Sunday Poster Session
Category: IBD
P1047 - Pattern of Joint Distribution in Peripheral Arthritis Does Not Alter Health-Related Quality of Life Across Multiple Patient-Reported Outcomes – Results From the CHASE Cohort
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Katherine Falloon, MD
Cleveland Clinic Foundation
Chagrin Falls, OH
Presenting Author(s)
Katherine Falloon, MD1, Suha Abushamma, MD1, Ashwin Ananthakrishnan, 2, Edward L. Barnes, MD, MPH3, Abhik Bhattacharya, MD4, Raymond K. Cross, MD, MS, FACG5, Shashank Cheemalavagu, MD1, Jean-Frederic Colombel, MD4, Emily Gore, MD4, Hans Herfarth, MD, PhD6, Sara Horst, MD, MPH, FACG7, M. Elaine Husni, MD1, Jeremy A.. Klein, MD8, Dana J. Lukin, MD, PhD, FACG9, David T. Rubin, MD10, Ellen J. Scherl, MD9, Taha Qazi, MD1, Qijun Yang, MS11, Benjamin L. Cohen, MD1, Brian G. Feagan, MD12, Florian Rieder, MD1
1Cleveland Clinic Foundation, Cleveland, OH; 2Division of Gastroenterology, Massachusetts General Hospital and Harvard Medical School, Boston, MA; 3Multidisciplinary Inflammatory Bowel Diseases Center, Division of Gastroenterology and Hepatology, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA, Chapel Hill, NC; 4Icahn School of Medicine at Mount Sinai, New York, NY; 5The Melissa L. Posner Institute for Digestive Health & Liver Disease, Mercy Medical Center, Baltimore, MD; 6University of North Carolina at Chapel Hill, Chapel Hill, NC, USA, Chapel Hill, NC; 7Vanderbilt University School of Medicine, Nashville, TN; 8University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL; 9Jill Roberts Center for Inflammatory Bowel Disease, Weill Cornell Medicine, New York, NY; 10University of Chicago Medicine Inflammatory Bowel Disease Center, Chicago, IL, USA, Chicago, IL; 11Cleveland Clinic, Cleveland, OH; 12Division of Gastroenterology, Department of Medicine, University of Western Ontario and Alimentiv, London, ON, Canada
Introduction: Inflammatory bowel disease (IBD)-associated peripheral spondylarthritis (IBD-pSpA) is common but not well studied, with limited research regarding impact on health-related quality of life (HRQoL). The type I vs type II classification schema, which groups patient based on the distribution, number and size of involved joints, is commonly utilized in the gastroenterology literature. However, this schema is neither widely accepted within the rheumatology literature nor prospectively validated. The aim of this study was to evaluate whether the HRQoL scores vary based on the type I vs type II classification schema.
Methods: We prospectively recruited patients with IBD-pSpA, defined by previously established consensus criteria via the Cohort for Healing Arthritis, Skin, and Eye Extra-Intestinal Manifestations (CHASE-EIM) from six sites across the United States. The relationship of clinical presentation of IBD-pSpA (number and type of involved peripheral joints) on HRQoL was assessed via three previously validated patient reported outcomes – the Inflammatory Bowel Disease Questionnaire (IBDQ), the Work Productivity and Activity Impairment Questionnaire (WPAI), and the Functional Assessment of Chronic Illness Therapy – Fatigue (FACIT-F). Analyses were performed using R software and a significance level of 0.05 was assumed for all tests.
Results: 134 patients with IBD-pSpA (61.2% female, 70.1% with CD) were included in the analysis (Table 1). 47.3% of patients had < 5 joints involved and the remainder ≥5. Hands (65.7%) and knees (58.2%) were the most commonly involved joints. 103 patients completed the requested questionnaires (76.9%). There were no statistically significant differences in any of the questionnaire scores based on number of swollen or tender joints or location of swollen or tender joints (Table 2, data for hands and knees reported; data for other joints not shown but no statistically significant differences identified).
