Sunday Poster Session
Category: Functional Bowel Disease
P0781 - Prevalence and Prescription Patterns of IBS Treatments Across Demographic and Socioeconomic Factors
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Anthony Kerbage, MD
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Anthony Kerbage, MD1, Yueqi Wu, MPH2, Madison Simons, PhD1, Judy Nee, MD3, Samita Garg, MD1, Scott L. Gabbard, MD, FACG4, Anthony Lembo, MD, FACG1
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic Foundation, Ypsilanti, MI; 3Beth Israel Deaconess Medical Center, Boston, MA; 4Cleveland Clinic Foundation, Shaker Heights, OH
Introduction: Irritable bowel syndrome (IBS) is a common disorder of gut-brain interaction with diverse clinical features and management strategies. We aimed to evaluate treatment patterns for IBS and investigate demographic and socioeconomic disparities in management.
Methods: We used data from the All of Us Research Program, a large, diverse cohort launched by the NIH in 2018. Medication data included FDA-approved drugs for IBS, common off-label treatments (antispasmodics, antidepressants), and over-the-counter agents (fiber, osmotic/stimulant laxatives). Patients were stratified by age, sex, race, ethnicity, income, education, and insurance status. Chi-square and Fisher’s exact tests were used for categorical comparisons using R.
Results: Among 390,202 individuals in the database, 3.9% (n=14,897) were diagnosed with IBS. The majority (57%) were diagnosed between 36 and 65 years of age, were White (73%) and female (78%). The most commonly used medications for IBS-C were osmotic laxatives (18%), stimulant laxatives (9%), and fiber (6%). Prescription IBS-C drugs were used in only 2%. The most commonly prescribed IBS-D medication was loperamide (4%), with prescription IBS-D drugs also used in only 2%. For all IBS subtypes, antispasmodics (9%) and antidepressants (14%) were the most prescribed. Patients diagnosed at an earlier age were more likely to receive medications. Females were more likely to be prescribed antispasmodics (10% vs. 7%) and antidepressants (15% vs. 10%) than males. Black patients were more likely to be prescribed stimulant laxatives, particularly bisacodyl (10% vs. 4% in White and 2% in Asian patients). Asian patients were less likely to receive antidepressants (6% vs. 13% in Black and 15% in White patients). Hispanic patients were less likely to be prescribed antispasmodics (6% vs. 10%) or antidepressants (11% vs. 15%) than non-Hispanic patients. Uninsured patients were less likely to receive osmotic laxatives (11% vs. 18%), stimulant laxatives (5% vs. 9%), and antidepressants (7% vs. 14%).
Discussion: Our findings reveal notable variations in treatment patterns across race, ethnicity, and socioeconomic groups. Females were more frequently prescribed antispasmodics and antidepressants. Asian patients tended to use fewer IBS medications compared to their White and Black counterparts. These disparities highlight the need for further investigation into contributing factors, including differences in disease severity, access to care, and provider treatment preferences.
