Sunday Poster Session
Category: Esophagus
P0695 - Aortic Compression: Unveiling Dysphagia Aortica in the Elderly
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Hobie L. Hughes, DO (he/him/his)
Thomas Hospital
Fairhope, AL
Presenting Author(s)
Hobie L. Hughes, DO1, Lauren Healey, DO2, Nathaniel Winstead, MD, MSPH, FACG1, Jonathan Francis, MD1, Matthew Eves, MD1
1Thomas Hospital, Fairhope, AL; 2University of South Alabama, Mobile, AL
Introduction: Dysphagia aortica (DA) is a rare form of dysphagia caused by external compression of the esophagus by an enlarged, ectatic, or aneurysmal thoracic aorta. This compression leads to mechanical obstruction resulting in progressively worsening dysphagia. DA is typically seen in elderly patients and has been associated with several risk factors including: female gender, short stature, and kyphosis. The diagnosis of DA can be challenging and often requires a high index of suspicion, especially in patient with a significant cardiovascular history presenting with dysphagia. Typical diagnostic modalities include video-fluoroscopic swallowing studies, computed tomography (CT) scans, and esophageal manometry. Treatment options primarily focus on addressing the underlying aortic pathology causing the external compression with surgical intervention often being necessary.
Case Description/
Methods: An 80-year-old female presented to the emergency department for evaluation of a fall resulting in a left trochanteric femur fracture. Her past medical history was significant for thoracoabdominal aortic aneurysm status post endovascular aneurysm repair (EVAR) with celiac snorkel as well as a superior mesenteric artery stent. Gastroenterology was consulted for evaluation of complaints of dysphagia along with imaging findings which showed concern for esophageal obstruction with an abrupt change in caliber of the thoracic esophagus at the superior most aspect of the aneurysmal sac. An esophagogastroduodenoscopy (EGD) was performed which showed a mildly dilated proximal esophagus with an area of pulsatile, extrinsic compression in the middle and lower third of the esophagus from 25 to 40 cm. There was also a notable area consistent with early esophageal diverticulum noted at 25 to 27 cm.
Discussion: Dysphagia aortica is a rare but significant cause of dysphagia due to esophageal compression by the thoracic aorta. Diagnosis is largely based on imaging findings and clinical suspicion for esophageal obstruction. There are several associated risk factors for developing dysphagia aortica including: advanced age, females, short statute, and significant kyphosis. Treatment options mainly focus on correcting the underlying aortic pathology and often require surgical intervention with either endovascular repair or open surgical repair to relieve the esophageal compression and prevent complications such as aortic rupture.
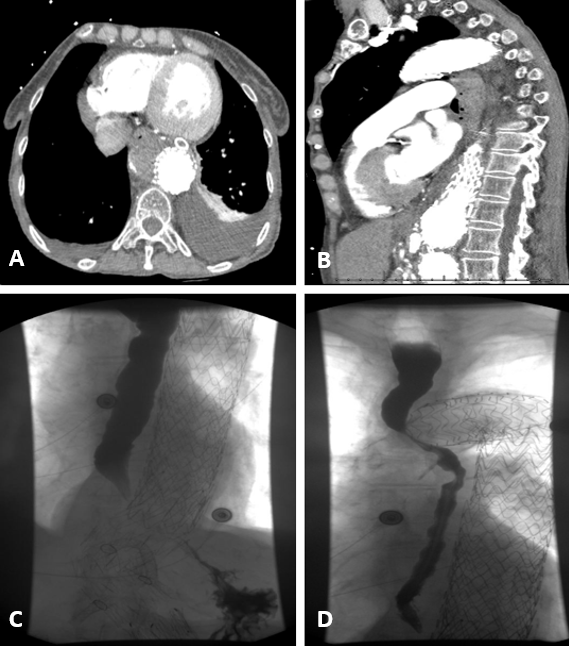
Figure: A: CTA chest transverse view showing extrinsic esophageal compression between thoracoabdominal aneurysm and left atrium and left ventricle.
