Sunday Poster Session
Category: GI Bleeding
P0983 - A Rare Cause of Upper Gastrointestinal Hemorrhage: Gastric Erosion of a Splenic Artery Pseudoaneurysm
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Valerie Quach, BS
John Sealy School of Medicine, University of Texas Medical Branch
Galveston, TX
Presenting Author(s)
Migara Jayasekera, MD1, Valerie Quach, BS2, Christo Mathew, MD3
1University of Texas Medical Branch, Galveston, TX; 2John Sealy School of Medicine, University of Texas Medical Branch, Galveston, TX; 3University of Texas Medical Branch, Department of Gastroenterology and Hepatology, Galveston, TX
Introduction: Splenic artery pseudoaneurysms are vascular anomalies caused by false expansion of the arterial wall due to disruption of the intimal and medial layers. They are most often associated with pancreatitis or abdominal trauma. These lesions carry a high rupture risk, with rates reported between 20–37%, and rupture mortality reaching 30–50%. Rarely, these pseudoaneurysms erode into the stomach, leading to hematemesis, melena, or hemodynamic collapse. This report highlights a rare etiology of gastrointestinal (GI) bleeding- a splenic artery pseudoaneurysm eroding into a gastric ulcer, requiring multiple interventions to stabilize the patient.
Case Description/
Methods: A 64-year-old woman with CHF, CKD presented to the emergency room with hematemesis. Her family noted she had abdominal and chest pain the night before, followed by several episodes of vomiting blood. She denied NSAID or steroid use but was on aspirin and had previously taken clopidogrel. On arrival, she was hypotensive (BP 92/32) and tachycardic (HR 100). Labs showed hemoglobin 7.7 g/dL (baseline 12), creatinine 1.74 mg/dL (baseline 0.8), BUN 43 mg/dL, and lactate 4.24 mmol/L. After a repeat episode of hematemesis, she was admitted to the critical care unit. Esophagogastroduodenoscopy (EGD) showed hematin in the esophagus with no active bleeding source; visualization of the gastric body and fundus was limited by clot burden. Angiography was deferred due to worsening renal function. Repeat EGD revealed a 15 mm cratered ulcer with a large, non-bleeding visible vessel (Forrest IIa) in the fundus. Hemostasis was attempted with Purastat, as the vessel was too large for clips. After extubation, the patient rebled and required reintubation. Emergent angiography revealed a splenic artery pseudoaneurysm. This was embolized and stabilized her bleeding. Her course was complicated by a femoral access site injury and subsequent wound infection. With clinical deterioration, the family opted for comfort care.
Discussion: Splenic artery pseudoaneurysms are rare but critical causes of upper GI bleeding. They may erode into adjacent structures and mimic more common lesions like peptic ulcers. Diagnosis requires high clinical suspicion, particularly in cases of recurrent or obscure bleeding with hemodynamic instability. Angiography is the preferred diagnostic tool. Given the high rupture risk, early intervention is essential. Embolization is first-line for stable patients, while surgery is reserved for those with rupture or failed endovascular therapy.
