Sunday Poster Session
Category: IBD
P1049 - The Risk of Serrated Lesions in Patients With Inflammatory Bowel Disease
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- AF
Adil Fazir, BS (he/him/his)
University of Massachusetts Chan Medical School
Worcester, Massachusetts
Presenting Author(s)
Ami Patel, DO, MPH1, Padmavathi Srivoleti, MD2, Sumayyah Akhtar, MD1, Adil Fazir, BS1, Ahmed El-Sadek, MD3, Abbas Rupawala, MD3
1University of Massachusetts Chan Medical School, Worcester, MA; 2University of Massachusetts Chan Medical School, Worester, MA; 3UMass Chan Medical School, Worcester, MA
Introduction: Colorectal cancer (CRC) arising from the serrated pathway accounts for approximately 20% of sporadic CRC. Patients with colonic Inflammatory Bowel Disease (IBD) are at increased risk of CRC and the relation between inflammation and dysplasia is well defined. However, there is limited literature on the risk of serrated adenomas (SA), thus this study aims to compare the incidence of SA in patients with IBD
Methods: In this single-center retrospective study, patients with IBD were compared to non-IBD patients who underwent screening or surveillance colonoscopy between Jan 1, 2024-June 30, 2024. The primary outcome was presence of SA on colonoscopy during the study time, herein referred to as “index colonoscopy”. Secondary outcomes included overall risk of SA and tubular adenoma (TA) considering all prior colonoscopies. Additionally, a query of the TriNetX database using data from 70 health care organizations in the U.S was then used to validate these findings comparing IBD patients to age, sex, race and ethnicity propensity score matched (PSM) patients without IBD.
Results: A total of 286 patients were included, of which 102 had IBD (33 UC and 69 CD) and 184 were controls. Patients with IBD were younger (54 years old vs. 63, p< 0.01) and more likely to have prior colonoscopies (94.1% vs. 70.7%, p< 0.01, Table 1). Patients with IBD were less likely to have SA (0% vs. 6.5%, p< 0.01) on index colonoscopy compared to non-IBD patients (Fig. 1).
When controlling for age, history of prior polyps, and prior colonoscopies, there was no difference in the risk of SA (OR 0.57, 95% CI 0.17-1.84, p=0.34) between IBD and non-IBD patients, though IBD was protective against the risk of polyps in general (OR 0.112, 95% CI 0.06-0.23, p< 0.01) and risk of TA (OR 0.14, 95% CI 0.07-0.28, p< 0.01). No significant differences were found in the risk of SA (OR2.59, 95% CI 0.23-29, p=0.44) in patients with CD compared to UC.
Additionally, 105,329 IBD patients were compared to PSM controls using TrinetX. IBD was protective against serrated adenomas (OR 0.62, 95% CI 0.55-0.69, p< 0.01) and polyps in general (OR 0.8, 95% CI 0.78-0.81, p< 0.01).
Discussion: Despite patients with IBD being at a greater risk of dysplasia our study shows that they are not at an increased risk of developing SA when compared to patients without IBD. IBD patients may have a protective effect against SA, which may be masked by the low sample size in our cohort, although it is more evident in the national cohort from the TrinetX database.
