Sunday Poster Session
Category: General Endoscopy
P0901 - Lemmel Syndrome Unveiled: A Rare Case of Periampullary Diverticulum-Induced Biliary Obstruction
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Guneet Sidhu, MD
University of North Dakota, School of Medicine and Health Sciences
Fargo, ND
Presenting Author(s)
Guneet Sidhu, MD1, Ross Meidinger, MD2
1University of North Dakota, School of Medicine and Health Sciences, Fargo, ND; 2Sanford Health, Fargo, ND
Introduction: Lemmel syndrome is an uncommon cause of obstructive jaundice, characterized by extrinsic compression of the common bile duct (CBD) by a periampullary duodenal diverticulum in the absence of choledocholithiasis or neoplasia. Due to its rarity and nonspecific clinical presentation, it is often misdiagnosed, leading to delays in appropriate management. Endoscopic retrograde cholangiopancreatography (ERCP) serves both diagnostic and therapeutic roles.
Case Description/
Methods: 69Y F with history for supraventricular tachycardia and basal ganglia stroke presented with acute epigastric pain radiating to the right upper quadrant, accompanied by nausea and non-hemorrhagic vomiting. Laboratory investigations revealed elevated lipase ( >3,000 U/L), amylase ( >2,000 U/L), total bilirubin (1.5 mg/dL), alkaline phosphatase (156 U/L), AST (607 U/L), and ALT (516 U/L), along with leukocytosis and acute kidney injury. Abdominal CT scan indicated acute pancreatitis, gallbladder wall thickening, and a duodenal diverticulum. Ultrasound showed a mildly dilated CBD without cholelithiasis. MRCP demonstrated mild intra- and extrahepatic biliary dilatation and a large periampullary diverticulum, raising suspicion for Lemmel syndrome. During ERCP, the major papilla was located at the edge of the diverticulum with redundant duodenal mucosa. Pancreatogram revealed a dilated pancreatic duct; a 5 Fr x 9 cm pancreatic stent was placed. Initial attempts at biliary cannulation were unsuccessful, necessitating EUS-guided cholangiography via a 22-gauge FNA needle, which showed a prominent bile duct with distal kinking likely due to the diverticulum. Subsequent needle-knife papillotomy allowed successful biliary access, and a 10 mm x 6 cm fully covered metal biliary stent was deployed.
Discussion: This case underscores the diagnostic challenge posed by Lemmel syndrome, a rare entity resulting from periampullary diverticulum-induced biliary obstruction. The patient's presentation with pancreatitis and biliary obstruction without evident choledocholithiasis highlights the importance of considering Lemmel syndrome in differential diagnoses. Advanced imaging techniques, particularly MRCP and EUS, were instrumental in identifying the periampullary diverticulum and assessing its impact on biliary anatomy. The therapeutic approach involved a combination of ERCP and EUS-guided interventions, demonstrating the utility of a multidisciplinary endoscopic strategy in managing complex biliary obstructions.
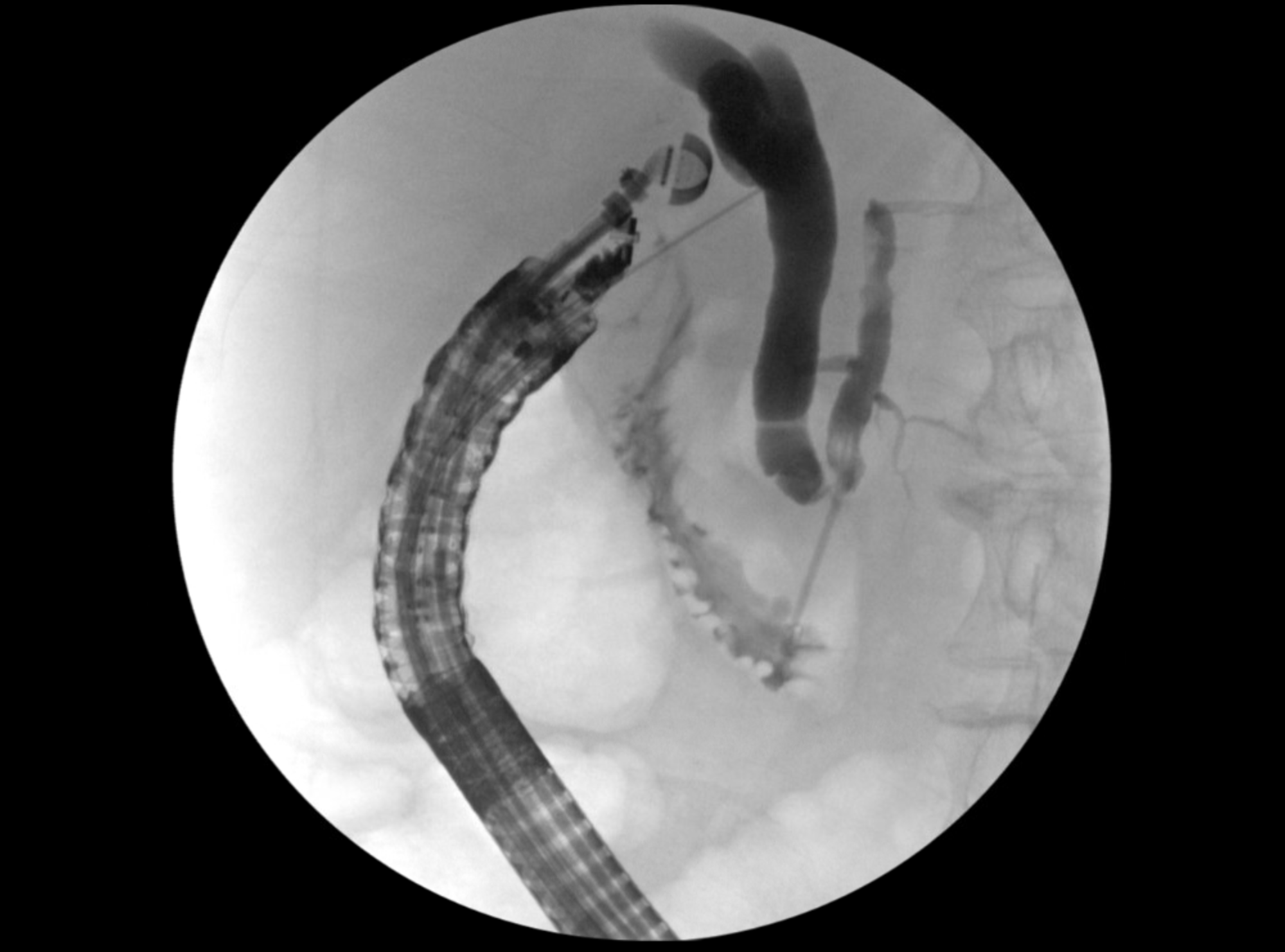
Figure: A 22-gauge FNA needle was punctured through the duodenal bulb wall into the bile duct and contrast was injected through the FNA needle to perform a cholangiogram. The distal 8 mm of CBD just above the ampulla appeared to be kinked with poor drainage into the duodenum, likely related to traction from the periampullary diverticulum