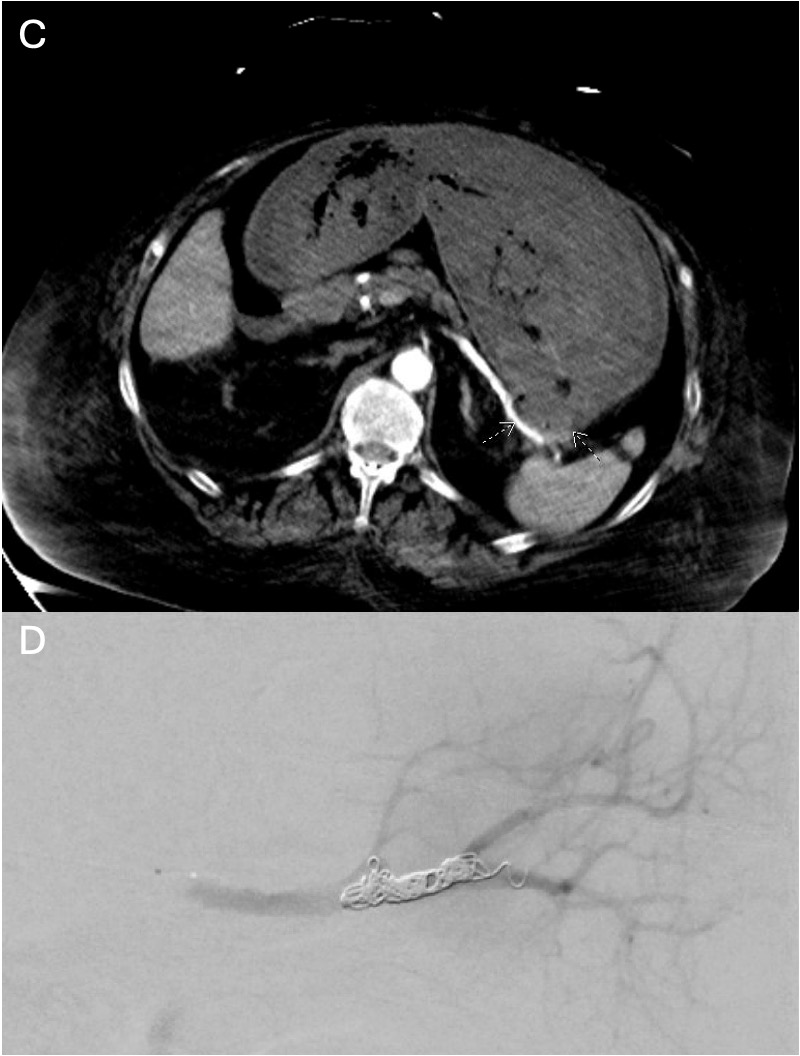
Figure: A- Gastric ulcer after biopsy and hemostat application
B- Ulcer with visible pseudoaneurysm vessel
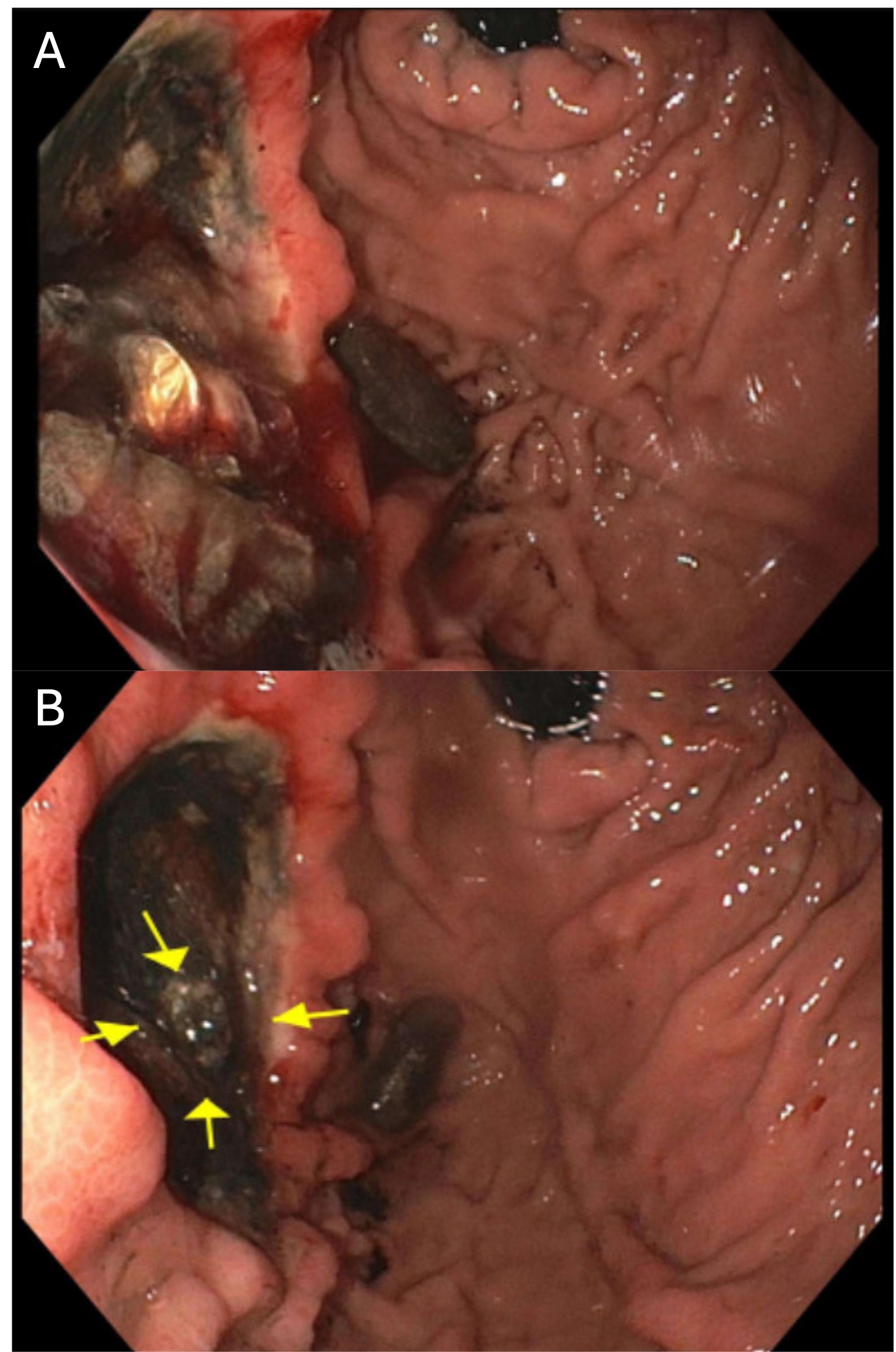
Figure: C- CT Abdomen showing splenic artery pseudoaneurysm protruding into a gastric ulcer
D- Angiographic embolization of the splenic artery pseudoaneurysm
Disclosures:
Migara Jayasekera indicated no relevant financial relationships.
Valerie Quach indicated no relevant financial relationships.
Christo Mathew indicated no relevant financial relationships.
Migara Jayasekera, MD1, Valerie Quach, BS2, Christo Mathew, MD3. P0983 - A Rare Cause of Upper Gastrointestinal Hemorrhage: Gastric Erosion of a Splenic Artery Pseudoaneurysm, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas Medical Branch, Galveston, TX; 2John Sealy School of Medicine, University of Texas Medical Branch, Galveston, TX; 3University of Texas Medical Branch, Department of Gastroenterology and Hepatology, Galveston, TX
Introduction: Splenic artery pseudoaneurysms are vascular anomalies caused by false expansion of the arterial wall due to disruption of the intimal and medial layers. They are most often associated with pancreatitis or abdominal trauma. These lesions carry a high rupture risk, with rates reported between 20–37%, and rupture mortality reaching 30–50%. Rarely, these pseudoaneurysms erode into the stomach, leading to hematemesis, melena, or hemodynamic collapse. This report highlights a rare etiology of gastrointestinal (GI) bleeding- a splenic artery pseudoaneurysm eroding into a gastric ulcer, requiring multiple interventions to stabilize the patient.
Case Description/
Methods: A 64-year-old woman with CHF, CKD presented to the emergency room with hematemesis. Her family noted she had abdominal and chest pain the night before, followed by several episodes of vomiting blood. She denied NSAID or steroid use but was on aspirin and had previously taken clopidogrel. On arrival, she was hypotensive (BP 92/32) and tachycardic (HR 100). Labs showed hemoglobin 7.7 g/dL (baseline 12), creatinine 1.74 mg/dL (baseline 0.8), BUN 43 mg/dL, and lactate 4.24 mmol/L. After a repeat episode of hematemesis, she was admitted to the critical care unit. Esophagogastroduodenoscopy (EGD) showed hematin in the esophagus with no active bleeding source; visualization of the gastric body and fundus was limited by clot burden. Angiography was deferred due to worsening renal function. Repeat EGD revealed a 15 mm cratered ulcer with a large, non-bleeding visible vessel (Forrest IIa) in the fundus. Hemostasis was attempted with Purastat, as the vessel was too large for clips. After extubation, the patient rebled and required reintubation. Emergent angiography revealed a splenic artery pseudoaneurysm. This was embolized and stabilized her bleeding. Her course was complicated by a femoral access site injury and subsequent wound infection. With clinical deterioration, the family opted for comfort care.
