Sunday Poster Session
Category: GI Bleeding
P0919 - Lower In-Hospital Mortality in Long-Term Anticoagulated Patients With GI Bleeding: A National Inpatient Sample Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Abdulmoiz Aljafari, MD
Hamilton Medical Center
Dalton, GA
Presenting Author(s)
Abdulmoiz Aljafari, MD1, Abdulkader Shaar, MD2
1Hamilton Medical Center, Dalton, GA; 2University of Miami, Miami, FL
Introduction: Gastrointestinal (GI) bleeding is a frequent emergency with a major clinical and economic burden. With rising long-term anticoagulant (LTA) use due to aging and expanded indications, more GI bleeds occur in anticoagulated patients. Whether pre-existing anticoagulation worsens or improves outcomes remains uncertain, with mixed findings across studies. We evaluated this relationship using a large national inpatient dataset.
Methods: We conducted a retrospective cohort study using the 2020 National Inpatient Sample (NIS) to analyze adult patients (≥18 years) admitted with a principal diagnosis of gastrointestinal (GI) bleeding. ICD-10-CM codes identified patients with upper or lower GI bleeds and long-term anticoagulant use. Survey weights provided by the NIS generated nationally representative estimates. Multivariable logistic regression was employed to adjust for potential confounders, including patient characteristics, Charlson Comorbidity Index, complications, and hospital characteristics. Analyses were performed using STATA 14.2, with a significance threshold of p< 0.05.
Results: A total of 254,305 patients were identified with GI bleeding, 35,815 (14%) of whom were on long-term anticoagulation (LTA). After adjusting for potential confounders and complications, LTA patients had a 52.5% lower mortality rate. Length of stay decreased by 0.32 days, and total hospital charges were reduced by a mean of $6,459 (p< 0.001). Patients using LTA were 24.7% and 49.8% less likely to develop hypovolemia/shock and respiratory failure, respectively (p< 0.001). However, the incidence of acute renal disease (31.9%), the utilization of endoscopic therapy (39.3%), and the administration of blood transfusions (14.2%) increased significantly (p< 0.001) (Table 1).
Discussion: This study challenges traditional views and supports re-evaluation of anticoagulation in GI bleeding. In our analysis, LTA patients had a 52.5% lower in-hospital mortality risk despite requiring more transfusions and procedures. This aligns with studies suggesting anticoagulation may not worsen—and may even improve—GI bleed outcomes. This may be linked to the fact that LTA patients are often managed more proactively, with closer monitoring, early hospitalization, and multidisciplinary care. These findings could influence risk-benefit decisions regarding anticoagulant management in patients at risk for GI bleeding.
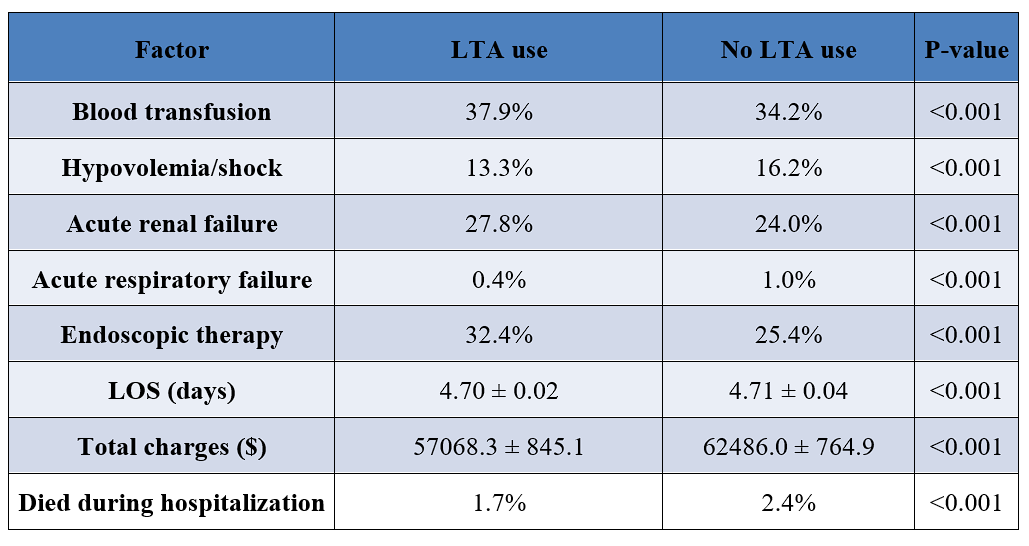
Figure: Table 1. Clinical outcomes and resource utilization for LTA and non-LTA use in patients with GI bleeding.
Disclosures:
Abdulmoiz Aljafari indicated no relevant financial relationships.
Abdulkader Shaar indicated no relevant financial relationships.
