Sunday Poster Session
Category: GI Bleeding
P0975 - Dieulafoy's Lesion in the Distal Esophagus
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Thomas Rogan, MD (he/him/his)
Morristown Medical Center, Atlantic Health System
Morristown, NJ
Presenting Author(s)
Thomas Rogan, MD1, Joseph J. Berman, MD, MBA1, Paul Evens Gregoire Charles, MD1, Nicholas Tarangelo, MD2
1Morristown Medical Center, Atlantic Health System, Morristown, NJ; 2Affiliates in Gastroenterology, Morristown Medical Center, Morristown, NJ
Introduction: Dieulafoy lesions represent an uncommon etiology for GI bleeds accounting for approximately 2% of all cases. Most of these cases occur in the proximal stomach along the lesser curvature. Here we present a case of Dieulafoy lesion occurring in the distal esophagus.
Case Description/
Methods:
A 44 y/o F with complex PMHx most notable for cryptogenic cirrhosis, esophageal varices s/p banding, polysubstance abuse, cyclic vomiting syndrome presented to the ED for evaluation of non-bloody vomiting x1 week. On admission, patient developed hematemesis and underwent EGD which showed normal esophagus and gastrum without bleeding. Etiology of hematemesis presumed secondary to resolved Mallory Weiss tear in the setting of persistent vomiting. Several days later during the same admission, patient developed large volume hematemesis and hemorrhagic shock. Hb was initially 9.7 g/dL but decreased to 2.7 g/dL during this episode. MTP was ordered and patient initiated on pressors. Course complicated by presence of anti-C, anti-F, and JKA antibodies which delayed transfusion. Unmatched blood transfused in the acute setting.
Patient underwent emergent EGD which showed large Dieulafoy lesion on the L wall of the distal esophagus. This was injected with 3cc 1:10,000 epinephrine and hemoclip placed on the exposed bleeding vessel. Hemostasis was attained and patient sent to ICU for further stabilization.
Discussion: Dieulafoy lesions are dilated, aberrant submucosal blood vessels that erode through an otherwise normal epithelium and are not associated with an ulcer. They represent only 1 to 5.8% of acute upper GI bleeding cases, though the actual incidence is likely higher due to the difficult nature of diagnosing Dieulafoy lesions. Overall, etiology remains poorly understood. They are most often found along the lesser curvature of the stomach but can be found throughout the GI Tract. They often present as a massive arterial upper GI bleed. Diagnosis is confirmed through visualization during endoscopy but is often missed in the absence of active bleeding. Treatment includes a combination of epinephrine injection and cautery or hemostatic clips. There remains a high risk of rebleeding due to the large size of the underlying arteries.
A recent literature review of PubMed from 2021 revealed just 10 case reports discussing Esophageal Dieulafoy Lesions. While up to 1/3 of lesions may be found outside of the stomach, esophageal Dieulafoy lesions remain a rare etiology of acute upper GI bleeds.
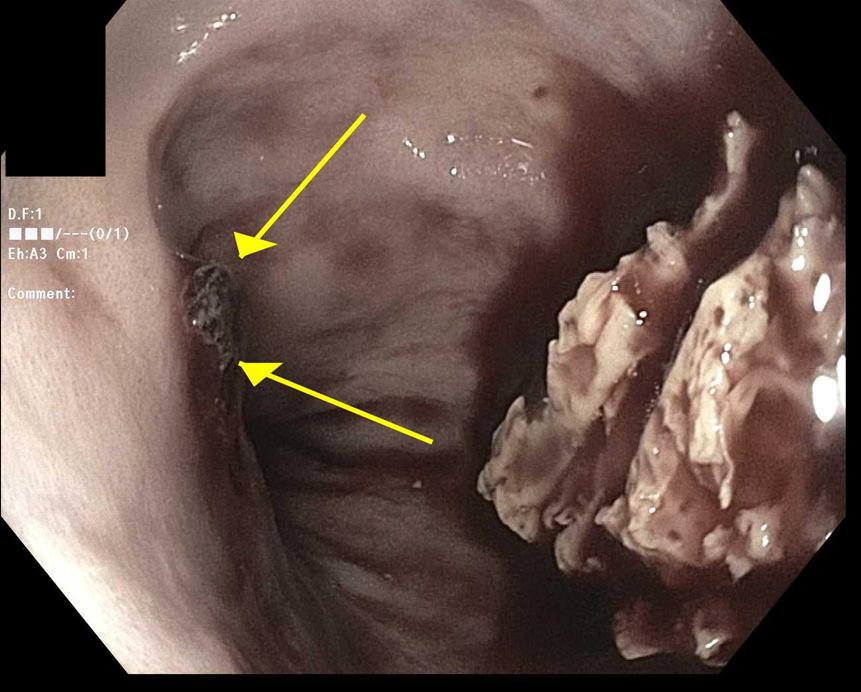
Figure: Esophageal Dieulafoy lesion
Disclosures:
Thomas Rogan indicated no relevant financial relationships.
Joseph Berman indicated no relevant financial relationships.
Paul Evens Gregoire Charles indicated no relevant financial relationships.
Nicholas Tarangelo indicated no relevant financial relationships.