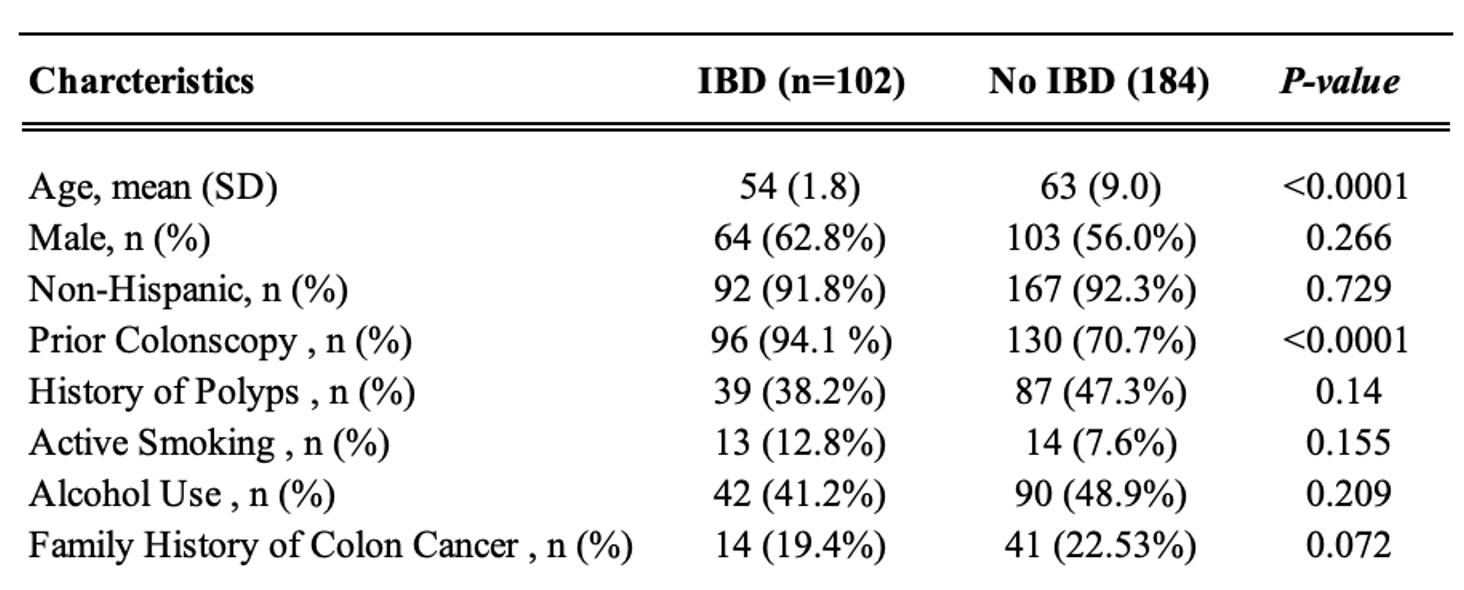
Figure: Table 1. Baseline characteristics comparing IBD patients to non-IBD patients.
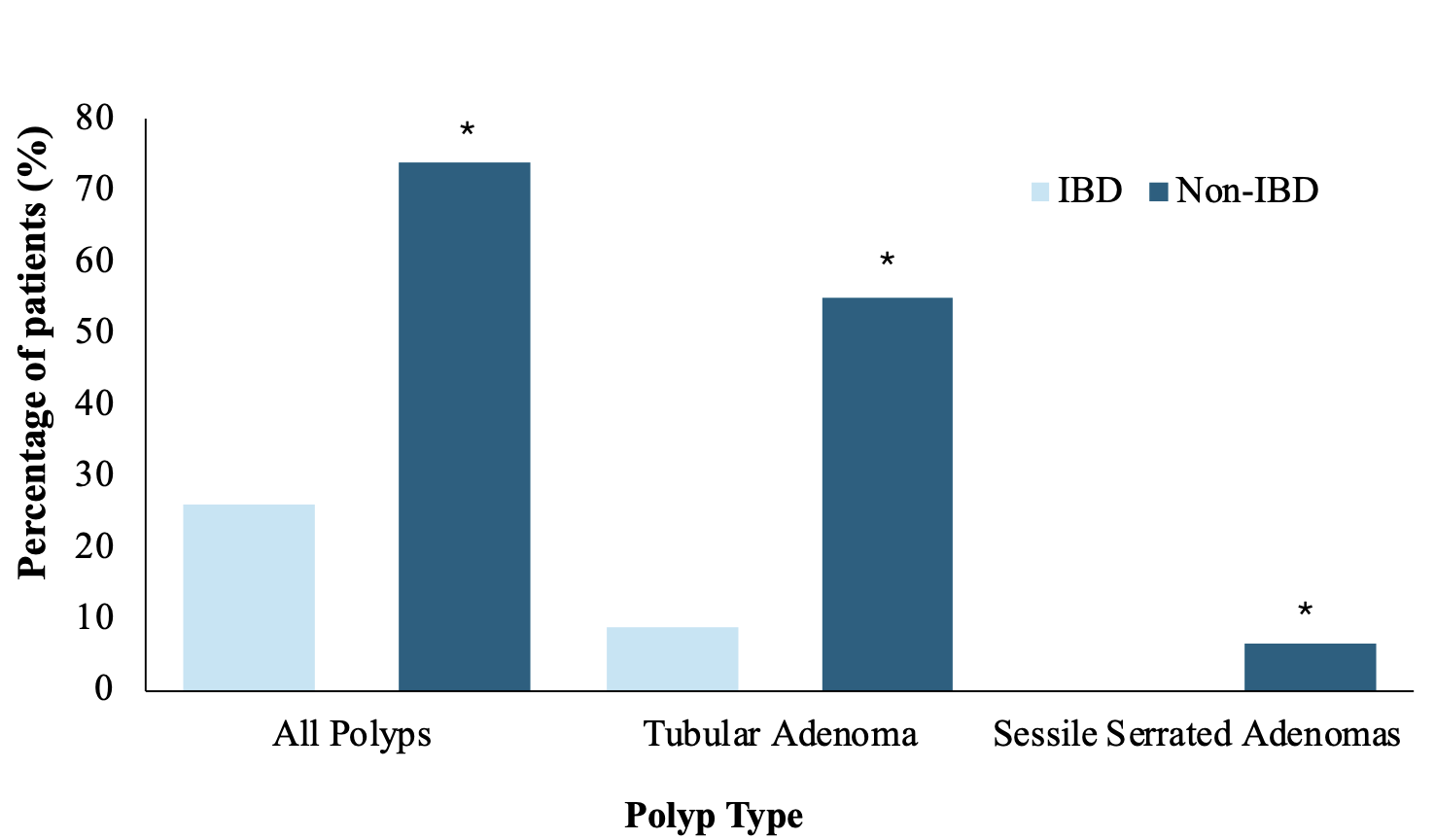
Figure: Figure 1. Incidence of polyps on index colonoscopy in IBD patients compared to non IBD patients (* p<0.05).
Disclosures:
Ami Patel indicated no relevant financial relationships.
Padmavathi Srivoleti indicated no relevant financial relationships.
Sumayyah Akhtar indicated no relevant financial relationships.
Adil Fazir indicated no relevant financial relationships.
Ahmed El-Sadek indicated no relevant financial relationships.
Abbas Rupawala: Abbvie – Consultant, Speakers Bureau. Pfizer – Consultant. Takeda – Consultant.
Ami Patel, DO, MPH1, Padmavathi Srivoleti, MD2, Sumayyah Akhtar, MD1, Adil Fazir, BS1, Ahmed El-Sadek, MD3, Abbas Rupawala, MD3. P1049 - The Risk of Serrated Lesions in Patients With Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Massachusetts Chan Medical School, Worcester, MA; 2University of Massachusetts Chan Medical School, Worester, MA; 3UMass Chan Medical School, Worcester, MA
Introduction: Colorectal cancer (CRC) arising from the serrated pathway accounts for approximately 20% of sporadic CRC. Patients with colonic Inflammatory Bowel Disease (IBD) are at increased risk of CRC and the relation between inflammation and dysplasia is well defined. However, there is limited literature on the risk of serrated adenomas (SA), thus this study aims to compare the incidence of SA in patients with IBD