Abdulmoiz Aljafari, MD1, Abdulkader Shaar, MD2. P0919 - Lower In-Hospital Mortality in Long-Term Anticoagulated Patients With GI Bleeding: A National Inpatient Sample Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Hamilton Medical Center, Dalton, GA; 2University of Miami, Miami, FL
Introduction: Gastrointestinal (GI) bleeding is a frequent emergency with a major clinical and economic burden. With rising long-term anticoagulant (LTA) use due to aging and expanded indications, more GI bleeds occur in anticoagulated patients. Whether pre-existing anticoagulation worsens or improves outcomes remains uncertain, with mixed findings across studies. We evaluated this relationship using a large national inpatient dataset.
Methods: We conducted a retrospective cohort study using the 2020 National Inpatient Sample (NIS) to analyze adult patients (≥18 years) admitted with a principal diagnosis of gastrointestinal (GI) bleeding. ICD-10-CM codes identified patients with upper or lower GI bleeds and long-term anticoagulant use. Survey weights provided by the NIS generated nationally representative estimates. Multivariable logistic regression was employed to adjust for potential confounders, including patient characteristics, Charlson Comorbidity Index, complications, and hospital characteristics. Analyses were performed using STATA 14.2, with a significance threshold of p< 0.05.
Results: A total of 254,305 patients were identified with GI bleeding, 35,815 (14%) of whom were on long-term anticoagulation (LTA). After adjusting for potential confounders and complications, LTA patients had a 52.5% lower mortality rate. Length of stay decreased by 0.32 days, and total hospital charges were reduced by a mean of $6,459 (p< 0.001). Patients using LTA were 24.7% and 49.8% less likely to develop hypovolemia/shock and respiratory failure, respectively (p< 0.001). However, the incidence of acute renal disease (31.9%), the utilization of endoscopic therapy (39.3%), and the administration of blood transfusions (14.2%) increased significantly (p< 0.001) (Table 1).
Discussion: This study challenges traditional views and supports re-evaluation of anticoagulation in GI bleeding. In our analysis, LTA patients had a 52.5% lower in-hospital mortality risk despite requiring more transfusions and procedures. This aligns with studies suggesting anticoagulation may not worsen—and may even improve—GI bleed outcomes. This may be linked to the fact that LTA patients are often managed more proactively, with closer monitoring, early hospitalization, and multidisciplinary care. These findings could influence risk-benefit decisions regarding anticoagulant management in patients at risk for GI bleeding.
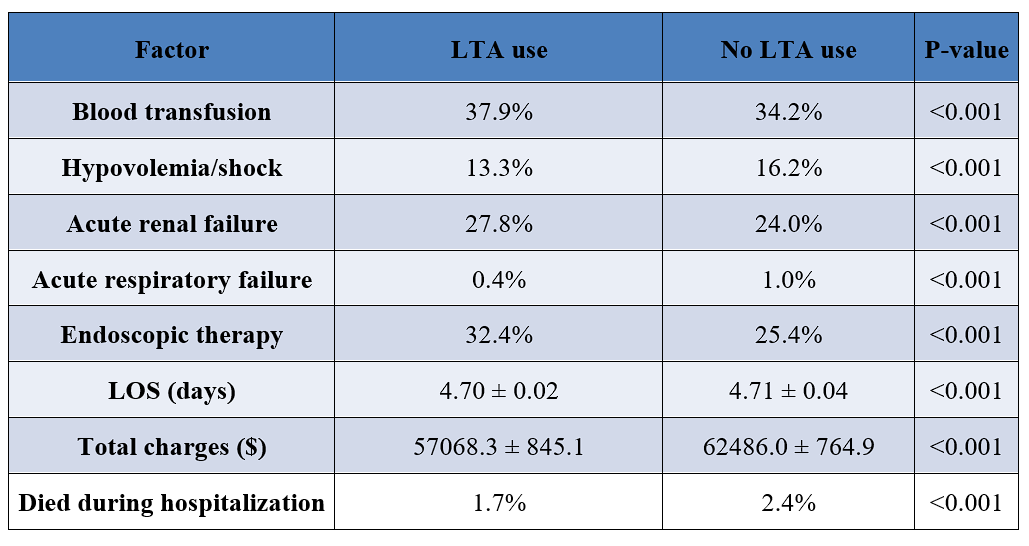
Figure: Table 1. Clinical outcomes and resource utilization for LTA and non-LTA use in patients with GI bleeding.
Disclosures:
Abdulmoiz Aljafari indicated no relevant financial relationships.
Abdulkader Shaar indicated no relevant financial relationships.
Abdulmoiz Aljafari, MD1, Abdulkader Shaar, MD2. P0919 - Lower In-Hospital Mortality in Long-Term Anticoagulated Patients With GI Bleeding: A National Inpatient Sample Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
