Sunday Poster Session
Category: Esophagus
P0687 - An Unusual Case of Hematemesis: Sevelamer-Induced Esophageal Ulceration
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- ZK
Zach Kovach, MD
West Virginia University School of Medicine
Morgantown, WV
Presenting Author(s)
Zach Kovach, MD1, Joey Simmons, MD1, Justin Kupec, MD, FACG1, William Hsueh, MD2
1West Virginia University School of Medicine, Morgantown, WV; 2Visalia Medical Clinic, Adventist Health Physicians Network, Visalia, CA
Introduction: Patients with end-stage renal disease on hemodialysis frequently struggle with electrolyte derangements. For those with poorly controlled hyperphosphatemia, phosphate binders such as sevelamer are routinely prescribed to facilitate fecal excretion of dietary phosphorus. Sevelamer is a non-absorbable polyamine resin activated by gastric acids which binds intraluminal phosphate. In rare cases sevelamer polymers crystallize within the mucosa of the gastrointestinal tract, resulting in mucosal inflammation, pseudopolyps, ulceration, ischemia or necrosis. Sevelamer-induced gastrointestinal mucosal injury (SIGMI) should be suspected in those with gastrointestinal bleeding, abdominal pain, and diarrhea. Biopsy samples with H&E staining often reveal a non-polarizable “fish-scale” pattern with central pink stain and yellow/orange peripheral stain.
Case Description/
Methods: We present a case of a 78-year-old female with past medical history of diabetes, hypertension, and ESRD on HD who was admitted for evaluation of chest and lower back pain following mechanical fall. On the sixth day of admission, she produced 500 cc of coffee-ground emesis and underwent EGD revealing Grade C esophagitis with ulceration and nodular-appearing mucosa. The patient denied any NSAID or alcohol use. Tissue sampling found fragments of entrapped sevelamer crystals within fibrinopurulent exudate, along with focal superficial neutrophilic inflammation with parakeratosis and reactive changes consistent with acute esophagitis. Sevelamer was discontinued upon discharge and the patient was treated with pantoprazole 40 mg daily. At a 2 month follow up appointment, the patient had no reported recurrence of hematemesis.
Discussion: The overall incidence of SIGMI remains unknown, as treatment of hyperphosphatemia with this agent rarely results in severe complications. Fortunately, most patients with SIGMI fully recover following discontinuation of the drug, and adjuvant treatment with PPIs may facilitate ulcer healing. Among the limited case reports available, SIGMI of the colon is the most common, whereas the esophagus is least common. One proposed mechanism for this observation is thought to be related to delayed colonic transit effect from the drug itself. Given suspected temporal relationship with this complication, patients should be recommended to drink adequate fluids and remain upright after taking this oral medication to decrease transit time and minimize risk of esophageal injury.
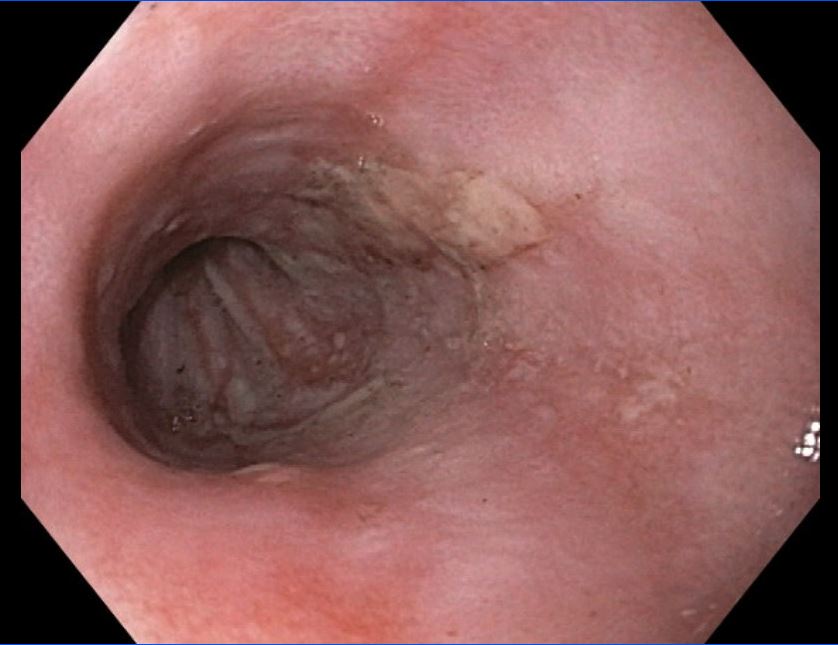
Figure: EGD revealing esophagitis with ulceration.
