Sunday Poster Session
Category: Functional Bowel Disease
P0783 - Association of Body Mass Index with Prevalence and Burden of Disorders of Gut-Brain Interaction: Data from the Rome Foundation Global Epidemiology Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Daniel M. Simadibrata, MD
Case Western Reserve University / MetroHealth
Cleveland, OH
Presenting Author(s)
Daniel M. Simadibrata, MD1, Noppachai Siranart, MD2, Zaid Al-Fakhouri, MD1, Laith Alomari, MD3, Benjamin Liu, MD1, Ami Sperber, MD, MSPH4, Olafur Palsson, 5, Shrikant Bangdiwala, PhD6, Yeong Yeh Lee, MD, PhD7
1Case Western Reserve University / MetroHealth, Cleveland, OH; 2Brigham and Women's Hospital, Boston, MA; 3Thomas Jefferson University, Philadelphia, PA; 4Joyce & Irving Goldman Medical School, Ben-Gurion University of the Negev, Kibbutz Paord, HaZafon, Israel; 5University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC; 6McMaster University, Hamilton, ON, Canada; 7Universiti Sains Malaysia, Kota Bharu, Kelantan, Malaysia
Introduction: The double burden of malnutrition, encompassing both undernutrition and obesity, presents with significant global health challenges; however, its association with disorders of gut-brain interaction (DGBI) remains inadequately explored. This study aims to comprehensively assess the prevalence of DGBI across body mass index (BMI) categories, elucidate associations between BMI and any DGBI as well as anatomically specific DGBI, and evaluate the impact of BMI on clinical burden of DGBI.
Methods: We analyzed data from the Rome Foundation Global Epidemiology Study, an internet-based survey involving 26 countries, focusing on participants with available BMI data. Participants were categorized based on World Health Organization-defined BMI standards: underweight (< 18.5 kg/m2), normal weight (18.5-24.9 kg/m2), overweight (25.0-29.9 kg/m2), obesity class I (30.0-34.9 kg/m2), obesity class II (35.0-39.9 kg/m2), and obesity class III (≥40.0 kg/m2). Presence of DGBI was determined according to the Rome IV Diagnostic Criteria. Logistic regression analyses calculated odds ratios (OR) and 95% confidence interval (95%CI) for any DGBI, with normal weight as the reference group.
Results: Among 48,359 respondents (2,308 [4.7%] underweight; 8,337 [17.2%] with obesity), the highest prevalence of DGBI was observed among participants with obesity class III (57.37%; 95%CI 54.28–60.41%) and underweight (48.74%; 95%CI 46.71–50.78%), demonstrating a U-shaped distribution (OR for obesity class III 1.86; 95%CI 1.63-2.11; Figure 1A). Moreover, higher BMI was associated with a greater number of overlapping DGBI diagnoses, particularly among the underweight and obesity categories (Figure 1B). Anatomical subgroup analysis demonstrated that the U-shaped association persisted consistently across all DGBI regions, with obesity class III, obesity class II, and underweight exhibiting the highest risks (Figure 2). Furthermore, among DGBI patients, those in the underweight and severe obesity groups (classes II and III) reported significantly lower PROMIS-10 Physical and Mental Health scores and higher PHQ-12 somatization scores compared with normal weight individuals (p< 0.05).
Discussion: This global study highlights a clear U-shaped association between BMI and DGBI prevalence, emphasizing the role of undernutrition and severe obesity in DGBI. Higher BMI is strongly linked to increased overlapping DGBI diagnoses, heightened somatization, and lower quality of life among patients with DGBI.
