Sunday Poster Session
Category: Esophagus
P0694 - Primary Achalasia in a Patient With Hepatocellular Carcinoma: Using TIPS and Splenic Embolization to Allow for Pneumatic Dilation
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Makell S. Brown, BSPH (he/him/his)
Atrium Health Wake Forest Baptist
Winston-Salem, NC
Presenting Author(s)
Makell S. Brown, BSPH1, Brian Kouri, MD1, Steven B. Clayton, MD2
1Atrium Health Wake Forest Baptist, Winston-Salem, NC; 2Wake Forest University School of Medicine, Winston-Salem, NC
Introduction: Achalasia is an esophageal motility disorder characterized by the degeneration of ganglion cells in the myenteric plexus, resulting in an unopposed excitatory esophagus and aperistalsis. It is a relatively rare condition, with an estimated prevalence of 10.82/100,000. This case report details a patient with hepatocellular carcinoma, esophageal varices, and thrombocytopenia diagnosed with primary achalasia. To allow for pneumatic dilation of the esophagus, he was innovatively treated with transjugular intrahepatic portosystemic shunt (TIPS) in conjunction with partial splenic embolization to decrease portal hypertension and address the patient’s thrombocytopenia.
Case Description/
Methods: A 73-year-old white male with a history of cirrhosis with metastatic hepatocellular carcinoma presented at our institution for evaluation of dysphagia and regurgitation that progressively worsened over the past two years. The difficulty swallowing contributed to his 40-pound weight loss over the two years. Labs revealed a mild thrombocytopenia. Timed Barium Esophagogram (TBE) revealed a persistent contrast column and a beaked appearance of the esophagus, consistent with Achalasia. EUS found small submucosal esophageal varices in the distal esophagus. Per oral endoscopic myotomy (POEM), laparoscopic Heller myotomy, and pneumatic dilation were deemed too risky due to the presence of esophageal varices. A transjugular intrahepatic portosystemic shunt (TIPS) with splenic embolization was placed to reduce portal pressure and address the patient’s underlying thrombocytopenia. The procedure successfully decompressed the varices and reduced the amount of viable splenic tissue, which increased the patient’s platelet count from 51*103/ μL to 87*103/ μL. Pneumatic dilation was then performed to improve symptoms due to achalasia. Since the dilation, the patient has improved clinically, Eckardt score 1.
Discussion: Our case is unique to the literature, as our patient was diagnosed with hepatocellular carcinoma (HCC), liver cirrhosis complicated by portal hypertensive gastropathy, esophageal varices, thrombocytopenia, and had radiographic and endoscopic findings consistent with primary achalasia. Primary achalasia in this patient population is a scarce phenomenon, with only one case mentioned in the literature. TIPS was an effective method to reduce portal hypertension and allow for pneumatic dilation, highlighting an effective treatment option to provide care for a unique population.

Figure: Figure 1. Timed barium esophagogram revealing persistent contrast column with beaked appearance of the esophagogastric junction
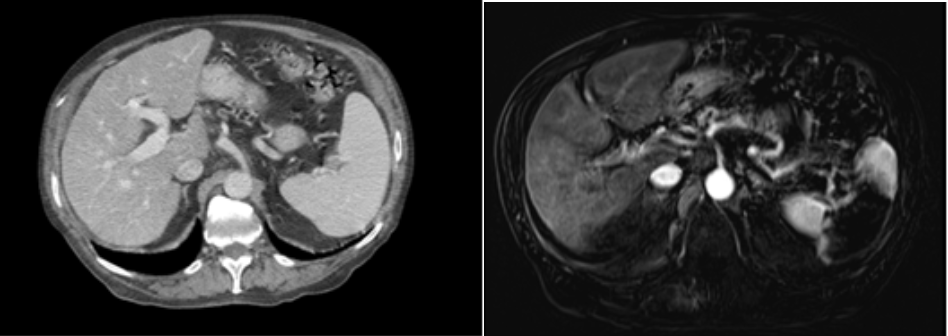
Figure: Figure 2. Computed Tomography (CT) before splenic embolization (left) and after (right), highlighting the decrease in viable splenic tissue.
Disclosures:
Makell Brown indicated no relevant financial relationships.
Brian Kouri indicated no relevant financial relationships.
Steven Clayton indicated no relevant financial relationships.
