Sunday Poster Session
Category: GI Bleeding
P0971 - A Case of Cytomegalovirus-Associated Gastric Ulcer Causing Hemorrhagic Shock in a Pre-Liver Transplant Patient
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Amber Hussain, MD
University Hospitals Cleveland Medical Center
Cleveland, OH
Presenting Author(s)
Amber Hussain, MD, Naemat Sandhu, MD, Jennifer Park, MD
University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: GI bleeding is a significant manifestation of CMV-related GI disease, with severity ranging from occult blood loss to life-threatening hemorrhage, particularly in immunocompromised hosts. CMV infection can affect various segments of the GI tract, presenting as esophagitis, gastritis, or colitis. Ulceration, however, is a rare presentation.
Case Description/
Methods: A 39-year-old woman with decompensated alcoholic cirrhosis and autoimmune hemolytic anemia on rituximab presented with abdominal pain and hypotension requiring vasopressor support. She was found to have colitis and ascites on CT abdomen. Blood cultures revealed Moraxella Catarrhalis bacteremia and urine culture grew E. Coli for which she was treated with antibiotics with clinical improvement of her septic shock. Hospital course was also notable for large volume paracentesis and autoimmune hemolytic anemia, requiring blood transfusion and dexamethasone course. Despite the above interventions, her clinical condition deteriorated with fever (despite negative ascitic and blood cultures), hepatic, and renal dysfunction.
Unfortunately, on hospital day 21, she developed significant hematemesis necessitating massive transfusion protocol. Subsequent EGD showed necrotic, friable mucosa with active bleeding at the GE junction and an ulcerated gastric mucosa. Embolization of the pancreaticoduodenal artery was ultimately required for hemostasis. Repeat EGD showed gastric ischemia, limited by clot burden on hospital day 22 and a large superficial ulcer from the lesser curvature to the fundus on hospital day 27 (images 1 and 2). Biopsies confirmed CMV-associated ulceration; CMV PCR was positive. IV ganciclovir was initiated. She underwent orthotopic liver transplantation one week later. Follow-up EGD one month later showed no evidence of infection on biopsy and showed improvement in appearance of gastric ulceration.
Discussion: Although this patient did present with abdominal pain and imaging evidence of colitis, it is unclear if CMV was contributing to these symptoms. It is rare for a CMV ulcer to erode into a vessel and result in severe, life-threatening hemorrhage. Importantly, the patient had not yet undergone liver transplantation or initiated immunosuppressive therapy when the ulcer developed, though she had been treated with rituximab and a short course of steroids for autoimmune hemolytic anemia. Fortunately, she was able to clear the viremia with a course of IV ganciclovir despite starting immunosuppression following her liver transplant.
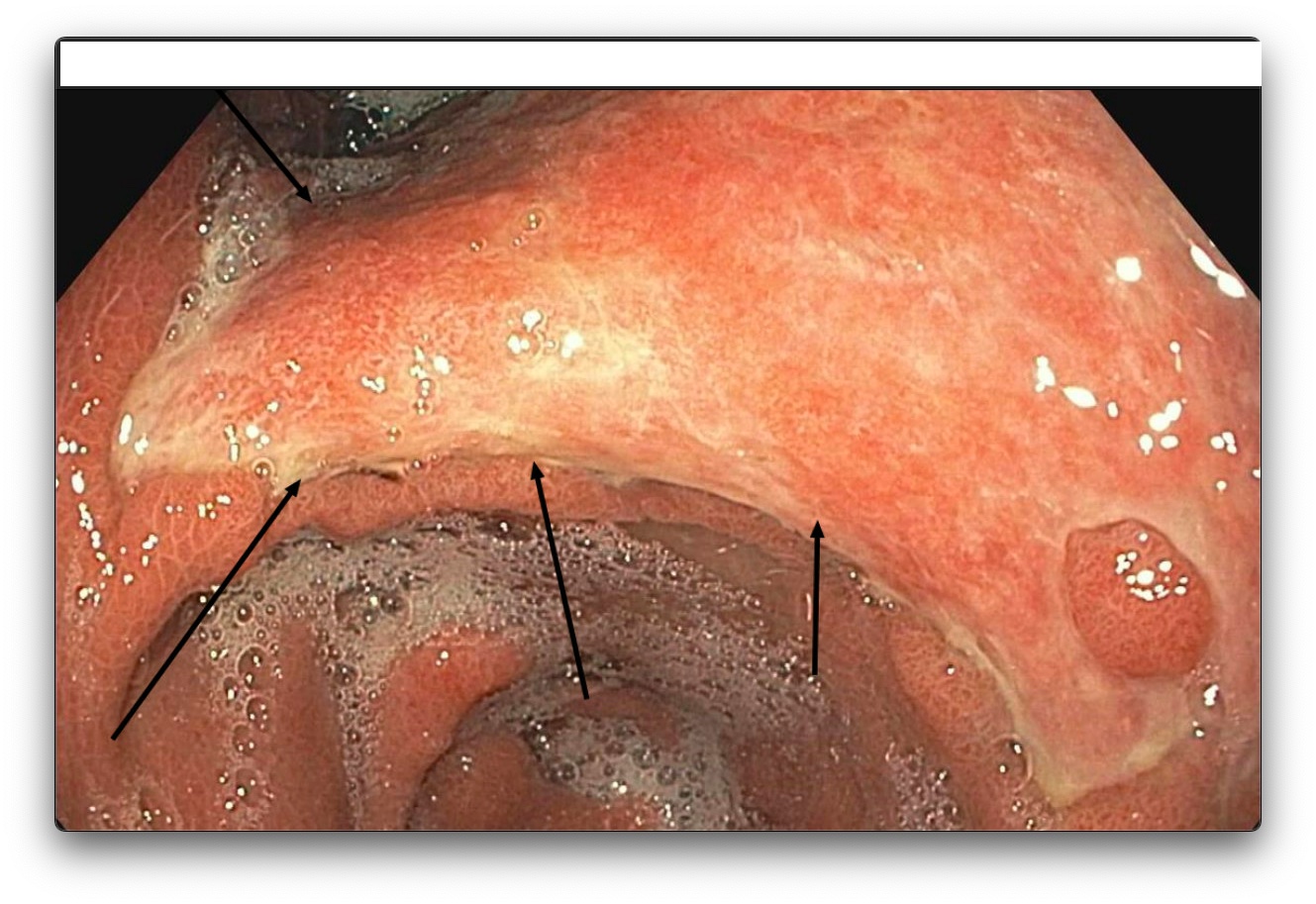
Figure: Diffuse ulceration of Incisura and gastric body on EGD