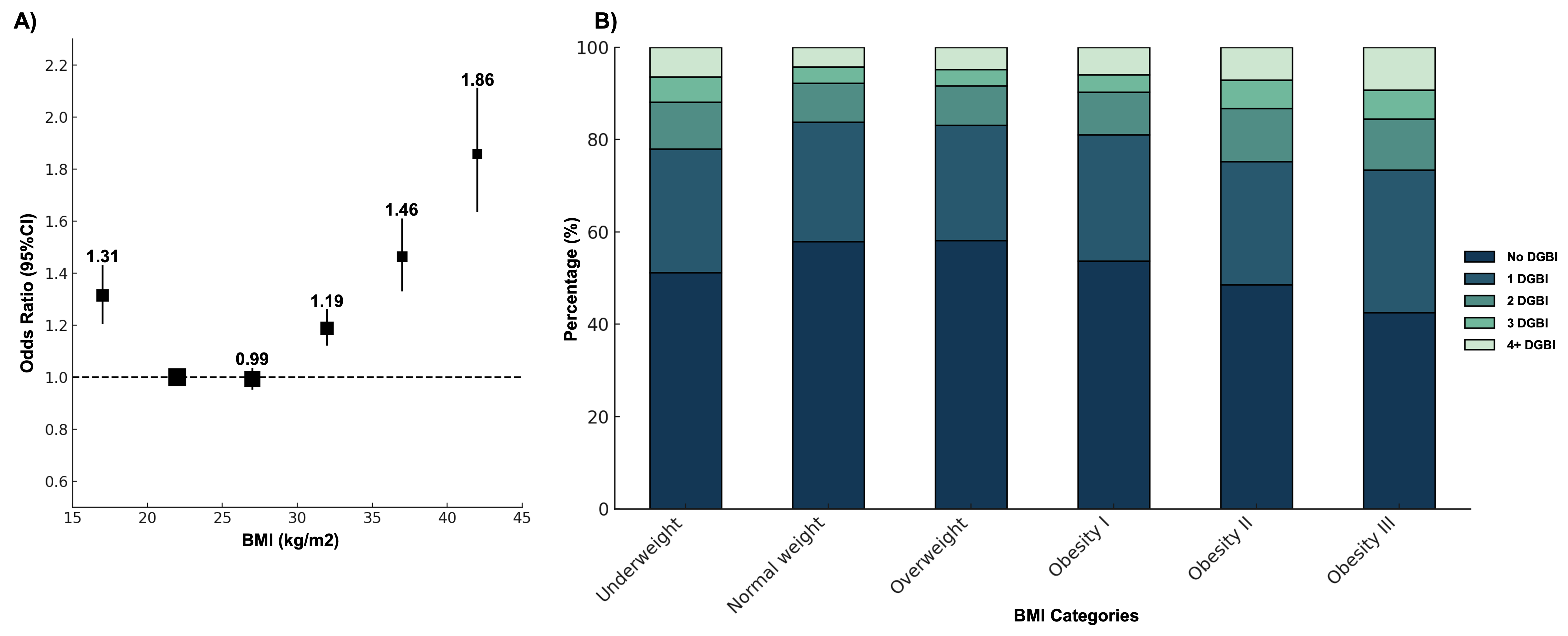
Figure: Figure 1. A) Association Between Body Mass Index (BMI) and Disorders of Gut-Brain Interaction (DGBI). B) Distribution of Number of Overlapping DGBI Diagnoses by BMI Categories.
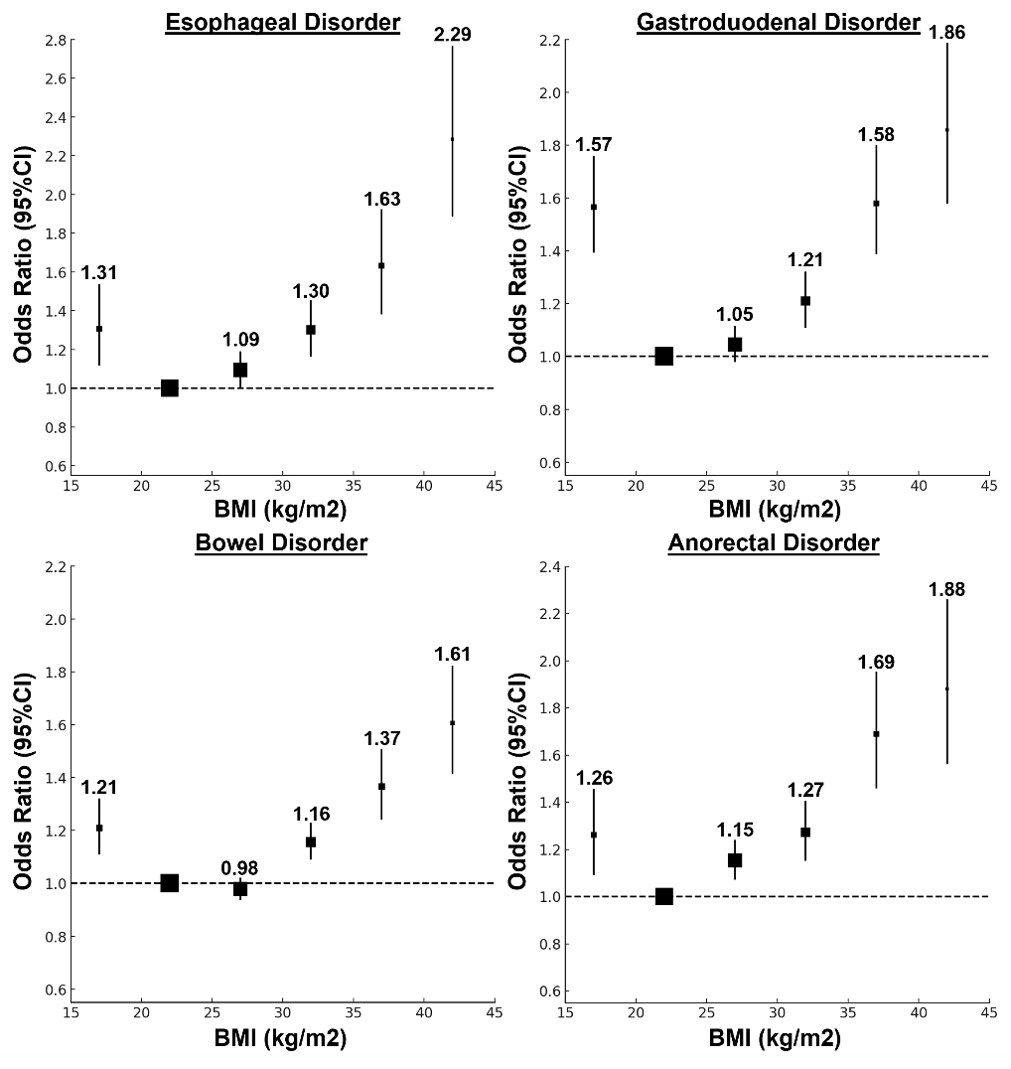
Figure: Figure 2. Association Between Body Mass Index and Disorders of Gut-Brain Interaction based on Anatomical Regions.
Disclosures:
Daniel Simadibrata indicated no relevant financial relationships.
Noppachai Siranart indicated no relevant financial relationships.
Zaid Al-Fakhouri indicated no relevant financial relationships.
Laith Alomari indicated no relevant financial relationships.
Benjamin Liu indicated no relevant financial relationships.
Ami Sperber indicated no relevant financial relationships.
Olafur Palsson indicated no relevant financial relationships.
Shrikant Bangdiwala indicated no relevant financial relationships.
Yeong Yeh Lee indicated no relevant financial relationships.
Daniel M. Simadibrata, MD1, Noppachai Siranart, MD2, Zaid Al-Fakhouri, MD1, Laith Alomari, MD3, Benjamin Liu, MD1, Ami Sperber, MD, MSPH4, Olafur Palsson, 5, Shrikant Bangdiwala, PhD6, Yeong Yeh Lee, MD, PhD7. P0783 - Association of Body Mass Index with Prevalence and Burden of Disorders of Gut-Brain Interaction: Data from the Rome Foundation Global Epidemiology Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Case Western Reserve University / MetroHealth, Cleveland, OH; 2Brigham and Women's Hospital, Boston, MA; 3Thomas Jefferson