Methods: In this single-center retrospective study, patients with IBD were compared to non-IBD patients who underwent screening or surveillance colonoscopy between Jan 1, 2024-June 30, 2024. The primary outcome was presence of SA on colonoscopy during the study time, herein referred to as “index colonoscopy”. Secondary outcomes included overall risk of SA and tubular adenoma (TA) considering all prior colonoscopies. Additionally, a query of the TriNetX database using data from 70 health care organizations in the U.S was then used to validate these findings comparing IBD patients to age, sex, race and ethnicity propensity score matched (PSM) patients without IBD.
Results: A total of 286 patients were included, of which 102 had IBD (33 UC and 69 CD) and 184 were controls. Patients with IBD were younger (54 years old vs. 63, p< 0.01) and more likely to have prior colonoscopies (94.1% vs. 70.7%, p< 0.01, Table 1). Patients with IBD were less likely to have SA (0% vs. 6.5%, p< 0.01) on index colonoscopy compared to non-IBD patients (Fig. 1).
When controlling for age, history of prior polyps, and prior colonoscopies, there was no difference in the risk of SA (OR 0.57, 95% CI 0.17-1.84, p=0.34) between IBD and non-IBD patients, though IBD was protective against the risk of polyps in general (OR 0.112, 95% CI 0.06-0.23, p< 0.01) and risk of TA (OR 0.14, 95% CI 0.07-0.28, p< 0.01). No significant differences were found in the risk of SA (OR2.59, 95% CI 0.23-29, p=0.44) in patients with CD compared to UC.