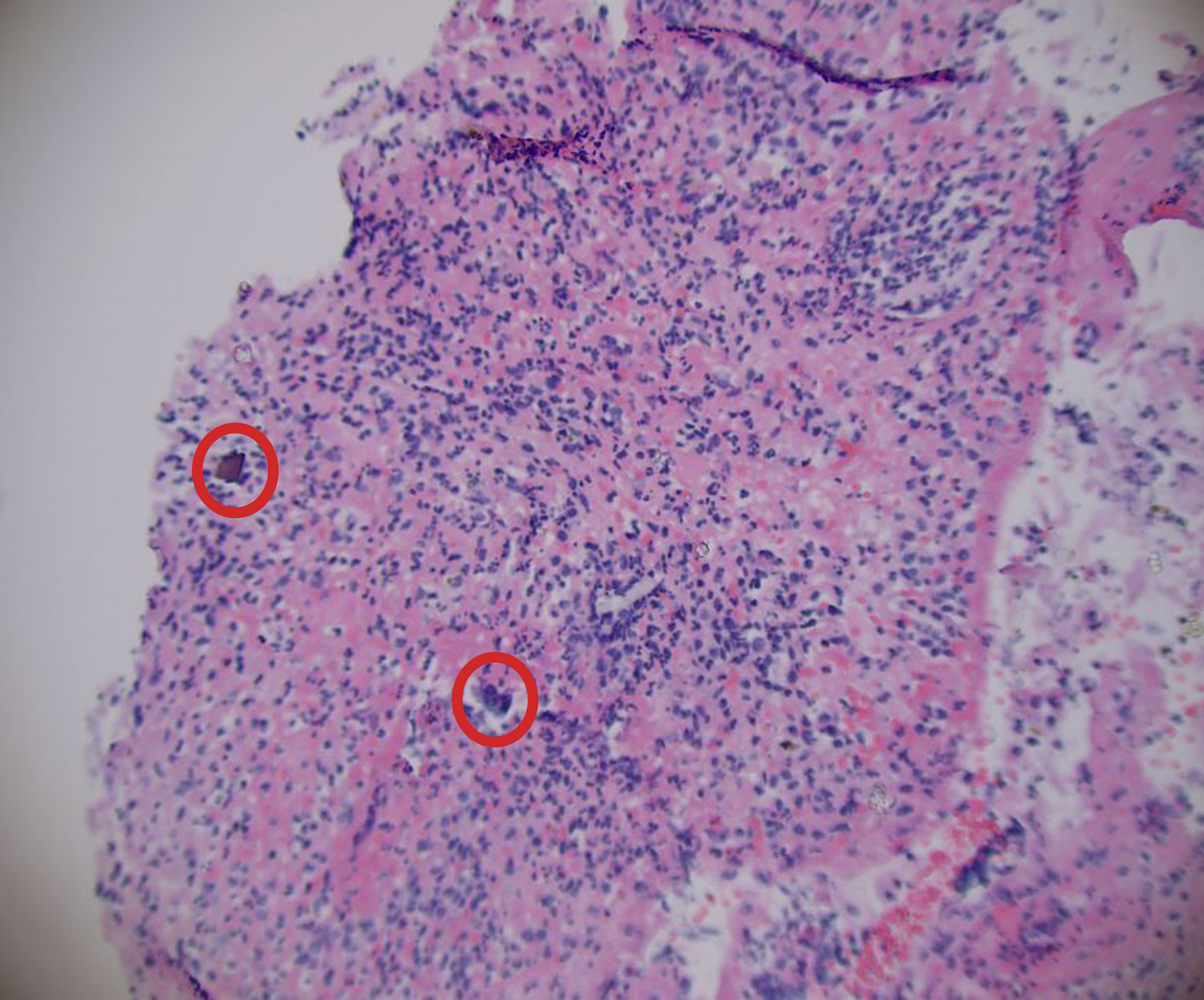
Figure: Biopsy sampling with H&E stain of esophageal ulceration revealing "fish-scale" sevelamer crystals (circled in red).
Disclosures:
Zach Kovach indicated no relevant financial relationships.
Joey Simmons indicated no relevant financial relationships.
Justin Kupec indicated no relevant financial relationships.
William Hsueh indicated no relevant financial relationships.