Discussion: Pattern of joint involvement did not influence HRQoL across multiple previously validated PROs (IBDQ, WPAI, and FACIT-F) in patients with IBD-pSpA, casting additional doubt regarding the clinical utility of the type I vs type II classification schema in this patient population. Development of a novel PRO specific to IBD-pSpA will provide further insights into the clinical impact of IBD-pSpA and is currently underway by our group.
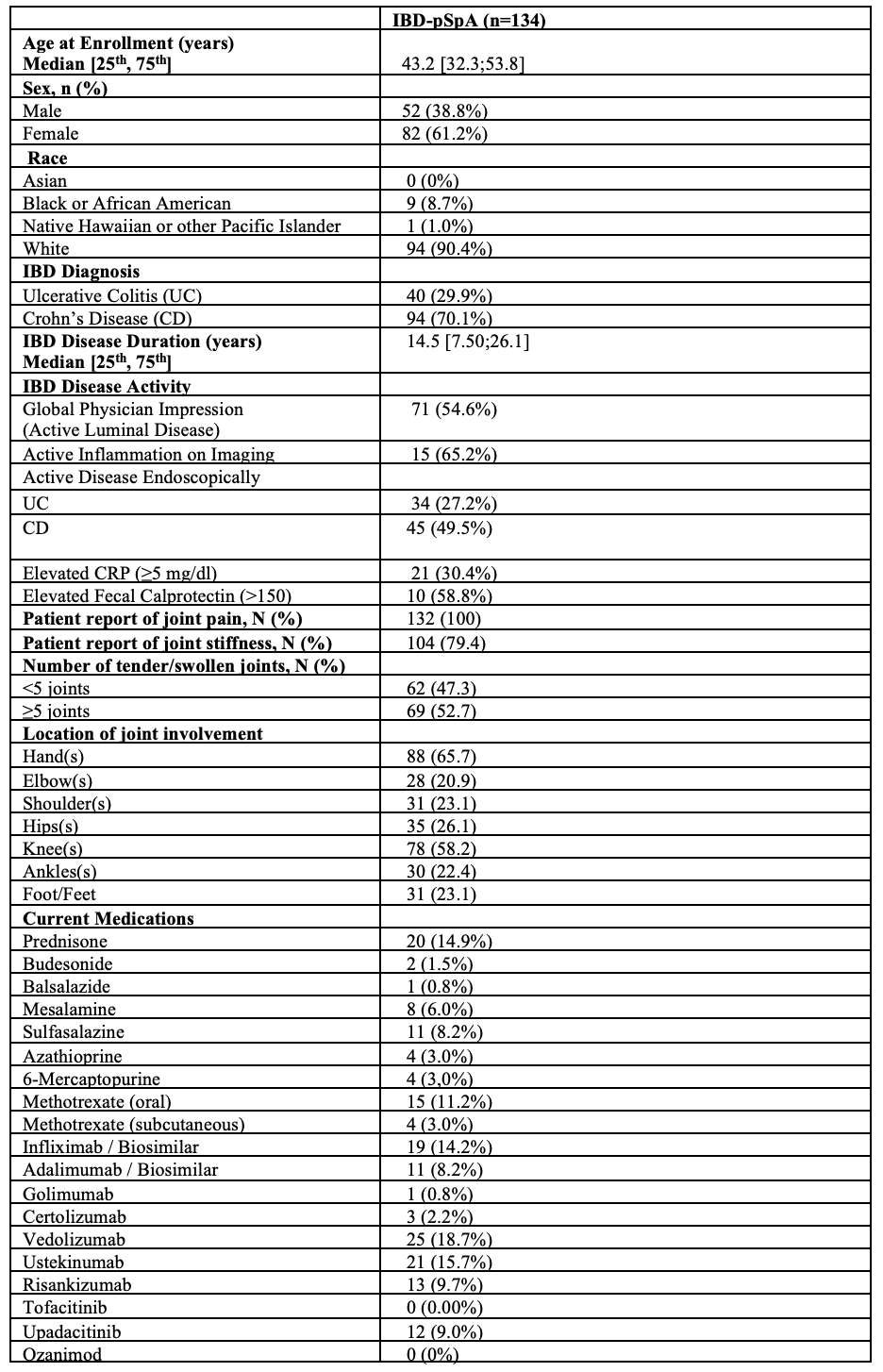
Figure:
Table 1: Baseline Demographics and Clinical Characteristics
