Sunday Poster Session
Category: Esophagus
P0768 - Esophageal Micro-Perforation Causing Neck and Chest Abscess
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Patt Panuncillon, DO
Ochsner Health Clinic Foundation, TX
Presenting Author(s)
Patt Panuncillon, DO1, Ricardo David Espinosa, MD2, Joanna Yuen, DO, MA3, Ian Tobal, DO2, Sameera Shuaibi, MD2, Koshy George, MD2
1Ochsner Health Clinic Foundation, Pearland, TX; 2Ochsner Health Clinic Foundation, New Orleans, LA; 3Ochsner Health Clinic Foundation, Jefferson, LA
Introduction: Esophageal micro-perforation is a rare phenomenon and can be challenging to diagnose. It can be seen in patients with recent device instrumentation, ingestion of foreign objects, various inflammatory processes, or vomiting and retching. These perforations can lead to abscess formation, pneumomediastinum, and potential hemodynamic collapse.
Case Description/
Methods: A 65-year-old female with GERD and recent admission for incision and drainage (I&D) of a right peritonsillar abscess presented with left neck and chest pain with swelling. She was afebrile, but tachycardic with a WBC of 18. CT neck and chest showed a lower anterior left neck abscess measuring 6.4 x 5.0 x 2.0 cm with overlying cellulitis. She was started on IV antibiotics and taken to the OR for I&D. Copious purulence was noted from the esophagus: concerning for a GI source of infection, specifically esophageal perforation. However, additional CT imaging and esophagram did not show perforation. Blood and abscess cultures later grew Corynebacterium. Her diet was advanced further after negative imaging, but her cellulitis worsened and purulent output from her surgical drains increased. Thus, she was made NPO again and both the cellulitis and output improved. The improvement with her NPO status made esophageal upper micro-perforation the leading differential as the source of her infection. She received a PEG tube, as she was going to require prolonged NPO status to allow the perforation to heal and was discharged home with IV antibiotics.
Discussion: Esophageal micro-perforations are rare and can lead to infection with abscess formation. It is reported that almost all upper esophageal perforations are secondary to instrumentation, which can allow esophageal contents to leak into the surrounding tissues. They are challenging to diagnose as they may not show up on traditional imaging. In this case, the combination of multiple cultures growing the same oral flora, recent oropharyngeal manipulation, improvement of abscess output while NPO, and thorough workup to rule out other sources made esophageal micro-perforation the most likely diagnosis, despite negative imaging. This case shows the importance of recognizing esophageal micro-perforation as a source of neck and chest abscesses and emphasizes that negative imaging alone cannot exclude the diagnosis. Appropriate interventions, including I&D, esophageal rest, and antibiotics, are essential for managing this uncommon condition and preventing further complications.
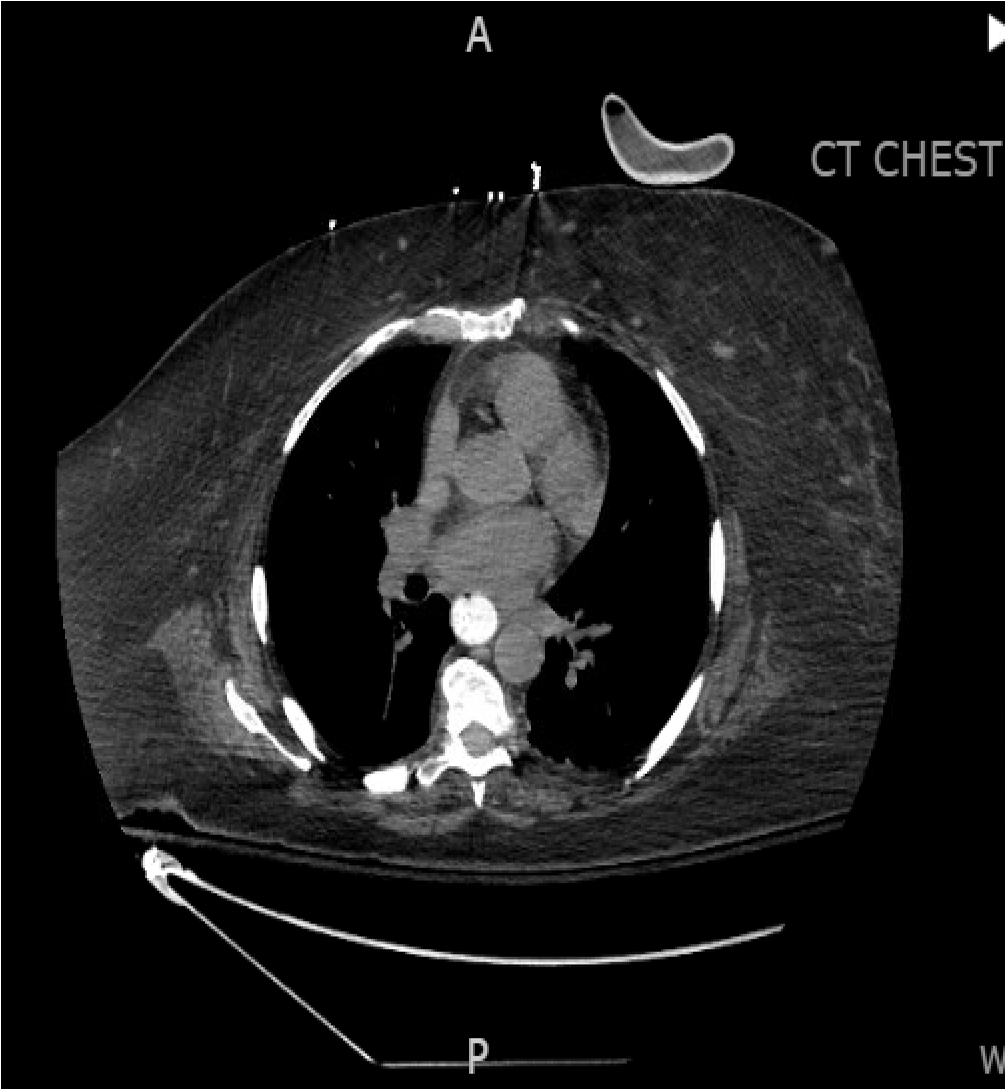
Figure: Figure 1: CT chest without evidence of frank esophageal perforation

Figure: Figure 2: CT neck chest displaying abscess and phlegmon
Disclosures:
Patt Panuncillon indicated no relevant financial relationships.
Ricardo David Espinosa indicated no relevant financial relationships.
Joanna Yuen indicated no relevant financial relationships.
Ian Tobal indicated no relevant financial relationships.
Sameera Shuaibi indicated no relevant financial relationships.
Koshy George indicated no relevant financial relationships.
Patt Panuncillon, DO1, Ricardo David Espinosa, MD2, Joanna Yuen, DO, MA3, Ian Tobal, DO2, Sameera Shuaibi, MD2, Koshy George, MD2. P0768 - Esophageal Micro-Perforation Causing Neck and Chest Abscess, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Ochsner Health Clinic Foundation, Pearland, TX; 2Ochsner Health Clinic Foundation, New Orleans, LA; 3Ochsner Health Clinic Foundation, Jefferson, LA
Introduction: Esophageal micro-perforation is a rare phenomenon and can be challenging to diagnose. It can be seen in patients with recent device instrumentation, ingestion of foreign objects, various inflammatory processes, or vomiting and retching. These perforations can lead to abscess formation, pneumomediastinum, and potential hemodynamic collapse.
Case Description/
Methods: A 65-year-old female with GERD and recent admission for incision and drainage (I&D) of a right peritonsillar abscess presented with left neck and chest pain with swelling. She was afebrile, but tachycardic with a WBC of 18. CT neck and chest showed a lower anterior left neck abscess measuring 6.4 x 5.0 x 2.0 cm with overlying cellulitis. She was started on IV antibiotics and taken to the OR for I&D. Copious purulence was noted from the esophagus: concerning for a GI source of infection, specifically esophageal perforation. However, additional CT imaging and esophagram did not show perforation. Blood and abscess cultures later grew Corynebacterium. Her diet was advanced further after negative imaging, but her cellulitis worsened and purulent output from her surgical drains increased. Thus, she was made NPO again and both the cellulitis and output improved. The improvement with her NPO status made esophageal upper micro-perforation the leading differential as the source of her infection. She received a PEG tube, as she was going to require prolonged NPO status to allow the perforation to heal and was discharged home with IV antibiotics.
Discussion: Esophageal micro-perforations are rare and can lead to infection with abscess formation. It is reported that almost all upper esophageal perforations are secondary to instrumentation, which can allow esophageal contents to leak into the surrounding tissues. They are challenging to diagnose as they may not show up on traditional imaging. In this case, the combination of multiple cultures growing the same oral flora, recent oropharyngeal manipulation, improvement of abscess output while NPO, and thorough workup to rule out other sources made esophageal micro-perforation the most likely diagnosis, despite negative imaging. This case shows the importance of recognizing esophageal micro-perforation as a source of neck and chest abscesses and emphasizes that negative imaging alone cannot exclude the diagnosis. Appropriate interventions, including I&D, esophageal rest, and antibiotics, are essential for managing this uncommon condition and preventing further complications.