University, Philadelphia, PA; 4Joyce & Irving Goldman Medical School, Ben-Gurion University of the Negev, Kibbutz Paord, HaZafon, Israel; 5University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC; 6McMaster University, Hamilton, ON, Canada; 7Universiti Sains Malaysia, Kota Bharu, Kelantan, Malaysia
Introduction: The double burden of malnutrition, encompassing both undernutrition and obesity, presents with significant global health challenges; however, its association with disorders of gut-brain interaction (DGBI) remains inadequately explored. This study aims to comprehensively assess the prevalence of DGBI across body mass index (BMI) categories, elucidate associations between BMI and any DGBI as well as anatomically specific DGBI, and evaluate the impact of BMI on clinical burden of DGBI.
Methods: We analyzed data from the Rome Foundation Global Epidemiology Study, an internet-based survey involving 26 countries, focusing on participants with available BMI data. Participants were categorized based on World Health Organization-defined BMI standards: underweight (< 18.5 kg/m2), normal weight (18.5-24.9 kg/m2), overweight (25.0-29.9 kg/m2), obesity class I (30.0-34.9 kg/m2), obesity class II (35.0-39.9 kg/m2), and obesity class III (≥40.0 kg/m2). Presence of DGBI was determined according to the Rome IV Diagnostic Criteria. Logistic regression analyses calculated odds ratios (OR) and 95% confidence interval (95%CI) for any DGBI, with normal weight as the reference group.