IBD-pSpA = inflammatory bowel disease associated peripheral spondyloarthritis, CRP = C reactive protein
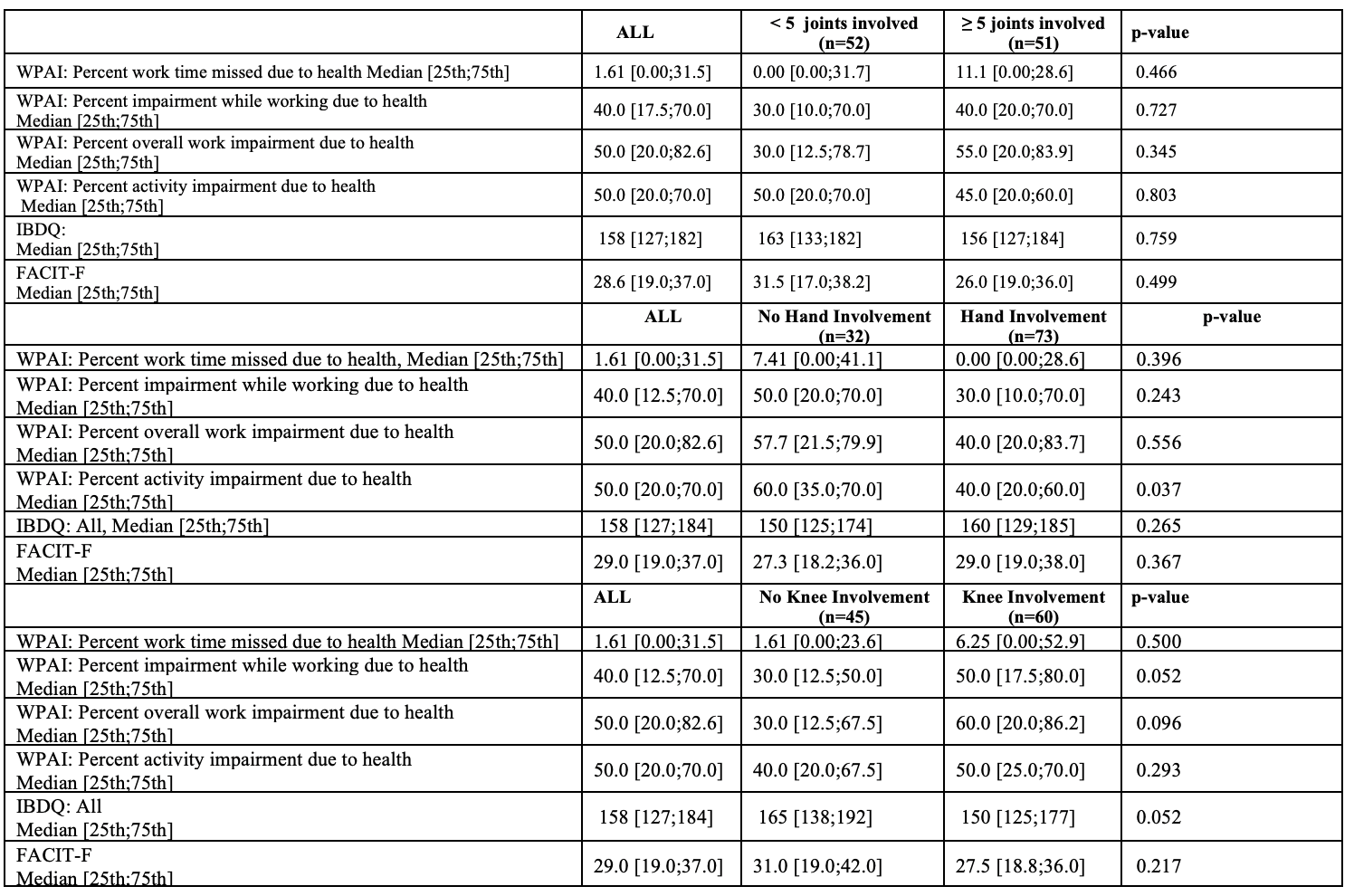
Figure: Table 2: Questionnaire Scores Based on Pattern of Joint Involvement
WPAI = work productivity and activity impairment questionnaire, IBDQ = inflammatory bowel disease questionnaire, FACIT=F = functional assessment of chronic illness therapy
Disclosures:
Katherine Falloon: Cardinal Health, Inc. – Husband is employee. Janssen Pharmaceuticals, Inc. – Consultant. MD Education – Speaker. Pfizer – Grant/Research Support. Takeda Pharmaceuticals, Inc. – Speaker.