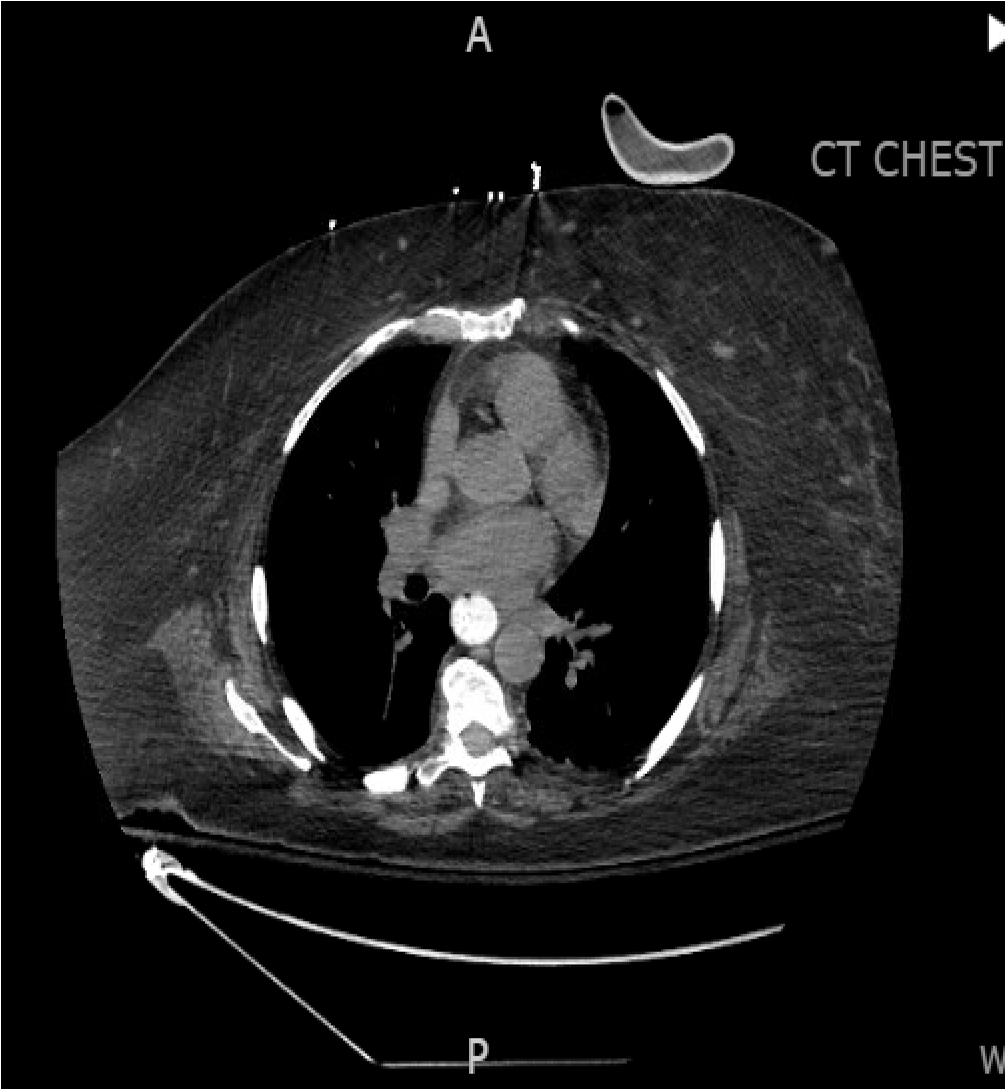
Figure: Figure 1: CT chest without evidence of frank esophageal perforation

Figure: Figure 2: CT neck chest displaying abscess and phlegmon
Disclosures:
Patt Panuncillon indicated no relevant financial relationships.
Ricardo David Espinosa indicated no relevant financial relationships.
Joanna Yuen indicated no relevant financial relationships.
Ian Tobal indicated no relevant financial relationships.
Sameera Shuaibi indicated no relevant financial relationships.
Koshy George indicated no relevant financial relationships.
Patt Panuncillon, DO1, Ricardo David Espinosa, MD2, Joanna Yuen, DO, MA3, Ian Tobal, DO2, Sameera Shuaibi, MD2, Koshy George, MD2. P0768 - Esophageal Micro-Perforation Causing Neck and Chest Abscess, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