Discussion: Splenic artery pseudoaneurysms are rare but critical causes of upper GI bleeding. They may erode into adjacent structures and mimic more common lesions like peptic ulcers. Diagnosis requires high clinical suspicion, particularly in cases of recurrent or obscure bleeding with hemodynamic instability. Angiography is the preferred diagnostic tool. Given the high rupture risk, early intervention is essential. Embolization is first-line for stable patients, while surgery is reserved for those with rupture or failed endovascular therapy.
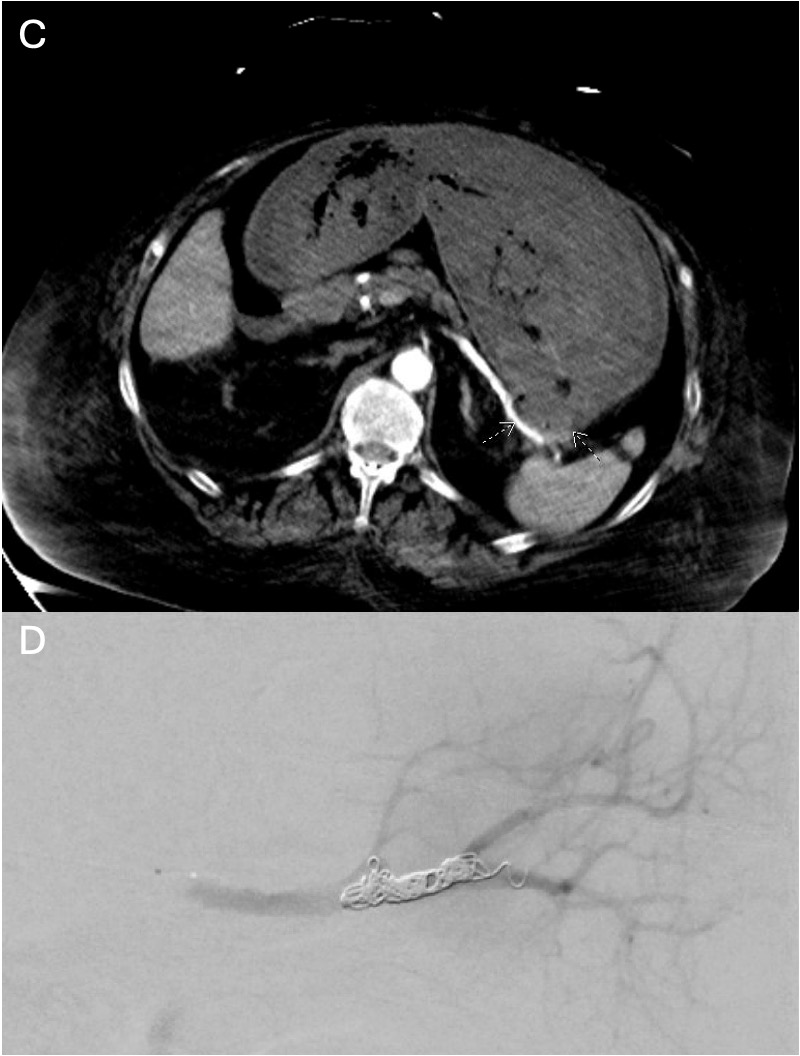
Figure: A- Gastric ulcer after biopsy and hemostat application