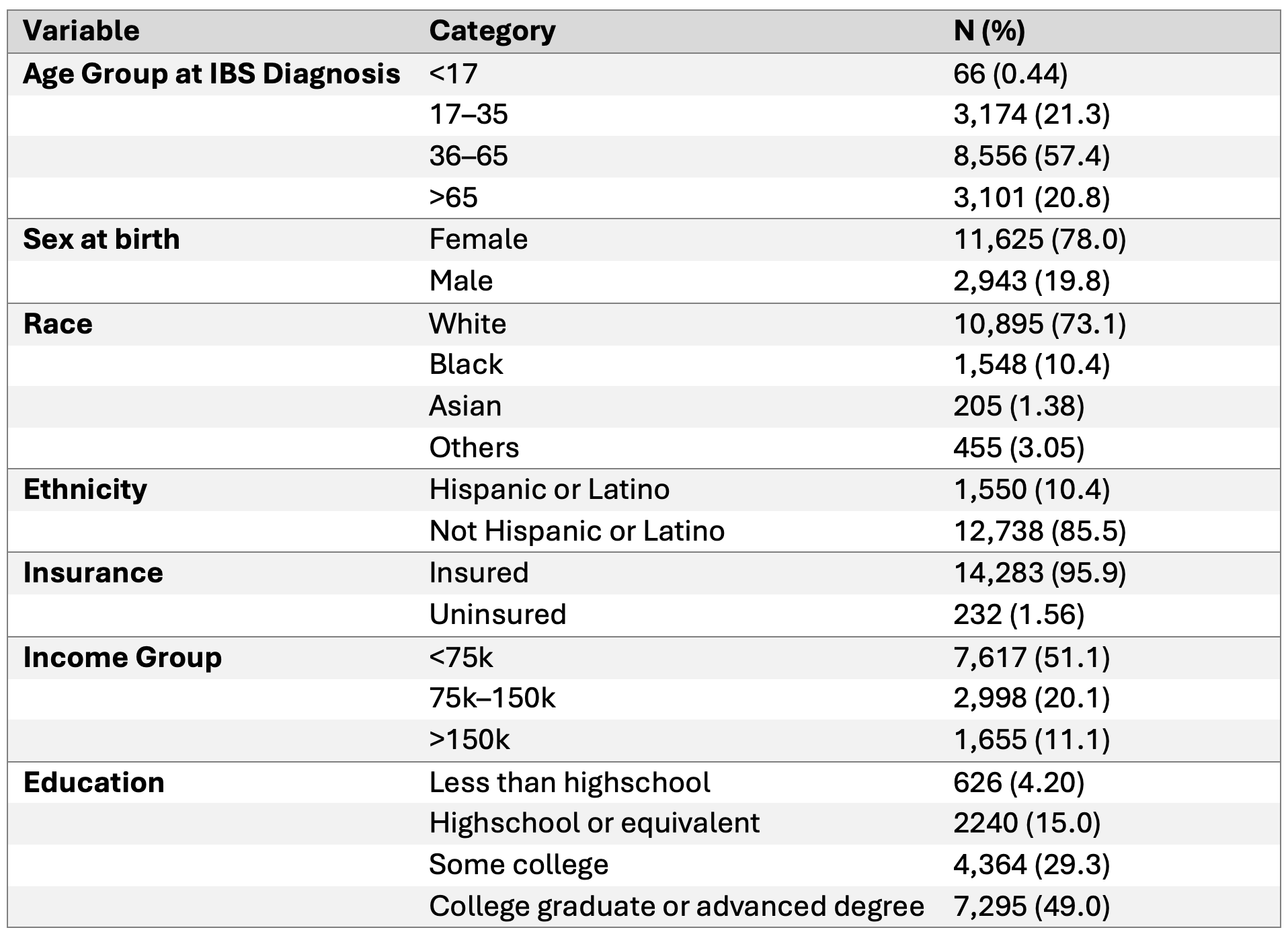
Figure: Figure 1. Demographics of IBS Patients
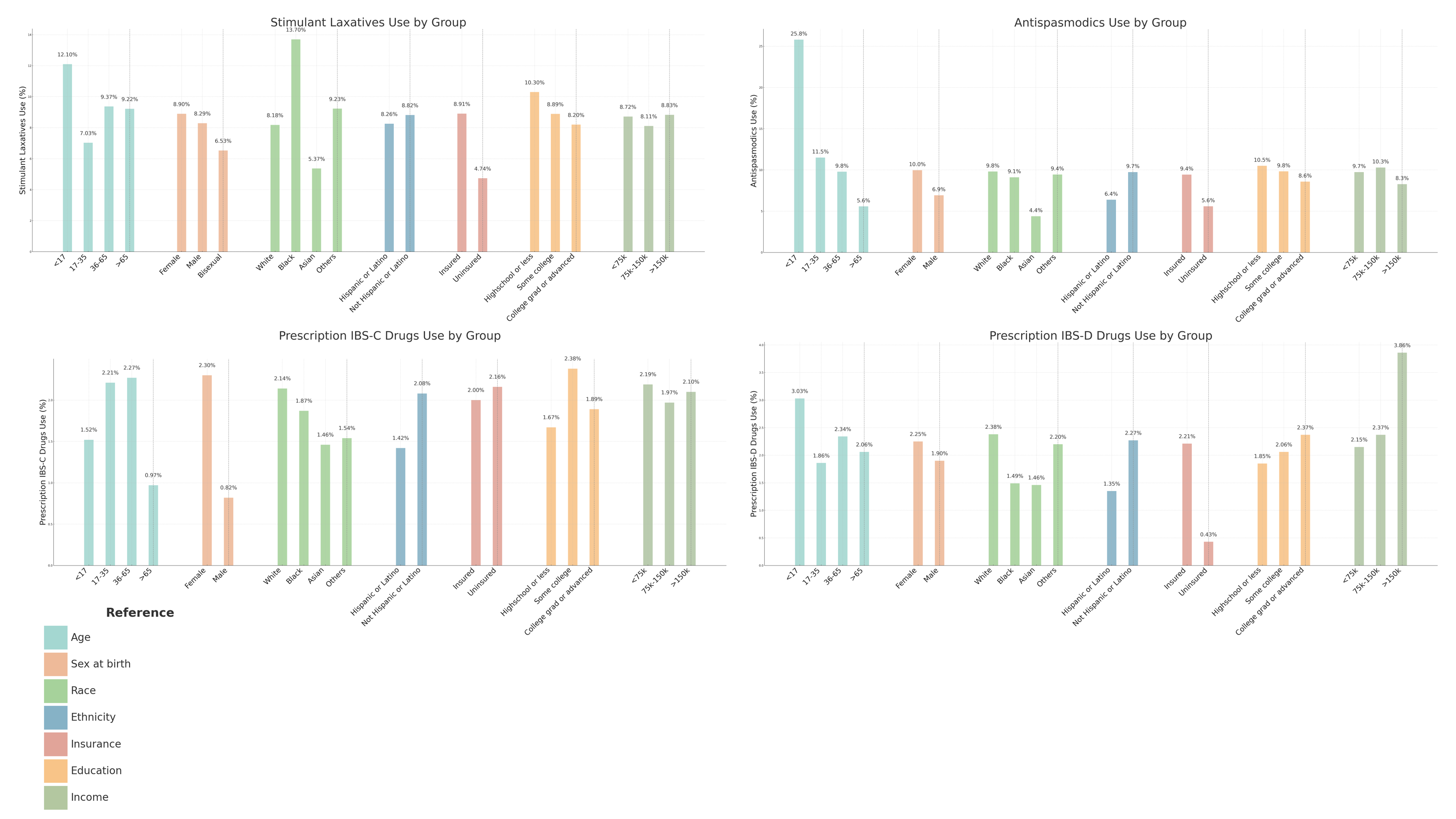
Figure: Figure 1. Stratified Analysis of IBS Medication Use Across Demographic and Socioeconomic Groups
Disclosures:
Anthony Kerbage indicated no relevant financial relationships.
Yueqi Wu indicated no relevant financial relationships.
Madison Simons indicated no relevant financial relationships.
Judy Nee: Fzata – Consultant.
Samita Garg indicated no relevant financial relationships.
Scott Gabbard: Gastrogirl – invited podcast talk.
Anthony Lembo: Allurion – Stock-publicly held company(excluding mutual/index funds). Ardeylx – Consultant. Atmo – Advisory Committee/Board Member. Bristol Myer Squibb – Stock-publicly held company(excluding mutual/index funds). GSK – Consultant. Ironwood – DSMB. J&J – Stock-publicly held company(excluding mutual/index funds). Salix – Consultant. Takeda – Consultant. Vibrant – Consultant.