Figure: Ulceration along the incisura extending proximally along the gastric body, retroflexed stomach view
Disclosures:
Amber Hussain indicated no relevant financial relationships.
Naemat Sandhu indicated no relevant financial relationships.
Jennifer Park indicated no relevant financial relationships.
Amber Hussain, MD, Naemat Sandhu, MD, Jennifer Park, MD. P0971 - A Case of Cytomegalovirus-Associated Gastric Ulcer Causing Hemorrhagic Shock in a Pre-Liver Transplant Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: GI bleeding is a significant manifestation of CMV-related GI disease, with severity ranging from occult blood loss to life-threatening hemorrhage, particularly in immunocompromised hosts. CMV infection can affect various segments of the GI tract, presenting as esophagitis, gastritis, or colitis. Ulceration, however, is a rare presentation.
Case Description/
Methods: A 39-year-old woman with decompensated alcoholic cirrhosis and autoimmune hemolytic anemia on rituximab presented with abdominal pain and hypotension requiring vasopressor support. She was found to have colitis and ascites on CT abdomen. Blood cultures revealed Moraxella Catarrhalis bacteremia and urine culture grew E. Coli for which she was treated with antibiotics with clinical improvement of her septic shock. Hospital course was also notable for large volume paracentesis and autoimmune hemolytic anemia, requiring blood transfusion and dexamethasone course. Despite the above interventions, her clinical condition deteriorated with fever (despite negative ascitic and blood cultures), hepatic, and renal dysfunction.
Unfortunately, on hospital day 21, she developed significant hematemesis necessitating massive transfusion protocol. Subsequent EGD showed necrotic, friable mucosa with active bleeding at the GE junction and an ulcerated gastric mucosa. Embolization of the pancreaticoduodenal artery was ultimately required for hemostasis. Repeat EGD showed gastric ischemia, limited by clot burden on hospital day 22 and a large superficial ulcer from the lesser curvature to the fundus on hospital day 27 (images 1 and 2). Biopsies confirmed CMV-associated ulceration; CMV PCR was positive. IV ganciclovir was initiated. She underwent orthotopic liver transplantation one week later. Follow-up EGD one month later showed no evidence of infection on biopsy and showed improvement in appearance of gastric ulceration.
Discussion: Although this patient did present with abdominal pain and imaging evidence of colitis, it is unclear if CMV was contributing to these symptoms. It is rare for a CMV ulcer to erode into a vessel and result in severe, life-threatening hemorrhage. Importantly, the patient had not yet undergone liver transplantation or initiated immunosuppressive therapy when the ulcer developed, though she had been treated with rituximab and a short course of steroids for autoimmune hemolytic anemia. Fortunately, she was able to clear the viremia with a course of IV ganciclovir despite starting immunosuppression following her liver transplant.