Additionally, 105,329 IBD patients were compared to PSM controls using TrinetX. IBD was protective against serrated adenomas (OR 0.62, 95% CI 0.55-0.69, p< 0.01) and polyps in general (OR 0.8, 95% CI 0.78-0.81, p< 0.01).
Discussion: Despite patients with IBD being at a greater risk of dysplasia our study shows that they are not at an increased risk of developing SA when compared to patients without IBD. IBD patients may have a protective effect against SA, which may be masked by the low sample size in our cohort, although it is more evident in the national cohort from the TrinetX database.
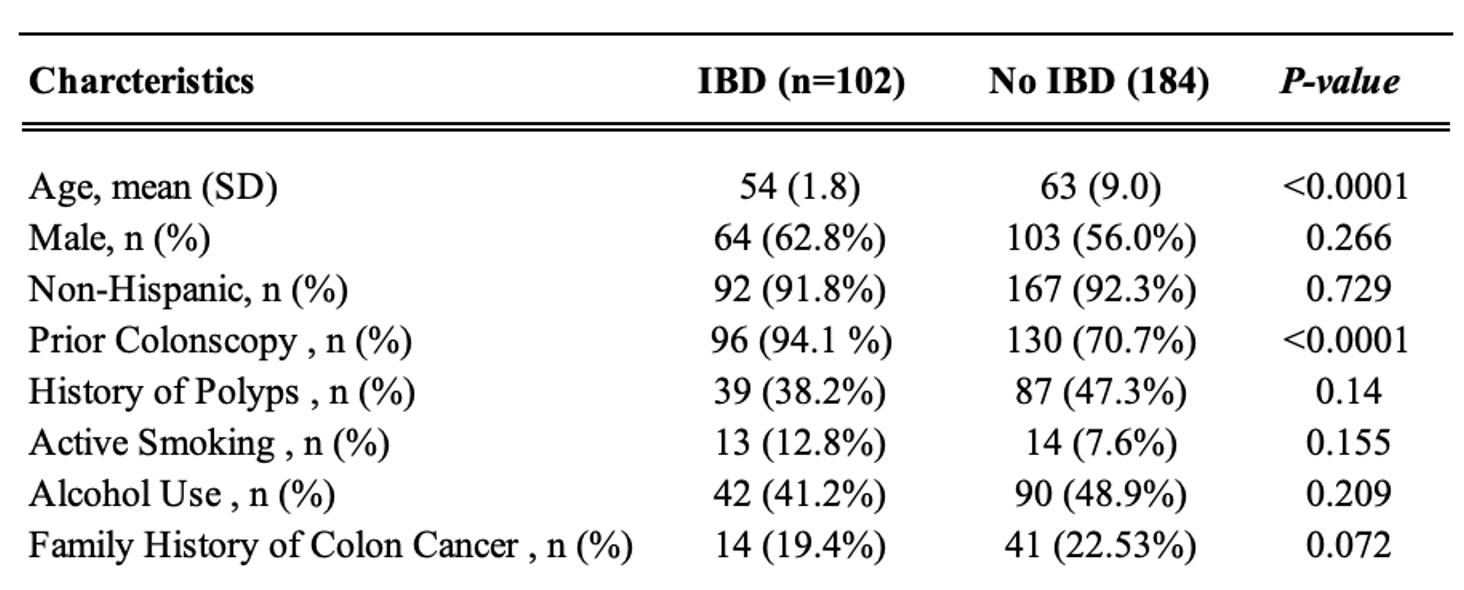
Figure: Table 1. Baseline characteristics comparing IBD patients to non-IBD patients.
