. Further studies are warranted to explore the effects of different BB formulations on EGJOO.
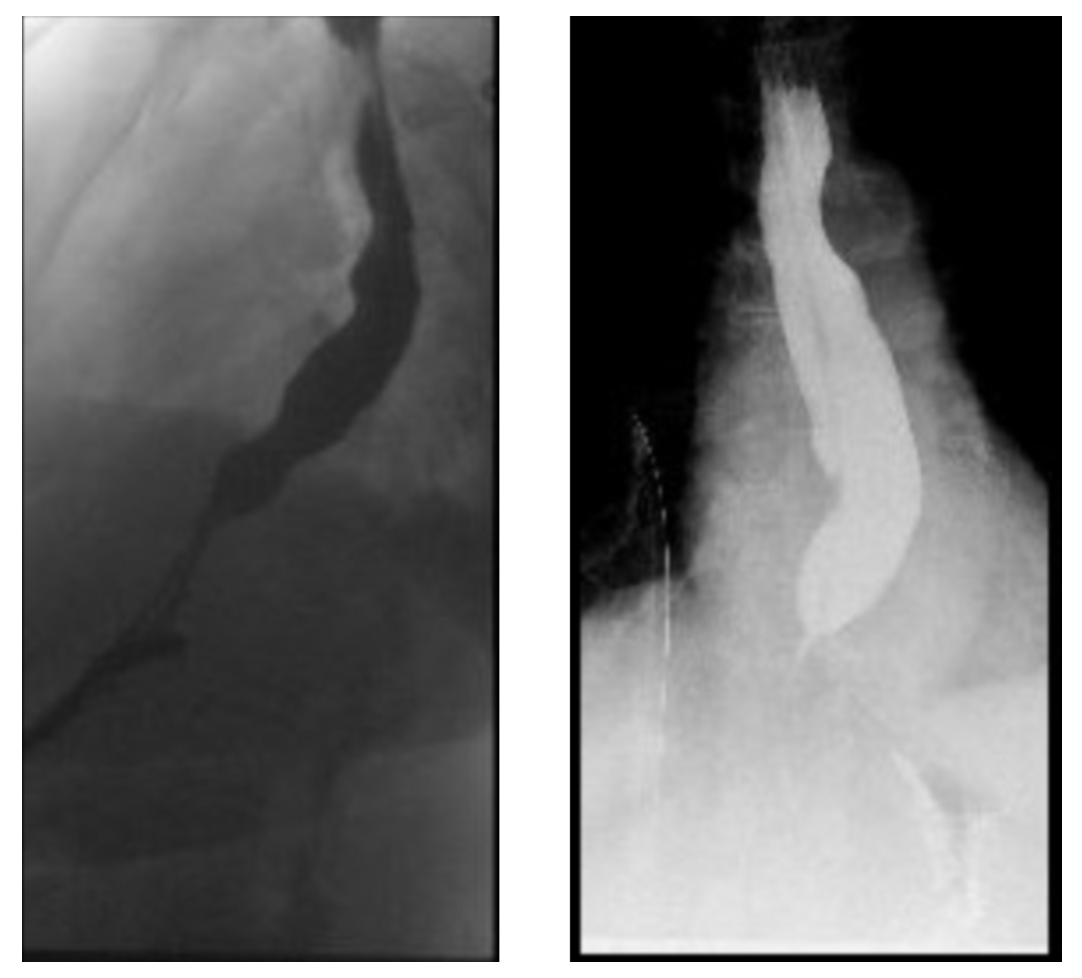
Figure: Figure 1 – Repeat Barium Esophagram on day 17 with dilated esophagus and disorganized peristalsis.
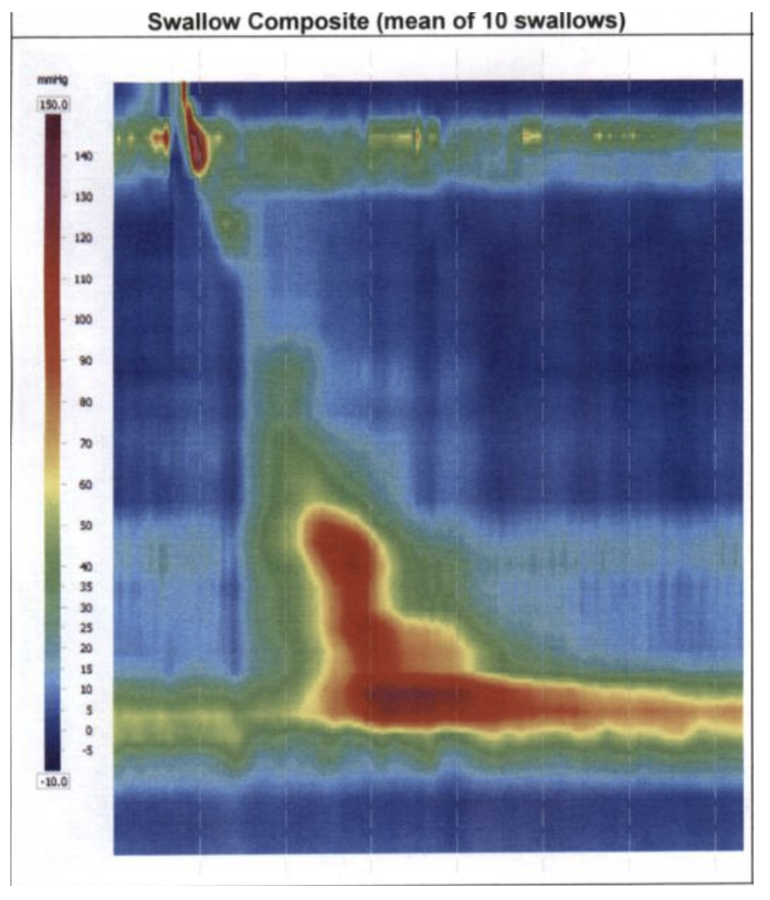
Figure: Figure 2 - High Resolution Manometry Performed on Day 18 Showed Elevated LES Integrated Relaxation Pressure and Shortened Distal Latency.
Disclosures:
Michelle Shi indicated no relevant financial relationships.
Mary Cheung indicated no relevant financial relationships.
Michelle Shi, MD, Mary Cheung, MD. P0696 - Acute Onset of Achalasia in a Patient With Metoprolol Initiation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