Zach Kovach, MD1, Joey Simmons, MD1, Justin Kupec, MD, FACG1, William Hsueh, MD2. P0687 - An Unusual Case of Hematemesis: Sevelamer-Induced Esophageal Ulceration, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1West Virginia University School of Medicine, Morgantown, WV; 2Visalia Medical Clinic, Adventist Health Physicians Network, Visalia, CA
Introduction: Patients with end-stage renal disease on hemodialysis frequently struggle with electrolyte derangements. For those with poorly controlled hyperphosphatemia, phosphate binders such as sevelamer are routinely prescribed to facilitate fecal excretion of dietary phosphorus. Sevelamer is a non-absorbable polyamine resin activated by gastric acids which binds intraluminal phosphate. In rare cases sevelamer polymers crystallize within the mucosa of the gastrointestinal tract, resulting in mucosal inflammation, pseudopolyps, ulceration, ischemia or necrosis. Sevelamer-induced gastrointestinal mucosal injury (SIGMI) should be suspected in those with gastrointestinal bleeding, abdominal pain, and diarrhea. Biopsy samples with H&E staining often reveal a non-polarizable “fish-scale” pattern with central pink stain and yellow/orange peripheral stain.
Case Description/
Methods: We present a case of a 78-year-old female with past medical history of diabetes, hypertension, and ESRD on HD who was admitted for evaluation of chest and lower back pain following mechanical fall. On the sixth day of admission, she produced 500 cc of coffee-ground emesis and underwent EGD revealing Grade C esophagitis with ulceration and nodular-appearing mucosa. The patient denied any NSAID or alcohol use. Tissue sampling found fragments of entrapped sevelamer crystals within fibrinopurulent exudate, along with focal superficial neutrophilic inflammation with parakeratosis and reactive changes consistent with acute esophagitis. Sevelamer was discontinued upon discharge and the patient was treated with pantoprazole 40 mg daily. At a 2 month follow up appointment, the patient had no reported recurrence of hematemesis.
Discussion: The overall incidence of SIGMI remains unknown, as treatment of hyperphosphatemia with this agent rarely results in severe complications. Fortunately, most patients with SIGMI fully recover following discontinuation of the drug, and adjuvant treatment with PPIs may facilitate ulcer healing. Among the limited case reports available, SIGMI of the colon is the most common, whereas the esophagus is least common. One proposed mechanism for this observation is thought to be related to delayed colonic transit effect from the drug itself. Given suspected temporal relationship with this complication, patients should be recommended to drink adequate fluids and remain upright after taking this oral medication to decrease transit time and minimize risk of esophageal injury.
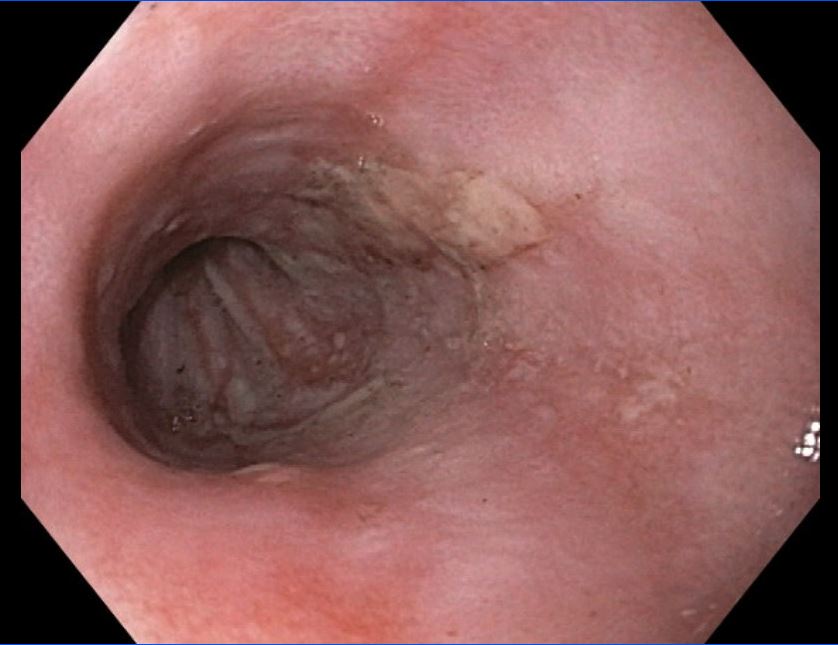
Figure: EGD revealing esophagitis with ulceration.