B: CTA chest sagittal view showing extrinsic esophageal compression between thoracoabdominal aneurysm and left atrium and left ventricle.
C: Upper GI fluoroscopic exam showing lower thoracoabdominal aneurysmal stent with distal esophageal compression and delayed contrast progression.
D: Upper GI fluoroscopic exam showing upper portion of thoracoabdominal aneurysmal stent with proximal esophageal compression and delayed contrast progression.
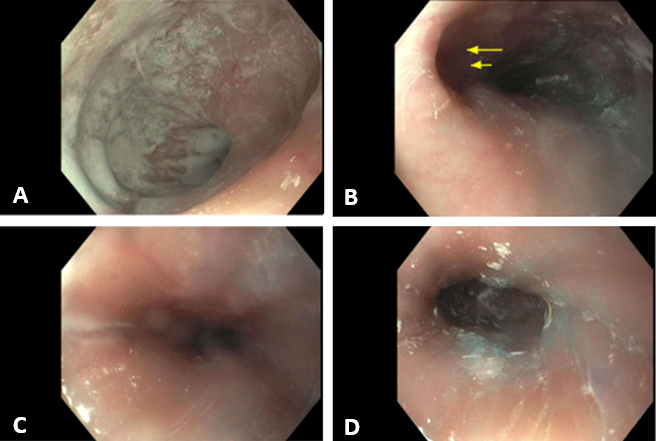
Figure: A: Dilated upper third of esophagus.
B: Middle third of esophagus with early diverticulum (double arrows).
C: Middle third of esophagus with extrinsic compression.
D: Lower third of esophagus with extrinsic compression.
Disclosures:
Hobie Hughes indicated no relevant financial relationships.
Lauren Healey indicated no relevant financial relationships.
Nathaniel Winstead indicated no relevant financial relationships.
Jonathan Francis indicated no relevant financial relationships.
Matthew Eves indicated no relevant financial relationships.
Hobie L. Hughes, DO1, Lauren Healey, DO2, Nathaniel Winstead, MD, MSPH, FACG1, Jonathan Francis, MD1, Matthew Eves, MD1. P0695 - Aortic Compression: Unveiling Dysphagia Aortica in the Elderly, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Thomas Hospital, Fairhope, AL; 2University of South Alabama, Mobile, AL
Introduction: Dysphagia aortica (DA) is a rare form of dysphagia caused by external compression of the esophagus by an enlarged, ectatic, or aneurysmal thoracic aorta. This compression leads to mechanical obstruction resulting in progressively worsening dysphagia. DA is typically seen in elderly patients and has been associated with several risk factors including: female gender, short stature, and kyphosis. The diagnosis of DA can be challenging and often requires a high index of suspicion, especially in patient with a significant cardiovascular history presenting with dysphagia. Typical diagnostic modalities include video-fluoroscopic swallowing studies, computed tomography (CT) scans, and esophageal manometry. Treatment options primarily focus on addressing the underlying aortic pathology causing the external compression with surgical intervention often being necessary.
Case Description/
Methods: An 80-year-old female presented to the emergency department for evaluation of a fall resulting in a left trochanteric femur fracture. Her past medical history was significant for thoracoabdominal aortic aneurysm status post endovascular aneurysm repair (EVAR) with celiac snorkel as well as a superior mesenteric artery stent. Gastroenterology was consulted for evaluation of complaints of dysphagia along with imaging findings which showed concern for esophageal obstruction with an abrupt change in caliber of the thoracic esophagus at the superior most aspect of the aneurysmal sac. An esophagogastroduodenoscopy (EGD) was performed which showed a mildly dilated proximal esophagus with an area of pulsatile, extrinsic compression in the middle and lower third of the esophagus from 25 to 40 cm. There was also a notable area consistent with early esophageal diverticulum noted at 25 to 27 cm.