Results: Among 48,359 respondents (2,308 [4.7%] underweight; 8,337 [17.2%] with obesity), the highest prevalence of DGBI was observed among participants with obesity class III (57.37%; 95%CI 54.28–60.41%) and underweight (48.74%; 95%CI 46.71–50.78%), demonstrating a U-shaped distribution (OR for obesity class III 1.86; 95%CI 1.63-2.11; Figure 1A). Moreover, higher BMI was associated with a greater number of overlapping DGBI diagnoses, particularly among the underweight and obesity categories (Figure 1B). Anatomical subgroup analysis demonstrated that the U-shaped association persisted consistently across all DGBI regions, with obesity class III, obesity class II, and underweight exhibiting the highest risks (Figure 2). Furthermore, among DGBI patients, those in the underweight and severe obesity groups (classes II and III) reported significantly lower PROMIS-10 Physical and Mental Health scores and higher PHQ-12 somatization scores compared with normal weight individuals (p< 0.05).
Discussion: This global study highlights a clear U-shaped association between BMI and DGBI prevalence, emphasizing the role of undernutrition and severe obesity in DGBI. Higher BMI is strongly linked to increased overlapping DGBI diagnoses, heightened somatization, and lower quality of life among patients with DGBI.
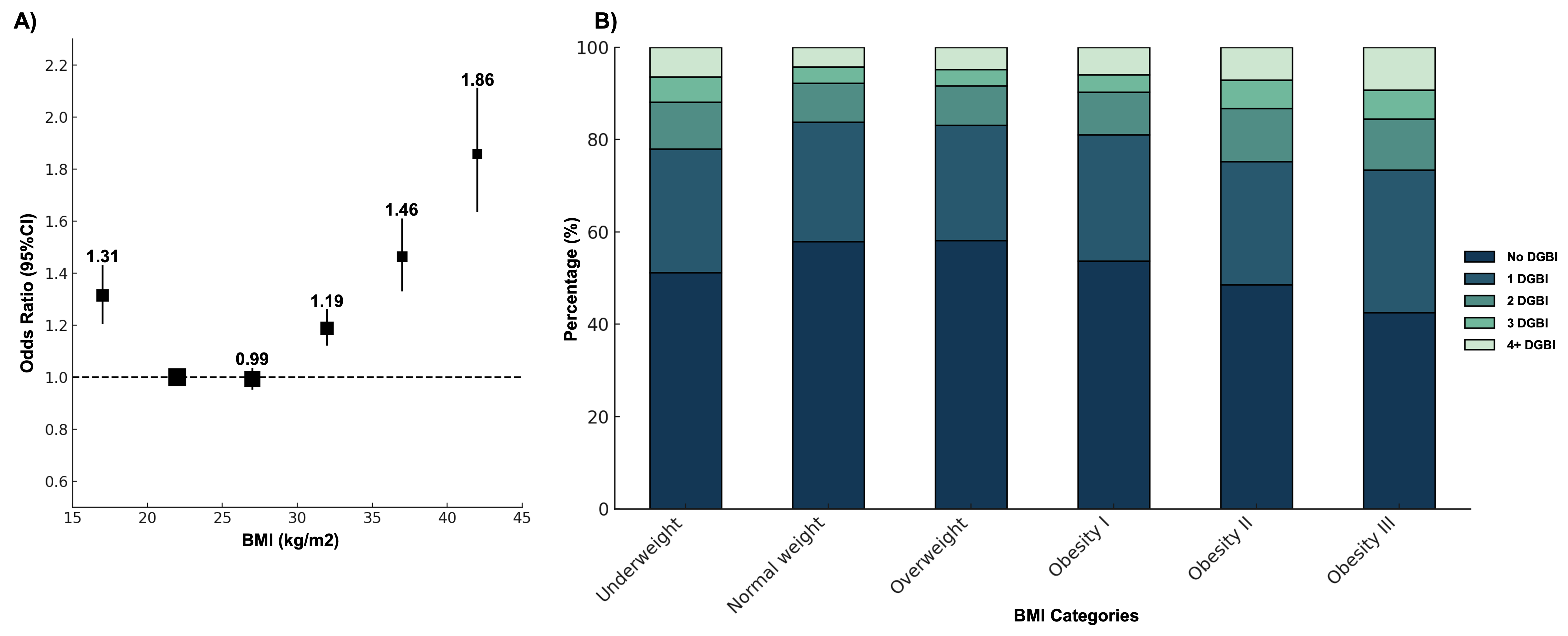
Figure: Figure 1. A) Association Between Body Mass Index (BMI) and Disorders of Gut-Brain Interaction (DGBI). B) Distribution of Number of Overlapping DGBI Diagnoses by BMI Categories.