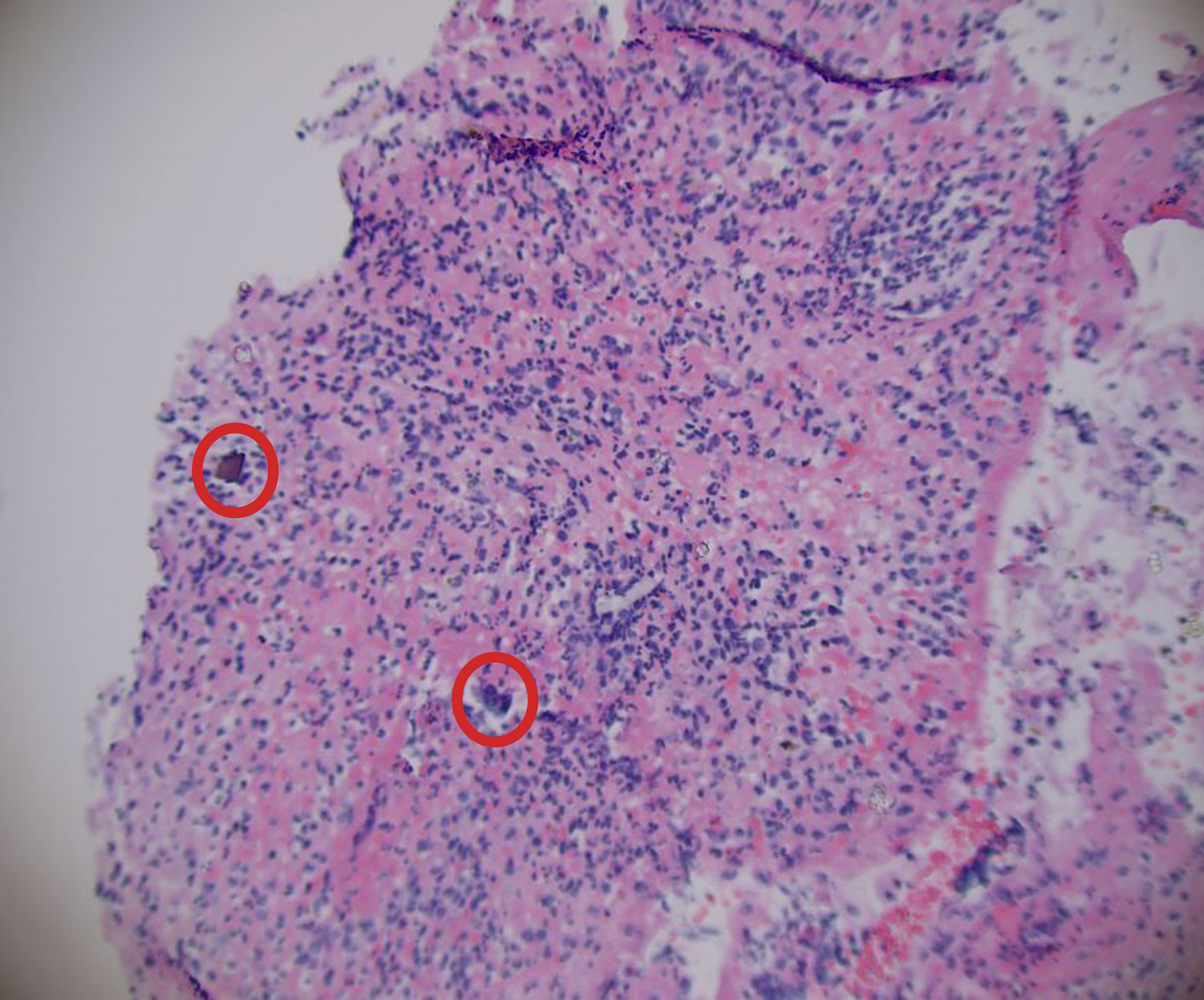
Figure: Biopsy sampling with H&E stain of esophageal ulceration revealing "fish-scale" sevelamer crystals (circled in red).
Disclosures:
Zach Kovach indicated no relevant financial relationships.
Joey Simmons indicated no relevant financial relationships.
Justin Kupec indicated no relevant financial relationships.
William Hsueh indicated no relevant financial relationships.
Zach Kovach, MD1, Joey Simmons, MD1, Justin Kupec, MD, FACG1, William Hsueh, MD2. P0687 - An Unusual Case of Hematemesis: Sevelamer-Induced Esophageal Ulceration, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