Figure: A extraction balloon was advanced into the bile duct and balloon sweeps yielded no stones or sludge
Disclosures:
Guneet Sidhu indicated no relevant financial relationships.
Ross Meidinger indicated no relevant financial relationships.
Guneet Sidhu, MD1, Ross Meidinger, MD2. P0901 - Lemmel Syndrome Unveiled: A Rare Case of Periampullary Diverticulum-Induced Biliary Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of North Dakota, School of Medicine and Health Sciences, Fargo, ND; 2Sanford Health, Fargo, ND
Introduction: Lemmel syndrome is an uncommon cause of obstructive jaundice, characterized by extrinsic compression of the common bile duct (CBD) by a periampullary duodenal diverticulum in the absence of choledocholithiasis or neoplasia. Due to its rarity and nonspecific clinical presentation, it is often misdiagnosed, leading to delays in appropriate management. Endoscopic retrograde cholangiopancreatography (ERCP) serves both diagnostic and therapeutic roles.
Case Description/
Methods: 69Y F with history for supraventricular tachycardia and basal ganglia stroke presented with acute epigastric pain radiating to the right upper quadrant, accompanied by nausea and non-hemorrhagic vomiting. Laboratory investigations revealed elevated lipase ( >3,000 U/L), amylase ( >2,000 U/L), total bilirubin (1.5 mg/dL), alkaline phosphatase (156 U/L), AST (607 U/L), and ALT (516 U/L), along with leukocytosis and acute kidney injury. Abdominal CT scan indicated acute pancreatitis, gallbladder wall thickening, and a duodenal diverticulum. Ultrasound showed a mildly dilated CBD without cholelithiasis. MRCP demonstrated mild intra- and extrahepatic biliary dilatation and a large periampullary diverticulum, raising suspicion for Lemmel syndrome. During ERCP, the major papilla was located at the edge of the diverticulum with redundant duodenal mucosa. Pancreatogram revealed a dilated pancreatic duct; a 5 Fr x 9 cm pancreatic stent was placed. Initial attempts at biliary cannulation were unsuccessful, necessitating EUS-guided cholangiography via a 22-gauge FNA needle, which showed a prominent bile duct with distal kinking likely due to the diverticulum. Subsequent needle-knife papillotomy allowed successful biliary access, and a 10 mm x 6 cm fully covered metal biliary stent was deployed.
Discussion: This case underscores the diagnostic challenge posed by Lemmel syndrome, a rare entity resulting from periampullary diverticulum-induced biliary obstruction. The patient's presentation with pancreatitis and biliary obstruction without evident choledocholithiasis highlights the importance of considering Lemmel syndrome in differential diagnoses. Advanced imaging techniques, particularly MRCP and EUS, were instrumental in identifying the periampullary diverticulum and assessing its impact on biliary anatomy. The therapeutic approach involved a combination of ERCP and EUS-guided interventions, demonstrating the utility of a multidisciplinary endoscopic strategy in managing complex biliary obstructions.