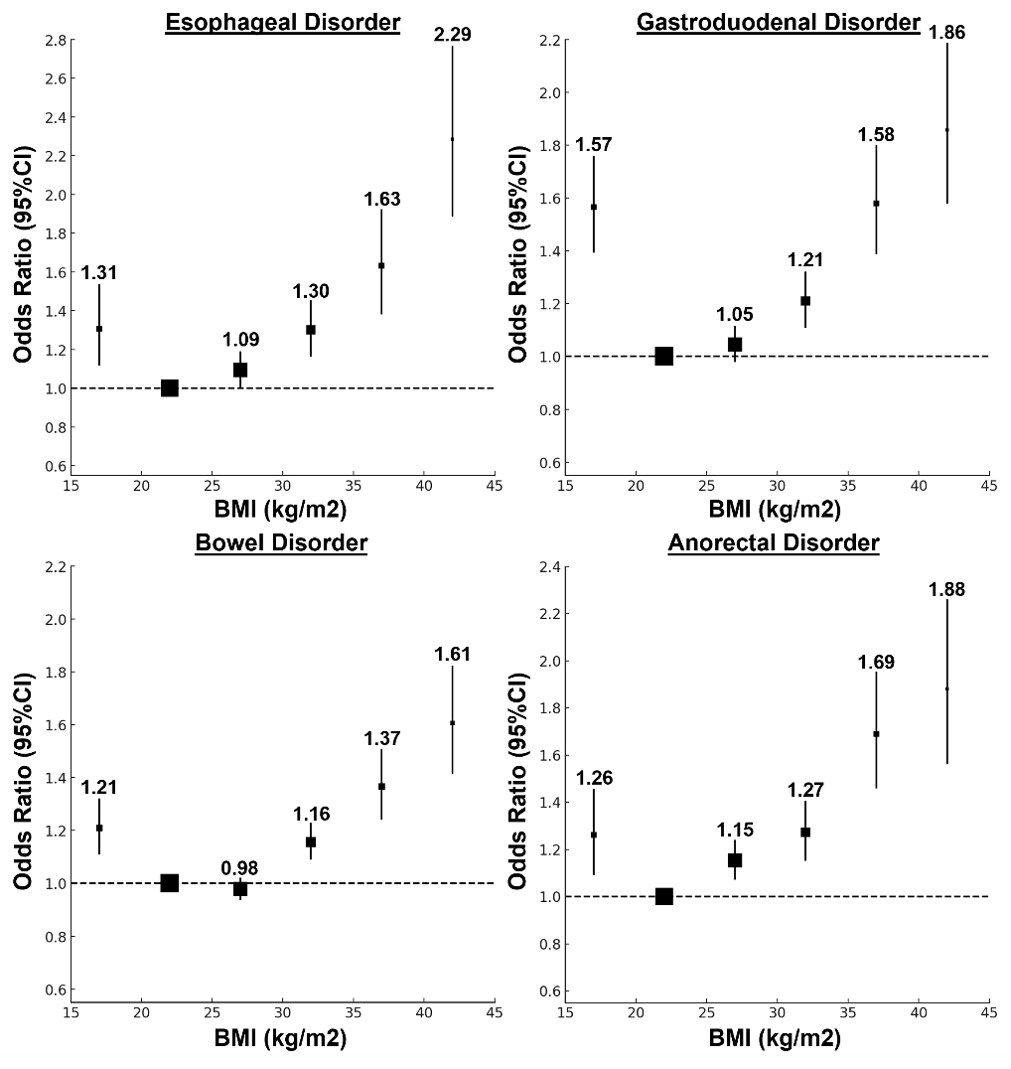
Figure: Figure 2. Association Between Body Mass Index and Disorders of Gut-Brain Interaction based on Anatomical Regions.
Disclosures:
Daniel Simadibrata indicated no relevant financial relationships.
Noppachai Siranart indicated no relevant financial relationships.
Zaid Al-Fakhouri indicated no relevant financial relationships.
Laith Alomari indicated no relevant financial relationships.
Benjamin Liu indicated no relevant financial relationships.
Ami Sperber indicated no relevant financial relationships.
Olafur Palsson indicated no relevant financial relationships.
Shrikant Bangdiwala indicated no relevant financial relationships.
Yeong Yeh Lee indicated no relevant financial relationships.
Daniel M. Simadibrata, MD1, Noppachai Siranart, MD2, Zaid Al-Fakhouri, MD1, Laith Alomari, MD3, Benjamin Liu, MD1, Ami Sperber, MD, MSPH4, Olafur Palsson, 5, Shrikant Bangdiwala, PhD6, Yeong Yeh Lee, MD, PhD7. P0783 - Association of Body Mass Index with Prevalence and Burden of Disorders of Gut-Brain Interaction: Data from the Rome Foundation Global Epidemiology Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