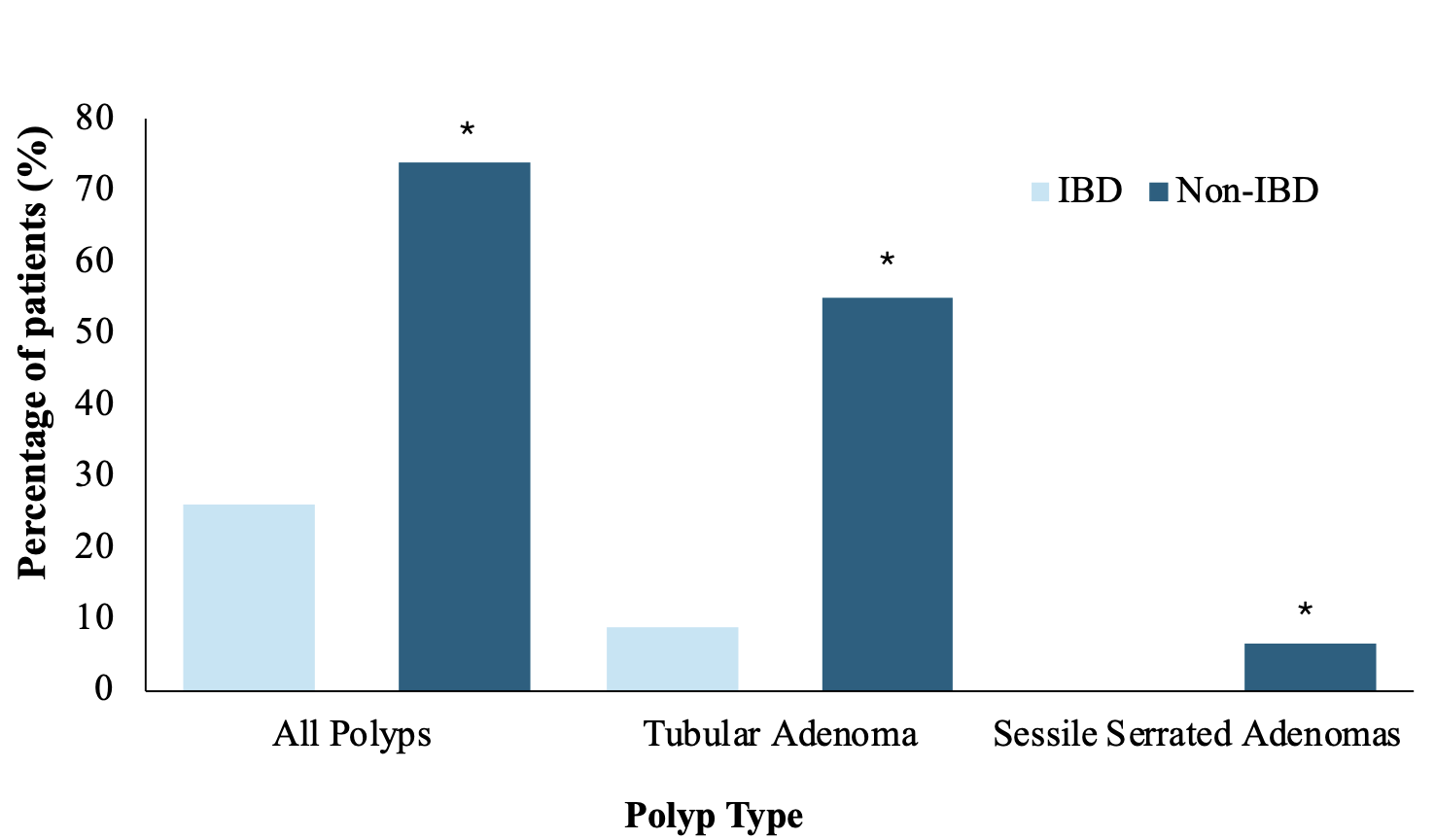
Figure: Figure 1. Incidence of polyps on index colonoscopy in IBD patients compared to non IBD patients (* p<0.05).
Disclosures:
Ami Patel indicated no relevant financial relationships.
Padmavathi Srivoleti indicated no relevant financial relationships.
Sumayyah Akhtar indicated no relevant financial relationships.
Adil Fazir indicated no relevant financial relationships.
Ahmed El-Sadek indicated no relevant financial relationships.
Abbas Rupawala: Abbvie – Consultant, Speakers Bureau. Pfizer – Consultant. Takeda – Consultant.
Ami Patel, DO, MPH1, Padmavathi Srivoleti, MD2, Sumayyah Akhtar, MD1, Adil Fazir, BS1, Ahmed El-Sadek, MD3, Abbas Rupawala, MD3. P1049 - The Risk of Serrated Lesions in Patients With Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