Suha Abushamma indicated no relevant financial relationships.
Ashwin Ananthakrishnan: Takeda – Grant/Research Support.
Edward Barnes: AbbVie, Inc. – Consultant. Boomerang – Consultant. Eli Lilly – Consultant. Eli Lilly – Grant/Research Support. Pfizer – Consultant. Sanofi – Consultant. Takeda – Consultant. Target RWE – Consultant.
Abhik Bhattacharya indicated no relevant financial relationships.
Raymond K. Cross: Abbvie – Advisor or Review Panel Member, Consultant, Speakers Bureau. BMS – Advisor or Review Panel Member, Consultant, Speakers Bureau. CorEvitas – Advisory Committee/Board Member. Fresenius Kabi – Advisory Committee/Board Member, Consultant. Genetech – Advisory Committee/Board Member, Consultant. Gilead – Advisory Committee/Board Member, Consultant. IBD Education Group – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Magellan Health – Advisory Committee/Board Member, Consultant. Option Care – Advisory Committee/Board Member, Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Speakers Bureau. Pharmacosmos – Advisory Committee/Board Member, Consultant. Samsung Bioepis – Advisory Committee/Board Member, Consultant. Sandoz – Advisory Committee/Board Member, Consultant. Takeda – Grant/Research Support.
Shashank Cheemalavagu indicated no relevant financial relationships.
Jean-Frederic Colombel: AbbVie – Grant/Research Support, Personal fees. Amgen – Personal fees. Boehringer Ingelheim – Personal fees. Celgene – Personal fees. Celltrion – Personal fees. Enterome – Personal fees. Ferring – Personal fees. Genentech – Personal fees. Genfit – Stock Options. Intestinal Biotech Development – Stock Options. Janssen – Grant/Research Support, Personal fees. MedImmune – Consultant, Personal fees. Merck – Personal fees. Pfizer – Personal fees. PPM Services – Personal fees. Protagonist – Personal fees. Second Genome – Personal fees. Seres – Personal fees. Shire – Personal fees. Takeda – Grant/Research Support, Personal fees. Theradiag – Personal fees.
Emily Gore indicated no relevant financial relationships.
Hans Herfarth: Celltrion – Consultant. ExeGi – Consultant. Gilead – Consultant. Janssen – Consultant. Lilly – Grant/Research Support. Novo Nordisk – Grant/Research Support.
Sara Horst: Abbvie – Consultant. Biocon – Consultant. Celltrion – Consultant. J&J – Consultant. Pfizer – Consultant. Takeda – Consultant.
M. Elaine Husni: Abbvie – Consultant. BMS – Consultant. Eli Lilly – Consultant. Janssen Pharmaceuticals, Inc. – Consultant. Novartis – Consultant. PASE Questionnaire, Co-Inventor – Royalties. UCB – Consultant.
Jeremy Klein indicated no relevant financial relationships.