Anthony Kerbage, MD1, Yueqi Wu, MPH2, Madison Simons, PhD1, Judy Nee, MD3, Samita Garg, MD1, Scott L. Gabbard, MD, FACG4, Anthony Lembo, MD, FACG1. P0781 - Prevalence and Prescription Patterns of IBS Treatments Across Demographic and Socioeconomic Factors, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic Foundation, Ypsilanti, MI; 3Beth Israel Deaconess Medical Center, Boston, MA; 4Cleveland Clinic Foundation, Shaker Heights, OH
Introduction: Irritable bowel syndrome (IBS) is a common disorder of gut-brain interaction with diverse clinical features and management strategies. We aimed to evaluate treatment patterns for IBS and investigate demographic and socioeconomic disparities in management.
Methods: We used data from the All of Us Research Program, a large, diverse cohort launched by the NIH in 2018. Medication data included FDA-approved drugs for IBS, common off-label treatments (antispasmodics, antidepressants), and over-the-counter agents (fiber, osmotic/stimulant laxatives). Patients were stratified by age, sex, race, ethnicity, income, education, and insurance status. Chi-square and Fisher’s exact tests were used for categorical comparisons using R.
Results: Among 390,202 individuals in the database, 3.9% (n=14,897) were diagnosed with IBS. The majority (57%) were diagnosed between 36 and 65 years of age, were White (73%) and female (78%). The most commonly used medications