Makell S. Brown, BSPH1, Brian Kouri, MD1, Steven B. Clayton, MD2. P0694 - Primary Achalasia in a Patient With Hepatocellular Carcinoma: Using TIPS and Splenic Embolization to Allow for Pneumatic Dilation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Atrium Health Wake Forest Baptist, Winston-Salem, NC; 2Wake Forest University School of Medicine, Winston-Salem, NC
Introduction: Achalasia is an esophageal motility disorder characterized by the degeneration of ganglion cells in the myenteric plexus, resulting in an unopposed excitatory esophagus and aperistalsis. It is a relatively rare condition, with an estimated prevalence of 10.82/100,000. This case report details a patient with hepatocellular carcinoma, esophageal varices, and thrombocytopenia diagnosed with primary achalasia. To allow for pneumatic dilation of the esophagus, he was innovatively treated with transjugular intrahepatic portosystemic shunt (TIPS) in conjunction with partial splenic embolization to decrease portal hypertension and address the patient’s thrombocytopenia.
Case Description/
Methods: A 73-year-old white male with a history of cirrhosis with metastatic hepatocellular carcinoma presented at our institution for evaluation of dysphagia and regurgitation that progressively worsened over the past two years. The difficulty swallowing contributed to his 40-pound weight loss over the two years. Labs revealed a mild thrombocytopenia. Timed Barium Esophagogram (TBE) revealed a persistent contrast column and a beaked appearance of the esophagus, consistent with Achalasia. EUS found small submucosal esophageal varices in the distal esophagus. Per oral endoscopic myotomy (POEM), laparoscopic Heller myotomy, and pneumatic dilation were deemed too risky due to the presence of esophageal varices. A transjugular intrahepatic portosystemic shunt (TIPS) with splenic embolization was placed to reduce portal pressure and address the patient’s underlying thrombocytopenia. The procedure successfully decompressed the varices and reduced the amount of viable splenic tissue, which increased the patient’s platelet count from 51*103/ μL to 87*103/ μL. Pneumatic dilation was then performed to improve symptoms due to achalasia. Since the dilation, the patient has improved clinically, Eckardt score 1.
Discussion: Our case is unique to the literature, as our patient was diagnosed with hepatocellular carcinoma (HCC), liver cirrhosis complicated by portal hypertensive gastropathy, esophageal varices, thrombocytopenia, and had radiographic and endoscopic findings consistent with primary achalasia. Primary achalasia in this patient population is a scarce phenomenon, with only one case mentioned in the literature. TIPS was an effective method to reduce portal hypertension and allow for pneumatic dilation, highlighting an effective treatment option to provide care for a unique population.

Figure: Figure 1. Timed barium esophagogram revealing persistent contrast column with beaked appearance of the esophagogastric junction
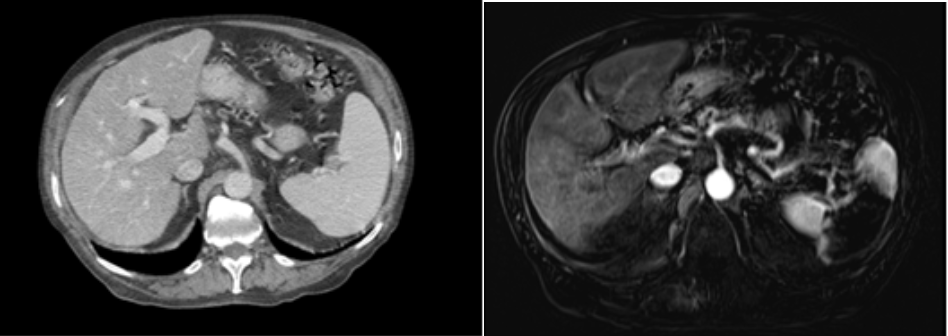
Figure: Figure 2. Computed Tomography (CT) before splenic embolization (left) and after (right), highlighting the decrease in viable splenic tissue.
Disclosures:
Makell Brown indicated no relevant financial relationships.
Brian Kouri indicated no relevant financial relationships.
Steven Clayton indicated no relevant financial relationships.
Makell S. Brown, BSPH1, Brian Kouri, MD1, Steven B. Clayton, MD2. P0694 - Primary Achalasia in a Patient With Hepatocellular Carcinoma: Using TIPS and Splenic Embolization to Allow for Pneumatic Dilation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