Discussion: Dysphagia aortica is a rare but significant cause of dysphagia due to esophageal compression by the thoracic aorta. Diagnosis is largely based on imaging findings and clinical suspicion for esophageal obstruction. There are several associated risk factors for developing dysphagia aortica including: advanced age, females, short statute, and significant kyphosis. Treatment options mainly focus on correcting the underlying aortic pathology and often require surgical intervention with either endovascular repair or open surgical repair to relieve the esophageal compression and prevent complications such as aortic rupture.
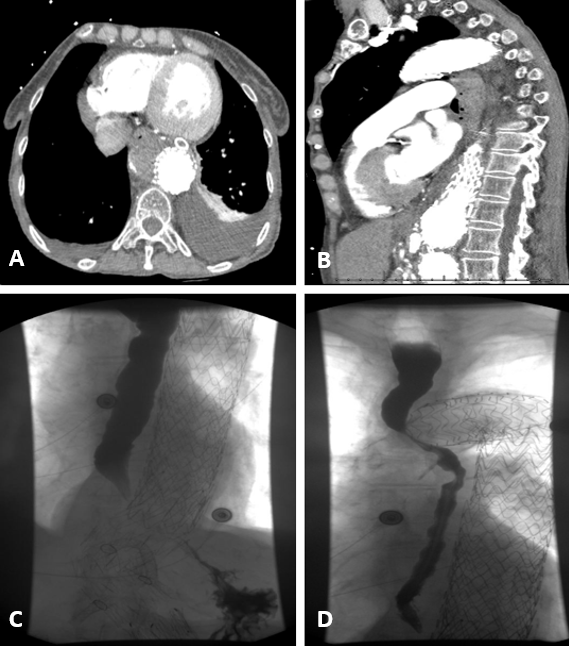
Figure: A: CTA chest transverse view showing extrinsic esophageal compression between thoracoabdominal aneurysm and left atrium and left ventricle.
B: CTA chest sagittal view showing extrinsic esophageal compression between thoracoabdominal aneurysm and left atrium and left ventricle.
C: Upper GI fluoroscopic exam showing lower thoracoabdominal aneurysmal stent with distal esophageal compression and delayed contrast progression.
D: Upper GI fluoroscopic exam showing upper portion of thoracoabdominal aneurysmal stent with proximal esophageal compression and delayed contrast progression.
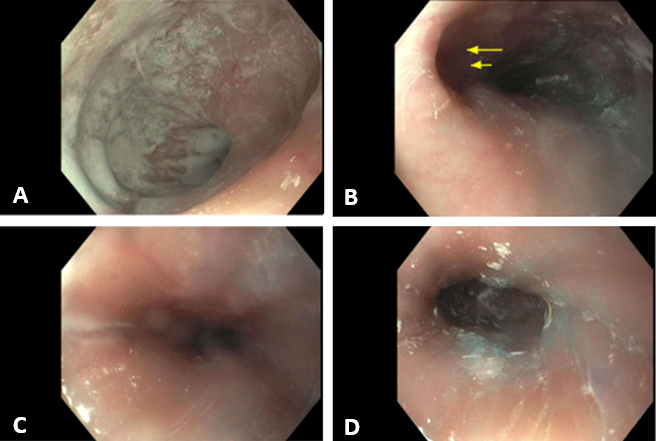
Figure: A: Dilated upper third of esophagus.
B: Middle third of esophagus with early diverticulum (double arrows).
C: Middle third of esophagus with extrinsic compression.
D: Lower third of esophagus with extrinsic compression.
Disclosures:
Hobie Hughes indicated no relevant financial relationships.
Lauren Healey indicated no relevant financial relationships.
Nathaniel Winstead indicated no relevant financial relationships.
Jonathan Francis indicated no relevant financial relationships.
Matthew Eves indicated no relevant financial relationships.
Hobie L. Hughes, DO1, Lauren Healey, DO2, Nathaniel Winstead, MD, MSPH, FACG1, Jonathan Francis, MD1, Matthew Eves, MD1. P0695 - Aortic Compression: Unveiling Dysphagia Aortica in the Elderly, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