for IBS-C were osmotic laxatives (18%), stimulant laxatives (9%), and fiber (6%). Prescription IBS-C drugs were used in only 2%. The most commonly prescribed IBS-D medication was loperamide (4%), with prescription IBS-D drugs also used in only 2%. For all IBS subtypes, antispasmodics (9%) and antidepressants (14%) were the most prescribed. Patients diagnosed at an earlier age were more likely to receive medications. Females were more likely to be prescribed antispasmodics (10% vs. 7%) and antidepressants (15% vs. 10%) than males. Black patients were more likely to be prescribed stimulant laxatives, particularly bisacodyl (10% vs. 4% in White and 2% in Asian patients). Asian patients were less likely to receive antidepressants (6% vs. 13% in Black and 15% in White patients). Hispanic patients were less likely to be prescribed antispasmodics (6% vs. 10%) or antidepressants (11% vs. 15%) than non-Hispanic patients. Uninsured patients were less likely to receive osmotic laxatives (11% vs. 18%), stimulant laxatives (5% vs. 9%), and antidepressants (7% vs. 14%).
Discussion: Our findings reveal notable variations in treatment patterns across race, ethnicity, and socioeconomic groups. Females were more frequently prescribed antispasmodics and antidepressants. Asian patients tended to use fewer IBS medications compared to their White and Black counterparts. These disparities highlight the need for further investigation into contributing factors, including differences in disease severity, access to care, and provider treatment preferences.
