Sunday Poster Session
Category: General Endoscopy
P0847 - Los Angeles Grade B Esophagitis as Actionable GERD - Does the Subspecialist Matter?
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Rama Hussein, DO (she/her/hers)
Mount Sinai West, Icahn School of Medicine at Mount Sinai
New York City, NY
Presenting Author(s)
Rama Hussein, DO1, Soha Noorani, DO2, Yuying Luo, MD3, Daniela Jodorkovsky, MD4
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York City, NY; 2Mount Sinai Morningside, Icahn School of Medicine at Mount Sinai, New York, NY; 3Mount Sinai West & Morningside, New York, NY; 4Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: According to the updated Lyon Consensus 2.0, Los Angeles (LA) grade B esophagitis is now considered a gastroesophageal reflux disease (GERD) equivalent. This change represents an important update in clinical guidance, but may have variable adherence and applicability by gastroenterologists depending on subspecialty. We aimed to evaluate if the management of LA grade B esophagitis was dependent on provider subspecialty.
Methods: A retrospective comparative analysis of patients with LA grade B esophagitis on esophagogastroduodenoscopy (EGD) between October 2022 and September 2023 at two hospital sites within one health system was performed. Outcomes included differences in patient demographics, escalation of medical management and referral for quantitative reflux testing, repeat endoscopy and fundoplication following detection of LA grade B between the two sites varying in subspecialist access. Escalation of medical management was defined as initiation of antisecretory therapy, or increase in dose, potency, or frequency of acid suppression medication.
Results: 66% of the providers at Hospital A are considered esophageal or motility specialists while none of the gastroenterologists at Hospital B are within this subspecialty. Patient demographic variables did not differ between the two sites. 15.6% of patients at Hospital A vs 2.5% at Hospital B were referred to quantitative reflux testing following LA grade B esophagitis detection (p-value=0.003). 52.2% of patients at Hospital A received medical management escalation compared to 55.7% of patients at Hospital B (p-value=0.65). 17.8% of patients at Hospital A were referred for repeat EGD compared to 12.7% at Hospital B (p-value=0.39). Of the 17 patients who underwent repeat EGD, 80% showed improvement in esophagitis grade at Hospital A compared to 57% showed improvement in Hospital B (p=0.36). 11.1% of patients at Hospital A were referred for fundoplication while 0% were referred at Hospital B (p-value=0.002).
Discussion: Patients with LA grade B esophagitis managed by esophagus or motility specialists were more likely to be referred for reflux testing or fundoplication compared to general gastroenterologists. However, there was no significant difference in plan for medical escalation of LA grade B esophagitis that was dependent on provider subspecialty. Increased provider education regarding recent inclusion of LA grade B esophagitis as conclusive GERD is important to provide uniform and personalized management for patients with esophagitis.
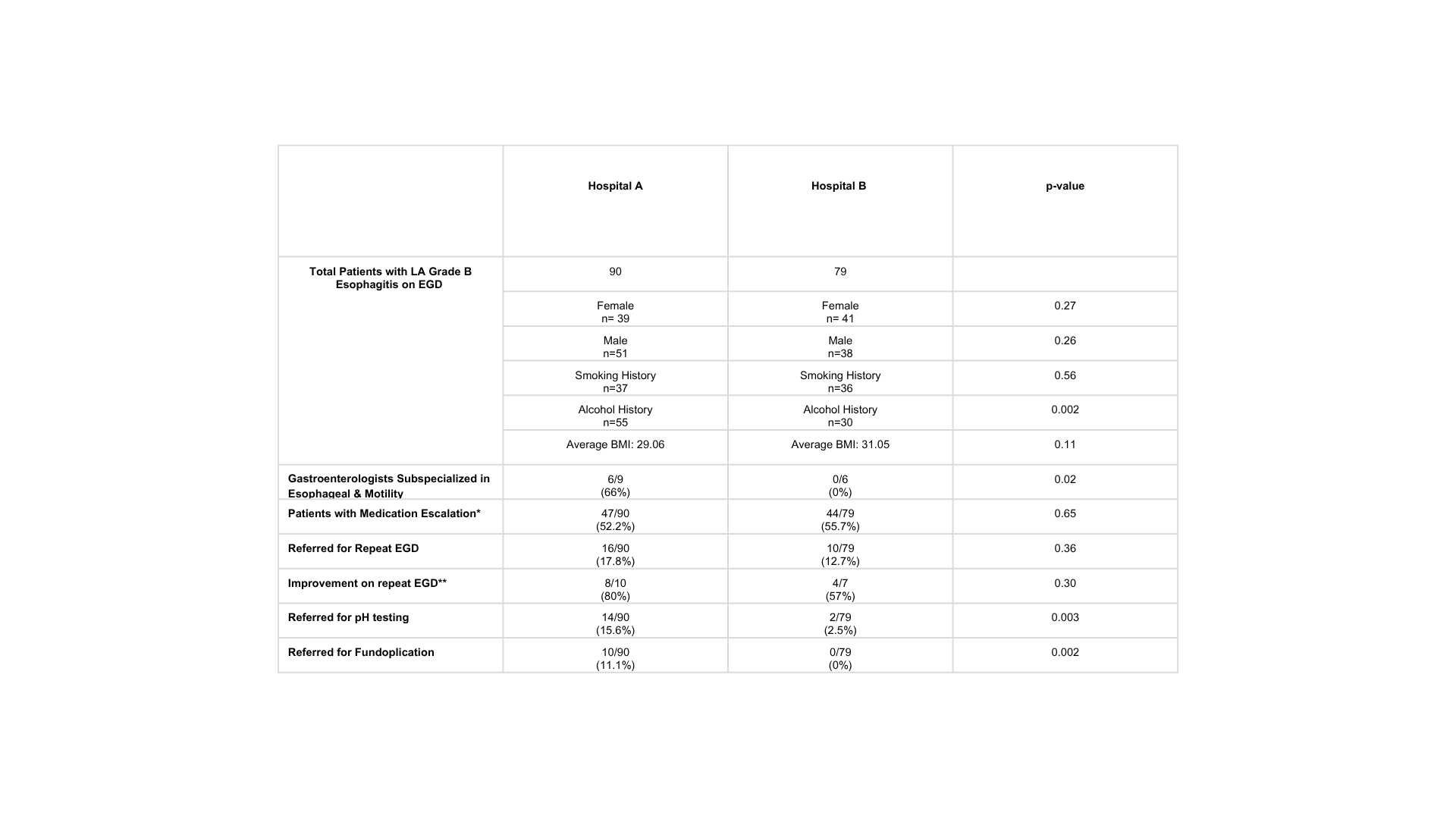
Figure: Table 1. Evaluation of escalation of medical care following initial findings of LA grade B esophagitis on EGD at two hospital sites with varying Gastroenterology subspecialists.
