Sunday Poster Session
Category: Functional Bowel Disease
P0780 - Depression and Digestive Health: Gut-Brain Axis Disorders in Hospitalized Patients With Major Depressive Disorder
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- HM
Hezborn Magacha, MD
East Tennessee State University
Johnson City, TN
Presenting Author(s)
Hezborn Magacha, MD1, McKenna Andrews, MD2, Sean Moore, MD3, Adedeji Adenusi, MD4
1East Tennessee State University, Johnson City, TN; 2East Tennessee State University, Kingsport, TN; 3East Tennessee State University Quillen College of Medicine, Johnson City, TN; 4One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY
Introduction: Depression impacts the gastrointestinal health via the gut brain axis (GBA), a bidirectional pathway between the central nervous system and the gastrointestinal system. This study analyzes the association between depression and the gastrointestinal disorders using the National inpatient sample (NIS) database, by emphasizing the role of depression on gastrointestinal comorbidities.
Methods: The study utilized the NIS database 2016- 2020, a national available database to assess the association between depression and the risk for gastrointestinal disorders including the irritable bowel syndrome (IBS), functional diarrhea and idiopathic constipation. Multivariate, logistic regression and the subgroup analyses were conducted to establish this association while accounting for confounders such as age, sex and race.
Results: Among 79,943,129 individuals, 12.3% (n = 9,834,583) were diagnosed with Major Depression (MDD), with higher prevalence in females (6.25 million) than males (3.58 million), and in White individuals (7.62 million) versus other races. The annual MDD diagnosis rate remained fairly stable from 2016–2020 (p < 0.0001). MDD was associated with significantly increased risks of IBS (OR 3.05, p < 0.0001), idiopathic constipation (OR 1.679, 95% CI 1.609–1.751), and functional diarrhea (OR 1.379, 95% CI 1.337–1.422), all p < 0.0001. Among those with MDD, females had lower odds of IBS (OR 0.289, 95% CI 0.288–0.291) and constipation (OR 0.727, 95% CI 0.701–0.754), but slightly higher odds of diarrhea (OR 1.068,95% CI 1.042–1.095) versus males. White individuals had over twice the odds of IBS compared to Native Americans (OR 2.289, 95% CI 2.194–2.388), with elevated odds of constipation (OR 1.249, 95% CI 0.946–1.650) and diarrhea (OR 1.287). Asians had lower odds across all conditions, especially IBS (OR 0.575). Black individuals had slightly lower IBS odds (OR 0.951), but higher odds for constipation (OR 1.452) and diarrhea (OR 1.426). Hispanics had reduced odds of IBS (OR 0.923); associations with constipation and diarrhea were not significant. Compared to those ≥70, younger adults had lower odds of all GI disorders, with increasing odds peaking at ages 40–60.
Discussion: This study demonstrates that depression is an independent and significant risk factor for functional gastrointestinal disorders. This association is notably influenced by demographic factors particularly race, age and sex, highlighting the complex association between mental health and gastrointestinal health.
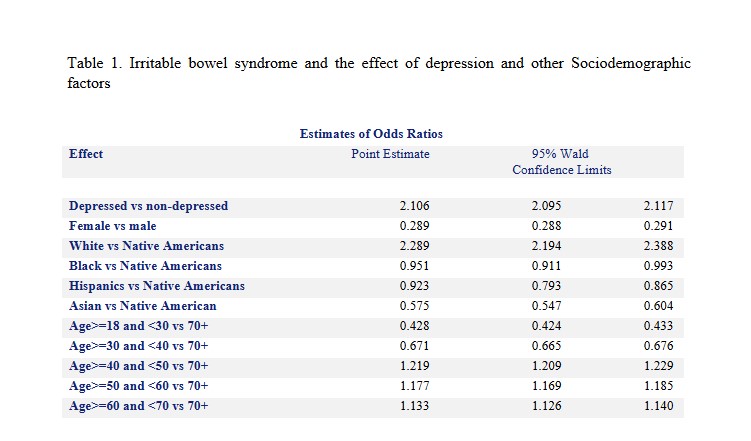
Figure: Irritable bowel syndrome and the effect of depression and other Sociodemographic factors
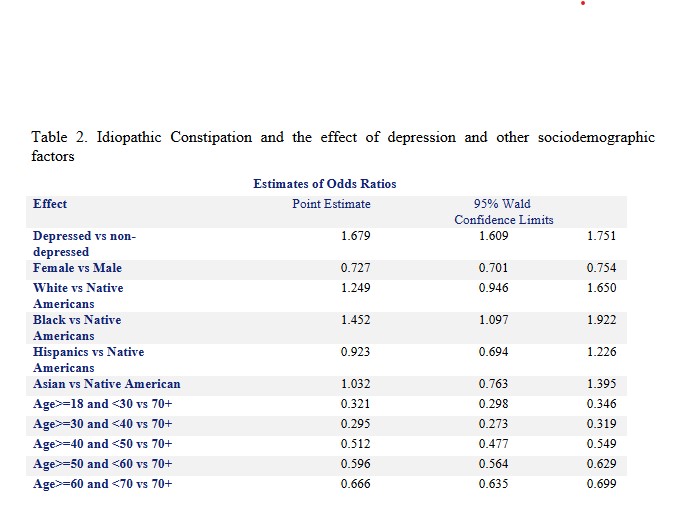
Figure: Idiopathic Constipation and the effect of depression and other sociodemographic factors
Disclosures:
Hezborn Magacha indicated no relevant financial relationships.