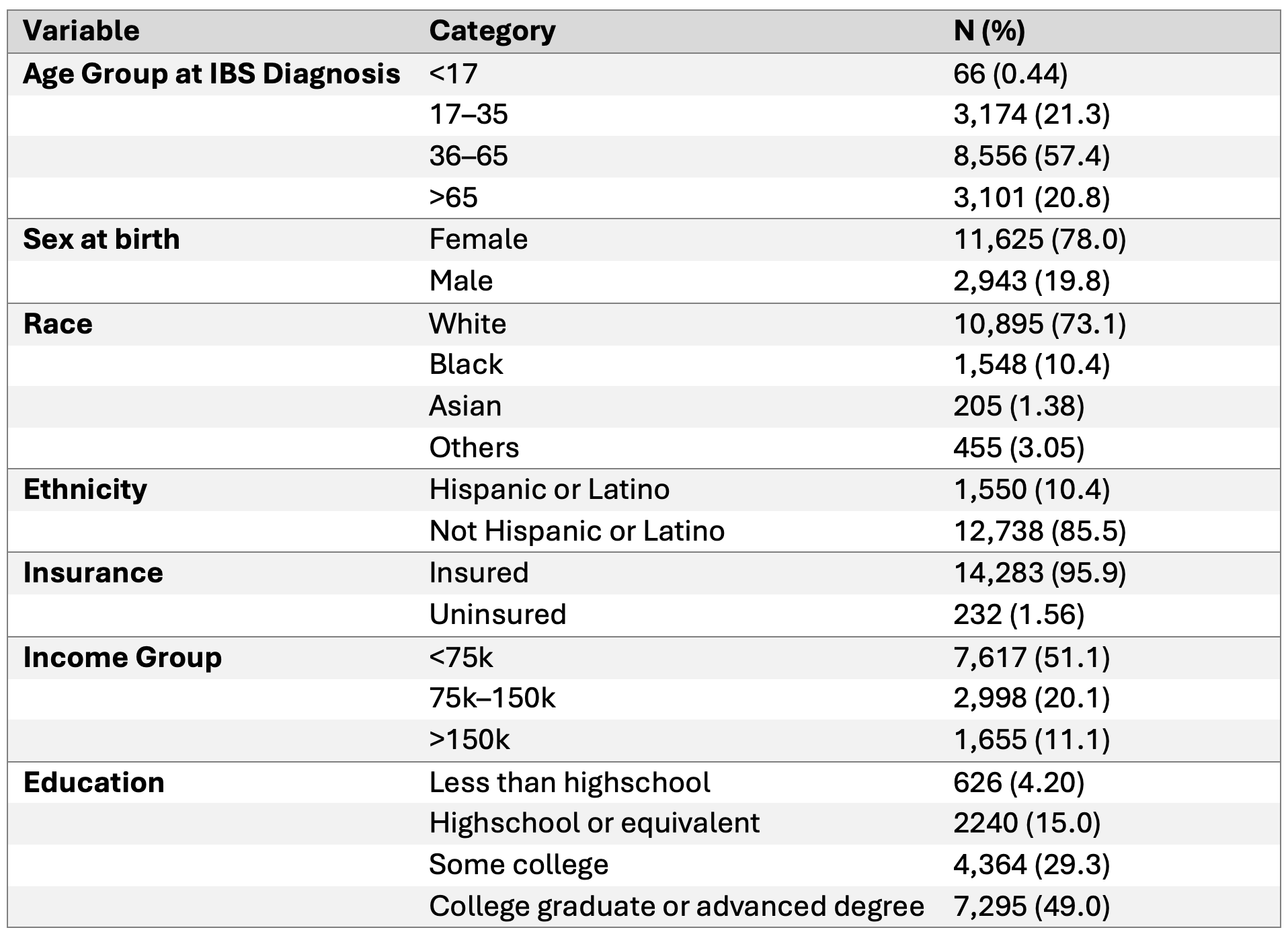
Figure: Figure 1. Demographics of IBS Patients
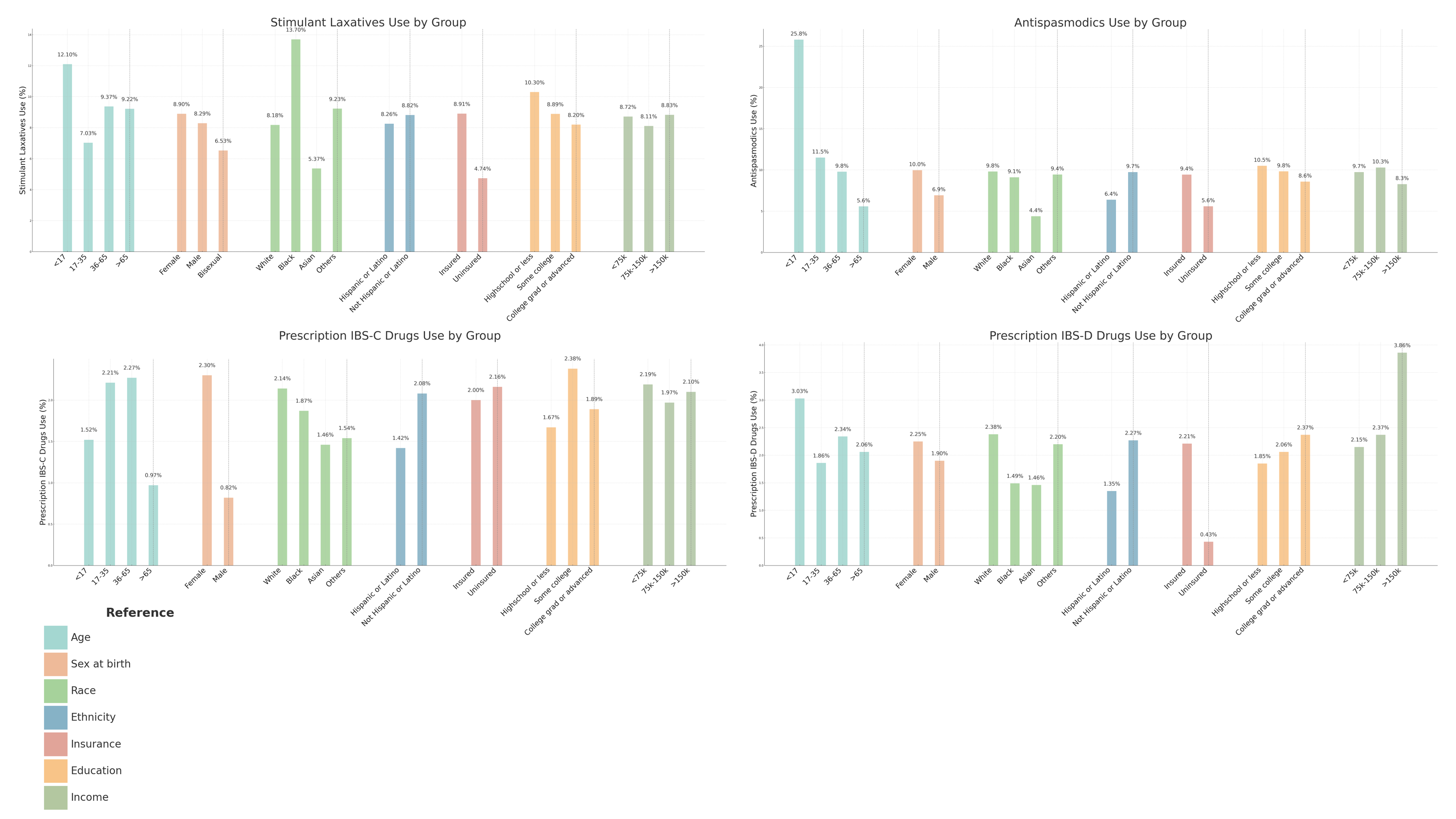
Figure: Figure 1. Stratified Analysis of IBS Medication Use Across Demographic and Socioeconomic Groups
Disclosures:
Anthony Kerbage indicated no relevant financial relationships.
Yueqi Wu indicated no relevant financial relationships.
Madison Simons indicated no relevant financial relationships.
Judy Nee: Fzata – Consultant.
Samita Garg indicated no relevant financial relationships.
Scott Gabbard: Gastrogirl – invited podcast talk.
Anthony Lembo: Allurion – Stock-publicly held company(excluding mutual/index funds). Ardeylx – Consultant. Atmo – Advisory Committee/Board Member. Bristol Myer Squibb – Stock-publicly held company(excluding mutual/index funds). GSK – Consultant. Ironwood – DSMB. J&J – Stock-publicly held company(excluding mutual/index funds). Salix – Consultant. Takeda – Consultant. Vibrant – Consultant.
Anthony Kerbage, MD1, Yueqi Wu, MPH2, Madison Simons, PhD1, Judy Nee, MD3, Samita Garg, MD1, Scott L. Gabbard, MD, FACG4, Anthony Lembo, MD, FACG1. P0781 - Prevalence and Prescription Patterns of IBS Treatments Across Demographic and Socioeconomic Factors, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