B- Ulcer with visible pseudoaneurysm vessel
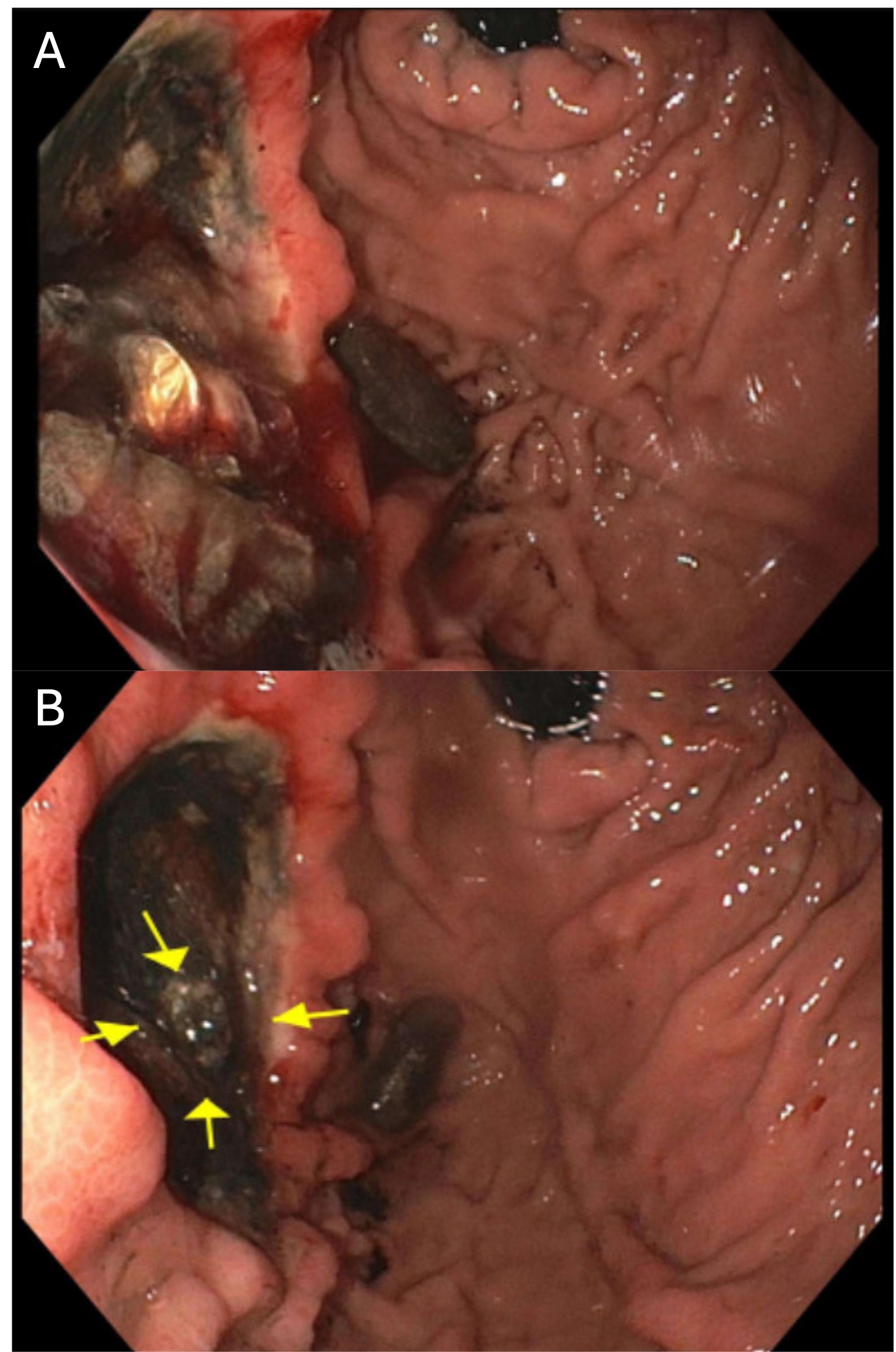
Figure: C- CT Abdomen showing splenic artery pseudoaneurysm protruding into a gastric ulcer
D- Angiographic embolization of the splenic artery pseudoaneurysm
Disclosures:
Migara Jayasekera indicated no relevant financial relationships.
Valerie Quach indicated no relevant financial relationships.
Christo Mathew indicated no relevant financial relationships.
Migara Jayasekera, MD1, Valerie Quach, BS2, Christo Mathew, MD3. P0983 - A Rare Cause of Upper Gastrointestinal Hemorrhage: Gastric Erosion of a Splenic Artery Pseudoaneurysm, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