McKenna Andrews indicated no relevant financial relationships.
Sean Moore indicated no relevant financial relationships.
Adedeji Adenusi indicated no relevant financial relationships.
Hezborn Magacha, MD1, McKenna Andrews, MD2, Sean Moore, MD3, Adedeji Adenusi, MD4. P0780 - Depression and Digestive Health: Gut-Brain Axis Disorders in Hospitalized Patients With Major Depressive Disorder, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1East Tennessee State University, Johnson City, TN; 2East Tennessee State University, Kingsport, TN; 3East Tennessee State University Quillen College of Medicine, Johnson City, TN; 4One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY
Introduction: Depression impacts the gastrointestinal health via the gut brain axis (GBA), a bidirectional pathway between the central nervous system and the gastrointestinal system. This study analyzes the association between depression and the gastrointestinal disorders using the National inpatient sample (NIS) database, by emphasizing the role of depression on gastrointestinal comorbidities.
Methods: The study utilized the NIS database 2016- 2020, a national available database to assess the association between depression and the risk for gastrointestinal disorders including the irritable bowel syndrome (IBS), functional diarrhea and idiopathic constipation. Multivariate, logistic regression and the subgroup analyses were conducted to establish this association while accounting for confounders such as age, sex and race.
Results: Among 79,943,129 individuals, 12.3% (n = 9,834,583) were diagnosed with Major Depression (MDD), with higher prevalence in females (6.25 million) than males (3.58 million), and in White individuals (7.62 million) versus other races. The annual MDD diagnosis rate remained fairly stable from 2016–2020 (p < 0.0001). MDD was associated with significantly increased risks of IBS (OR 3.05, p < 0.0001), idiopathic constipation (OR 1.679, 95% CI 1.609–1.751), and functional diarrhea (OR 1.379, 95% CI 1.337–1.422), all p < 0.0001. Among those with MDD, females had lower odds of IBS (OR 0.289, 95% CI 0.288–0.291) and constipation (OR 0.727, 95% CI 0.701–0.754), but slightly higher odds of diarrhea (OR 1.068,95% CI 1.042–1.095) versus males. White individuals had over twice the odds of IBS compared to Native Americans (OR 2.289, 95% CI 2.194–2.388), with elevated odds of constipation (OR 1.249, 95% CI 0.946–1.650) and diarrhea (OR 1.287). Asians had lower odds across all conditions, especially IBS (OR 0.575). Black individuals had slightly lower IBS odds (OR 0.951), but higher odds for constipation (OR 1.452) and diarrhea (OR 1.426). Hispanics had reduced odds of IBS (OR 0.923); associations with constipation and diarrhea were not significant. Compared to those ≥70, younger adults had lower odds of all GI disorders, with increasing odds peaking at ages 40–60.
Discussion: This study demonstrates that depression is an independent and significant risk factor for functional gastrointestinal disorders. This association is notably influenced by demographic factors particularly race, age and sex, highlighting the complex association between mental health and gastrointestinal health.
Figure: Irritable bowel syndrome and the effect of depression and other Sociodemographic factors
Figure: Idiopathic Constipation and the effect of depression and other sociodemographic factors
Disclosures:
Hezborn Magacha indicated no relevant financial relationships.
McKenna Andrews indicated no relevant financial relationships.
Sean Moore indicated no relevant financial relationships.
Adedeji Adenusi indicated no relevant financial relationships.
Hezborn Magacha, MD1, McKenna Andrews, MD2, Sean Moore, MD3, Adedeji Adenusi, MD4. P0780 - Depression and Digestive Health: Gut-Brain Axis Disorders in Hospitalized Patients With Major Depressive Disorder, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
