Sunday Poster Session
Category: General Endoscopy
P0902 - Systemic Amyloidosis With an Unusual Presentation as a Localized Jejunal Ulcer
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Hamza Akhtar, MD (he/him/his)
Rochester General Hospital
Rochester, NY
Presenting Author(s)
Hamza Akhtar, MD1, Aleena Khan, MD1, Prajjwol D. Bhatta, MD1, Sushrut Ingawale, MD, DNB, MBBS2, Joel E. McFarland, MD1
1Rochester General Hospital, Rochester, NY; 2Quinnipiac University - Frank H Netter MD School of Medicine, Bridgeport, CT
Introduction: Systemic amyloidosis is characterized by the deposition of misfolded extracellular protein fibrils in various organs. The annual incidence of AL amyloidosis is approximately 9.7-14 cases per 1 million-person years. Localized jejunal involvement is a rather rare manifestation of the gastrointestinal manifestations of systemic amyloidosis.
Case Description/
Methods: A 69-year-old female with PMHx of gastric bypass, prior tobacco use and hypertension who had been suffering with malaise, 40-pound weight loss, nausea and solid dysphagia x 3 months and presented to the ED with hypotension. Initial labs showed normocytic anemia and mild AKI. CT scan of abdomen showed type III paraoesophageal hiatal hernia. EGD demonstrated a punched-out ulceration ~ 5 mm in size and multiple biopsies were sent. She was discharged with recommendations for outpatient surgical repair and prescribed a PPI and sucralfate.
Biopsy results unexpectedly came back positive for AL type amyloidosis with congo red staining and BM biopsy revealed 15% plasma cell population. Plans for surgical hernia repair were canceled. Cardiology referral revealed LVH + LA enlargement and elevated proBNP and she was diagnosed with diastolic HF. PET scan showed increased uptake in the tongue, likely due to macroglossia. She continued to have decreased GFR consistent with stage IIIb CKD. Patient was started on chemotherapy with Dara-CyborD. 2 months after her initial presentation, she developed acute watery diarrhea for 2 days, became hypotensive and was admitted to the ICU with septic shock secondary to E. coli bacteremia likely due to translocation. Patient was discharged in stable condition after treatment with IV antibiotics. She is currently doing well and has resumed her chemotherapy regimen cycles.
Discussion: Ours was a case of a localized jejunal ulcer as the first manifestation of systemic amyloidosis with cardiac, renal and GI involvement. While Cowen et al estimates that GI involvement is seen in 3-8% of amyloidosis patients, jejunal involvement remains exceptionally rare with only a few documented cases in literature. We also hypothesized that her large hiatal hernia may have been the result of amyloid fibril deposition in the smooth muscle of the gastric wall leading to structural weakening. Our case also shows the benefit of collecting biopsies from multiple GI sites as jejunal biopsy enabled us to have an earlier diagnosis of amyloidosis and start curative treatment timely.
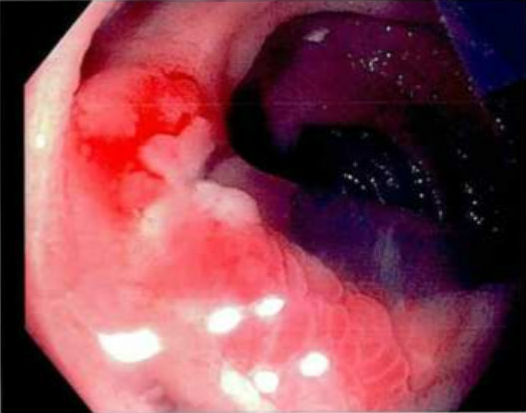
Figure: Punched out 5 mm Jejunal ulcer
Disclosures:
Hamza Akhtar indicated no relevant financial relationships.
Aleena Khan indicated no relevant financial relationships.
Prajjwol Bhatta indicated no relevant financial relationships.
Sushrut Ingawale indicated no relevant financial relationships.
Joel McFarland indicated no relevant financial relationships.