*Medication escalation defined as: initiating antisecretory medication, increasing potency of antisecretory medication, switching antisecretory medication class, or increasing frequency
*Improvement on repeat EGD is defined as complete resolution of esophagitis or findings of LA grade A esophagitis.
Disclosures:
Rama Hussein indicated no relevant financial relationships.
Soha Noorani indicated no relevant financial relationships.
Yuying Luo: Ardelyx – Grant/Research Support.
Daniela Jodorkovsky indicated no relevant financial relationships.
Rama Hussein, DO1, Soha Noorani, DO2, Yuying Luo, MD3, Daniela Jodorkovsky, MD4. P0847 - Los Angeles Grade B Esophagitis as Actionable GERD - Does the Subspecialist Matter?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York City, NY; 2Mount Sinai Morningside, Icahn School of Medicine at Mount Sinai, New York, NY; 3Mount Sinai West & Morningside, New York, NY; 4Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: According to the updated Lyon Consensus 2.0, Los Angeles (LA) grade B esophagitis is now considered a gastroesophageal reflux disease (GERD) equivalent. This change represents an important update in clinical guidance, but may have variable adherence and applicability by gastroenterologists depending on subspecialty. We aimed to evaluate if the management of LA grade B esophagitis was dependent on provider subspecialty.
Methods: A retrospective comparative analysis of patients with LA grade B esophagitis on esophagogastroduodenoscopy (EGD) between October 2022 and September 2023 at two hospital sites within one health system was performed. Outcomes included differences in patient demographics, escalation of medical management and referral for quantitative reflux testing, repeat endoscopy and fundoplication following detection of LA grade B between the two sites varying in subspecialist access. Escalation of medical management was defined as initiation of antisecretory therapy, or increase in dose, potency, or frequency of acid suppression medication.
Results: 66% of the providers at Hospital A are considered esophageal or motility specialists while none of the gastroenterologists at Hospital B are within this subspecialty. Patient demographic variables did not differ between the two sites. 15.6% of patients at Hospital A vs 2.5% at Hospital B were referred to quantitative reflux testing following LA grade B esophagitis detection (p-value=0.003). 52.2% of patients at Hospital A received medical management escalation compared to 55.7% of patients at Hospital B (p-value=0.65). 17.8% of patients at Hospital A were referred for repeat EGD compared to 12.7% at Hospital B (p-value=0.39). Of the 17 patients who underwent repeat EGD, 80% showed improvement in esophagitis grade at Hospital A compared to 57% showed improvement in Hospital B (p=0.36). 11.1% of patients at Hospital A were referred for fundoplication while 0% were referred at Hospital B (p-value=0.002).
Discussion: Patients with LA grade B esophagitis managed by esophagus or motility specialists were more likely to be referred for reflux testing or fundoplication compared to general gastroenterologists. However, there was no significant difference in plan for medical escalation of LA grade B esophagitis that was dependent on provider subspecialty. Increased provider education regarding recent inclusion of LA grade B esophagitis as conclusive GERD is important to provide uniform and personalized management for patients with esophagitis.