Thomas Rogan, MD1, Joseph J. Berman, MD, MBA1, Paul Evens Gregoire Charles, MD1, Nicholas Tarangelo, MD2. P0975 - Dieulafoy's Lesion in the Distal Esophagus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Morristown Medical Center, Atlantic Health System, Morristown, NJ; 2Affiliates in Gastroenterology, Morristown Medical Center, Morristown, NJ
Introduction: Dieulafoy lesions represent an uncommon etiology for GI bleeds accounting for approximately 2% of all cases. Most of these cases occur in the proximal stomach along the lesser curvature. Here we present a case of Dieulafoy lesion occurring in the distal esophagus.
Case Description/
Methods:
A 44 y/o F with complex PMHx most notable for cryptogenic cirrhosis, esophageal varices s/p banding, polysubstance abuse, cyclic vomiting syndrome presented to the ED for evaluation of non-bloody vomiting x1 week. On admission, patient developed hematemesis and underwent EGD which showed normal esophagus and gastrum without bleeding. Etiology of hematemesis presumed secondary to resolved Mallory Weiss tear in the setting of persistent vomiting. Several days later during the same admission, patient developed large volume hematemesis and hemorrhagic shock. Hb was initially 9.7 g/dL but decreased to 2.7 g/dL during this episode. MTP was ordered and patient initiated on pressors. Course complicated by presence of anti-C, anti-F, and JKA antibodies which delayed transfusion. Unmatched blood transfused in the acute setting.
Patient underwent emergent EGD which showed large Dieulafoy lesion on the L wall of the distal esophagus. This was injected with 3cc 1:10,000 epinephrine and hemoclip placed on the exposed bleeding vessel. Hemostasis was attained and patient sent to ICU for further stabilization.
Discussion: Dieulafoy lesions are dilated, aberrant submucosal blood vessels that erode through an otherwise normal epithelium and are not associated with an ulcer. They represent only 1 to 5.8% of acute upper GI bleeding cases, though the actual incidence is likely higher due to the difficult nature of diagnosing Dieulafoy lesions. Overall, etiology remains poorly understood. They are most often found along the lesser curvature of the stomach but can be found throughout the GI Tract. They often present as a massive arterial upper GI bleed. Diagnosis is confirmed through visualization during endoscopy but is often missed in the absence of active bleeding. Treatment includes a combination of epinephrine injection and cautery or hemostatic clips. There remains a high risk of rebleeding due to the large size of the underlying arteries.
A recent literature review of PubMed from 2021 revealed just 10 case reports discussing Esophageal Dieulafoy Lesions. While up to 1/3 of lesions may be found outside of the stomach, esophageal Dieulafoy lesions remain a rare etiology of acute upper GI bleeds.
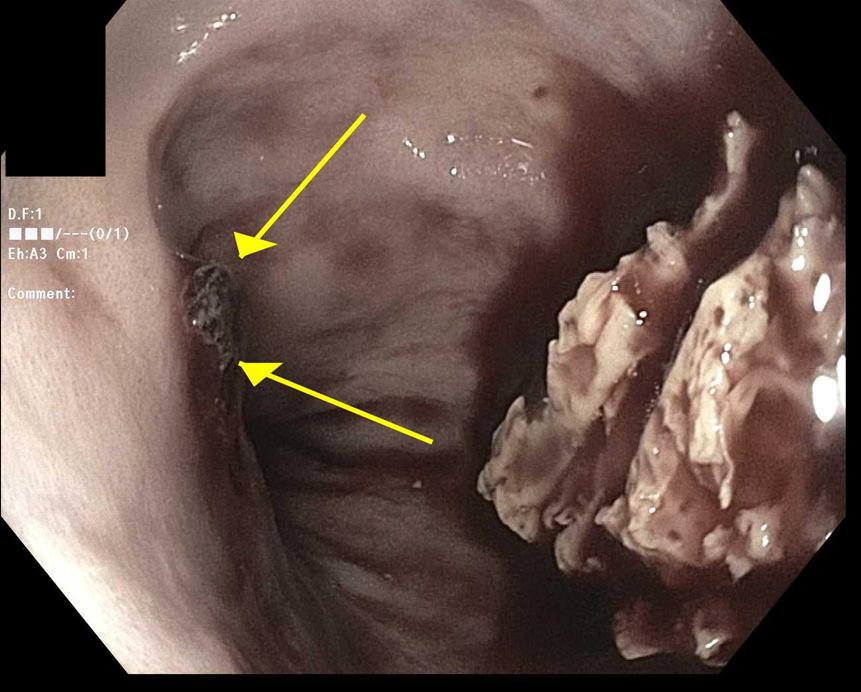
Figure: Esophageal Dieulafoy lesion
Disclosures:
Thomas Rogan indicated no relevant financial relationships.
Joseph Berman indicated no relevant financial relationships.
Paul Evens Gregoire Charles indicated no relevant financial relationships.
Nicholas Tarangelo indicated no relevant financial relationships.
Thomas Rogan, MD1, Joseph J. Berman, MD, MBA1, Paul Evens Gregoire Charles, MD1, Nicholas Tarangelo, MD2. P0975 - Dieulafoy's Lesion in the Distal Esophagus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