Hamza Akhtar, MD1, Aleena Khan, MD1, Prajjwol D. Bhatta, MD1, Sushrut Ingawale, MD, DNB, MBBS2, Joel E. McFarland, MD1. P0902 - Systemic Amyloidosis With an Unusual Presentation as a Localized Jejunal Ulcer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rochester General Hospital, Rochester, NY; 2Quinnipiac University - Frank H Netter MD School of Medicine, Bridgeport, CT
Introduction: Systemic amyloidosis is characterized by the deposition of misfolded extracellular protein fibrils in various organs. The annual incidence of AL amyloidosis is approximately 9.7-14 cases per 1 million-person years. Localized jejunal involvement is a rather rare manifestation of the gastrointestinal manifestations of systemic amyloidosis.
Case Description/
Methods: A 69-year-old female with PMHx of gastric bypass, prior tobacco use and hypertension who had been suffering with malaise, 40-pound weight loss, nausea and solid dysphagia x 3 months and presented to the ED with hypotension. Initial labs showed normocytic anemia and mild AKI. CT scan of abdomen showed type III paraoesophageal hiatal hernia. EGD demonstrated a punched-out ulceration ~ 5 mm in size and multiple biopsies were sent. She was discharged with recommendations for outpatient surgical repair and prescribed a PPI and sucralfate.
Biopsy results unexpectedly came back positive for AL type amyloidosis with congo red staining and BM biopsy revealed 15% plasma cell population. Plans for surgical hernia repair were canceled. Cardiology referral revealed LVH + LA enlargement and elevated proBNP and she was diagnosed with diastolic HF. PET scan showed increased uptake in the tongue, likely due to macroglossia. She continued to have decreased GFR consistent with stage IIIb CKD. Patient was started on chemotherapy with Dara-CyborD. 2 months after her initial presentation, she developed acute watery diarrhea for 2 days, became hypotensive and was admitted to the ICU with septic shock secondary to E. coli bacteremia likely due to translocation. Patient was discharged in stable condition after treatment with IV antibiotics. She is currently doing well and has resumed her chemotherapy regimen cycles.
Discussion: Ours was a case of a localized jejunal ulcer as the first manifestation of systemic amyloidosis with cardiac, renal and GI involvement. While Cowen et al estimates that GI involvement is seen in 3-8% of amyloidosis patients, jejunal involvement remains exceptionally rare with only a few documented cases in literature. We also hypothesized that her large hiatal hernia may have been the result of amyloid fibril deposition in the smooth muscle of the gastric wall leading to structural weakening. Our case also shows the benefit of collecting biopsies from multiple GI sites as jejunal biopsy enabled us to have an earlier diagnosis of amyloidosis and start curative treatment timely.
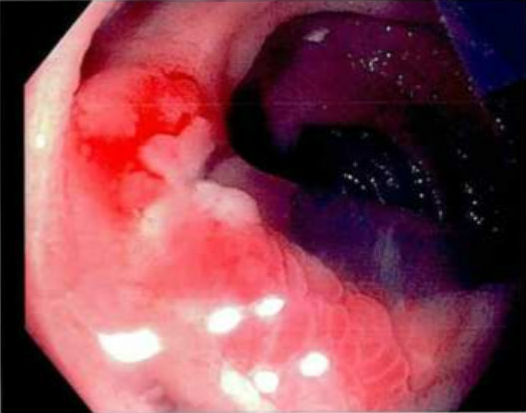
Figure: Punched out 5 mm Jejunal ulcer
Disclosures:
Hamza Akhtar indicated no relevant financial relationships.
Aleena Khan indicated no relevant financial relationships.
Prajjwol Bhatta indicated no relevant financial relationships.
Sushrut Ingawale indicated no relevant financial relationships.
Joel McFarland indicated no relevant financial relationships.
Hamza Akhtar, MD1, Aleena Khan, MD1, Prajjwol D. Bhatta, MD1, Sushrut Ingawale, MD, DNB, MBBS2, Joel E. McFarland, MD1. P0902 - Systemic Amyloidosis With an Unusual Presentation as a Localized Jejunal Ulcer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