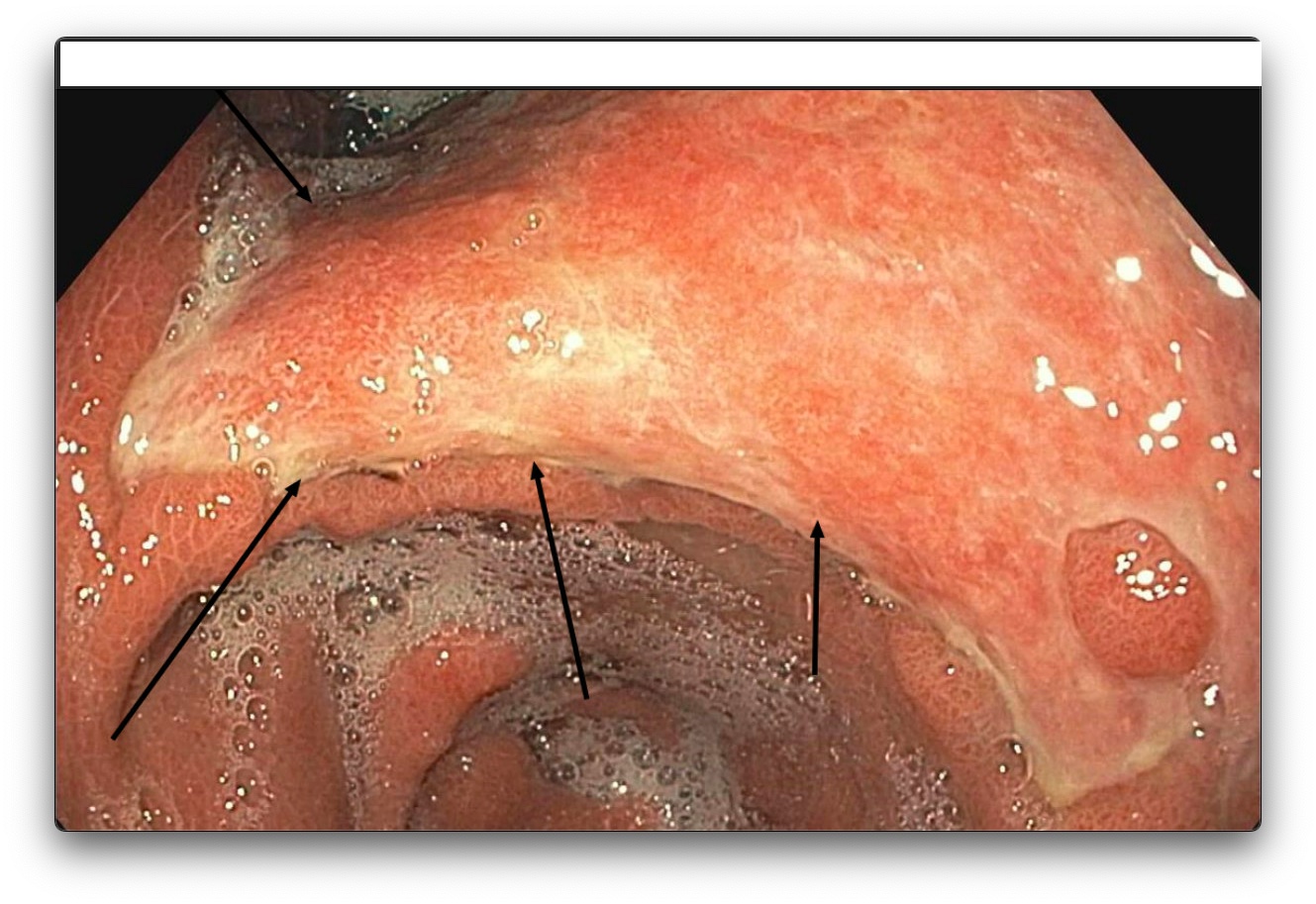
Figure: Diffuse ulceration of Incisura and gastric body on EGD

Figure: Ulceration along the incisura extending proximally along the gastric body, retroflexed stomach view
Disclosures:
Amber Hussain indicated no relevant financial relationships.
Naemat Sandhu indicated no relevant financial relationships.
Jennifer Park indicated no relevant financial relationships.
Amber Hussain, MD, Naemat Sandhu, MD, Jennifer Park, MD. P0971 - A Case of Cytomegalovirus-Associated Gastric Ulcer Causing Hemorrhagic Shock in a Pre-Liver Transplant Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