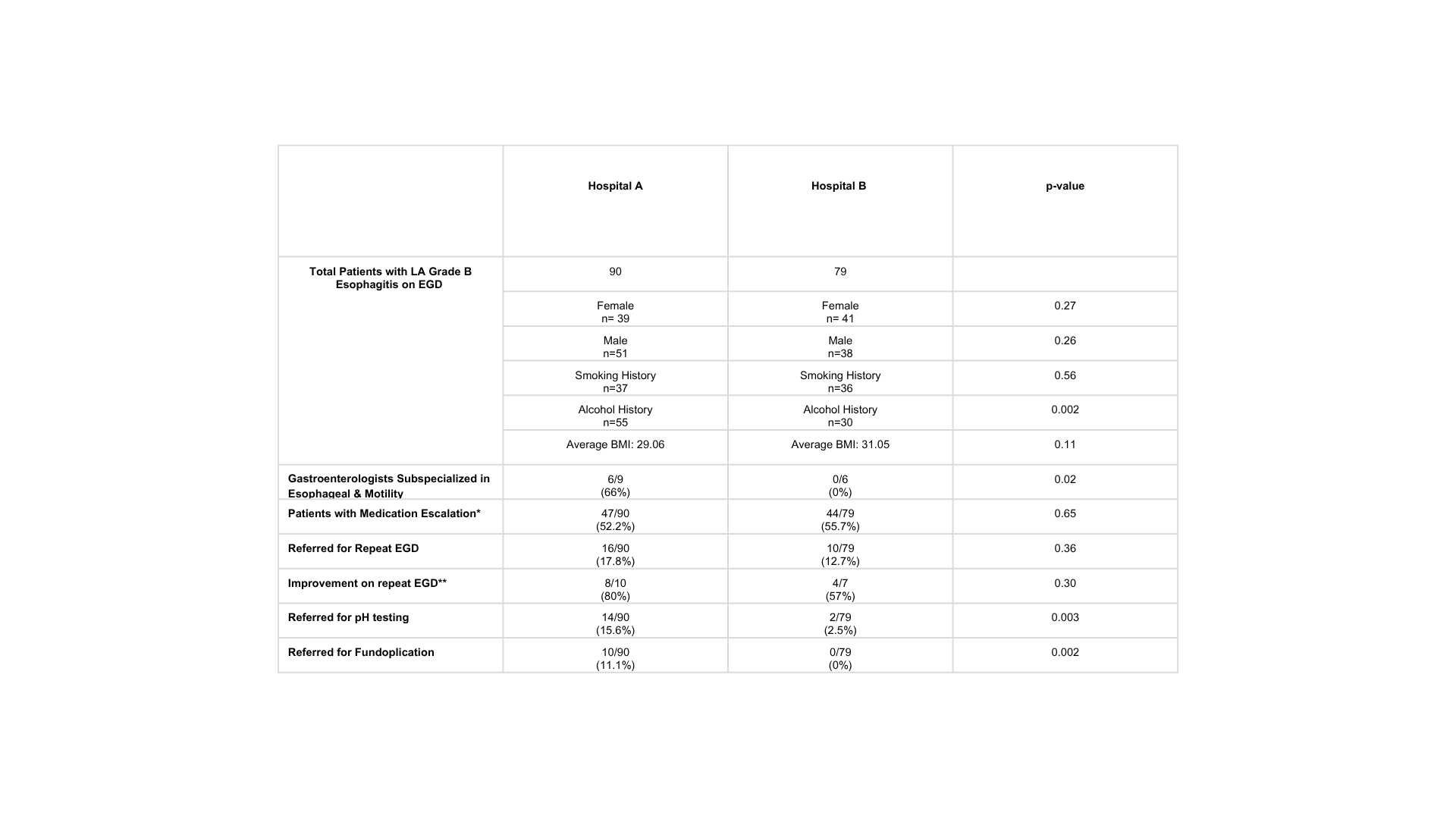
Figure: Table 1. Evaluation of escalation of medical care following initial findings of LA grade B esophagitis on EGD at two hospital sites with varying Gastroenterology subspecialists.
*Medication escalation defined as: initiating antisecretory medication, increasing potency of antisecretory medication, switching antisecretory medication class, or increasing frequency
*Improvement on repeat EGD is defined as complete resolution of esophagitis or findings of LA grade A esophagitis.
Disclosures:
Rama Hussein indicated no relevant financial relationships.
Soha Noorani indicated no relevant financial relationships.
Yuying Luo: Ardelyx – Grant/Research Support.
Daniela Jodorkovsky indicated no relevant financial relationships.
Rama Hussein, DO1, Soha Noorani, DO2, Yuying Luo, MD3, Daniela Jodorkovsky, MD4. P0847 - Los Angeles Grade B Esophagitis as Actionable GERD - Does the Subspecialist Matter?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