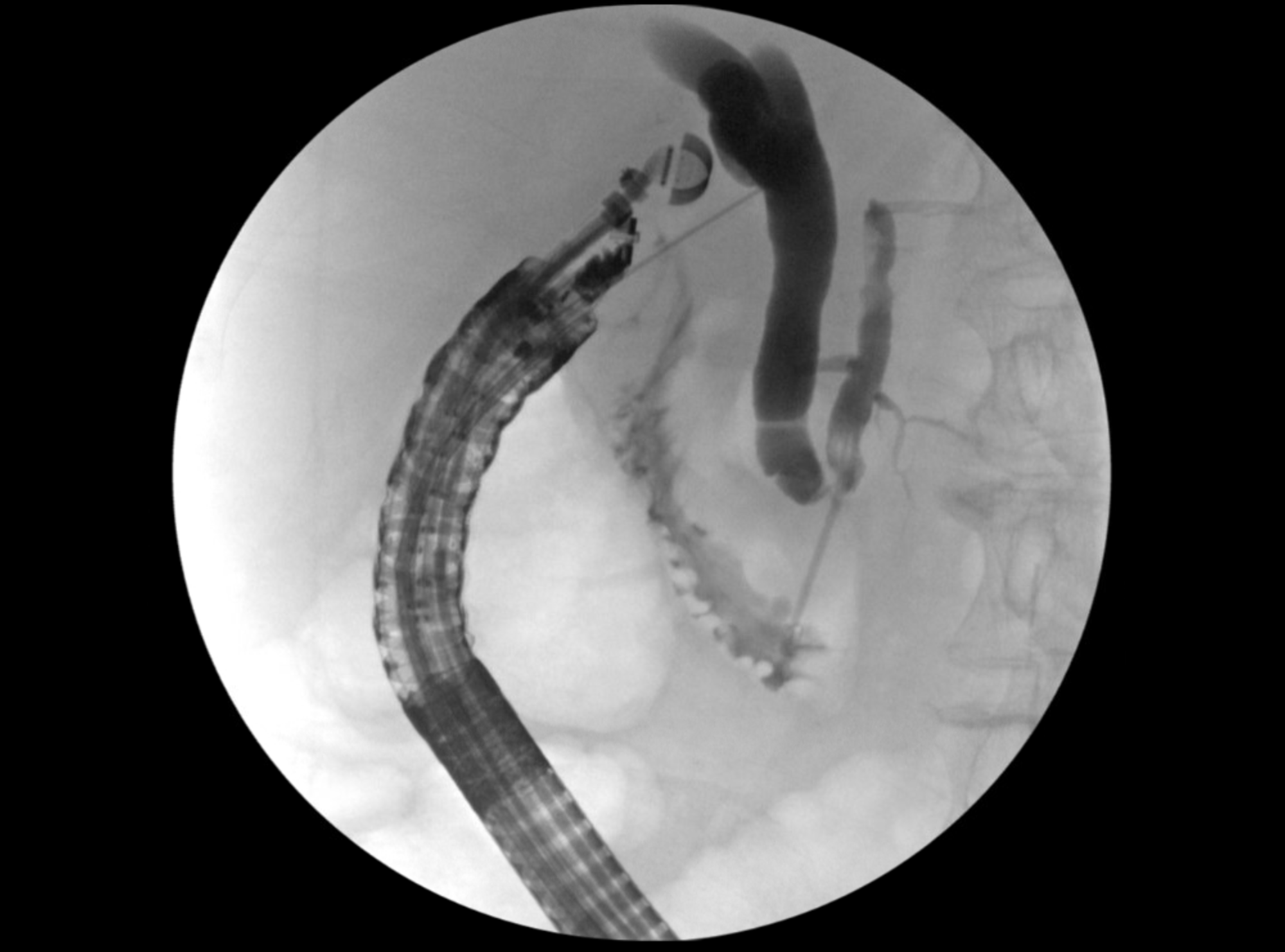
Figure: A 22-gauge FNA needle was punctured through the duodenal bulb wall into the bile duct and contrast was injected through the FNA needle to perform a cholangiogram. The distal 8 mm of CBD just above the ampulla appeared to be kinked with poor drainage into the duodenum, likely related to traction from the periampullary diverticulum

Figure: A extraction balloon was advanced into the bile duct and balloon sweeps yielded no stones or sludge
Disclosures:
Guneet Sidhu indicated no relevant financial relationships.
Ross Meidinger indicated no relevant financial relationships.
Guneet Sidhu, MD1, Ross Meidinger, MD2. P0901 - Lemmel Syndrome Unveiled: A Rare Case of Periampullary Diverticulum-Induced Biliary Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