Dana Lukin: AbbVie – Consultant, Grant/Research Support, Speakers Bureau. Altrubio – Consultant. Boehringer Ingelheim – Consultant, Grant/Research Support. Bristol Myers Squibb – Consultant. Johnson & Johnson – Consultant, Grant/Research Support, Speakers Bureau. Palatin Technologies – Consultant. Pfizer – Consultant. Prime – Consultant. PSI – Consultant. Takeda – Consultant. Vedanta – Consultant.
David Rubin: AbbVie – Advisory Committee/Board Member, Consultant, Speaker fees. Abivax SA – Consultant. Altrubio – Advisory Committee/Board Member, Consultant, Speaker feees, Stock Options. Avalo – Advisory Committee/Board Member, Consultant, Speaker fees. Bausch Health – Consultant. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant, Speaker fees. Buhlmann Diagnostics – Advisory Committee/Board Member, Consultant, Speaker fees. Celltrion – Consultant. ClostraBio – Consultant. Connect BioPharma – Consultant. Cornerstones Health, Inc – Board of Directors membership. Douglas Pharmaceuticals – Consultant. Eli Lilly & Co. – Consultant. Foresee, Genentech (Roche) Inc. – Consultant. Image Analysis Group – Consultant. InDex Pharmaceutical – Consultant. Intouch Group – Advisory Committee/Board Member, Consultant, Speaker fees. Iterative Health – Advisory Committee/Board Member, Consultant, Speaker fees. Iterative Health – Stock Options. Janssen Pharmaceuticals – Consultant. Lilly – Advisory Committee/Board Member, Consultant, Speaker fees. Odyssey Therapeutics – Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Speaker fees. Sanofi – Consultant. Takeda – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speaker fees. Throne – Consultant. Vedanta – Consultant.
Ellen Scherl indicated no relevant financial relationships.
Taha Qazi: Abbvie – Advisor or Review Panel Member, Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Celltirion – Grant/Research Support. Eli Lilly – Advisor or Review Panel Member, Advisory Committee/Board Member, Consultant. Johnson and Johnson – Advisor or Review Panel Member, Advisory Committee/Board Member, Consultant, Speakers Bureau. pfizer – Grant/Research Support.
Qijun Yang indicated no relevant financial relationships.
Benjamin Cohen: Abbvie – Advisory Committee/Board Member, Consultant, Speakers Bureau. ALPCO – Advisory Committee/Board Member, Consultant. Emmes Biopharma Services LLC – DSMB. J&J Innovative Medicine – Advisory Committee/Board Member. Pfizer – Advisory Committee/Board Member. Takeda – Consultant, Speakers Bureau.
Brian G. Feagan: Abbvie – Advisory Committee/Board Member, Consultant, honoraria. Abivax – Consultant. Adiso – Consultant. AgomAb Therapeutics – Consultant. Allianthera – Consultant. Amgen – Consultant. AnaptysBio – Advisory Committee/Board Member, Consultant. Arena Pharma – Consultant. Atomwise – Consultant. Avoro Capital Advisors – Consultant. BioJamp – Consultant. Biora Therapeutics – Consultant. Blackbird Laboratories – Consultant. Boehringer Ingelheim – Advisory Committee/Board Member, Consultant. Boxer Capital – Consultant. Celgene/BMS – Advisory Committee/Board Member, Consultant. Connect BioPharma – Consultant, Stock-publicly held company(excluding mutual/index funds). Cytoki – Consultant. Disc Medicine – Consultant. Duality – Consultant. EcoR1Capital – Advisory Committee/Board Member, Consultant. Eli Lilly – Advisory Committee/Board Member, Consultant. EnGene – Stock-publicly held company(excluding mutual/index funds). Equillium – Consultant. Ermium – Consultant. Evida – Stock-privately held company. First Wave – Consultant. Forbion – Consultant. Galapagos – Consultant. Galen Atlantica – Consultant. Genentech/Roche – Advisory Committee/Board Member, Consultant. Gilead – Consultant. GlaxoSmithKline – Advisory Committee/Board Member, Consultant. Gossamer Pharma – Consultant. Hinge Bio – Consultant. Imhotex – Consultant. Immunic Therapeutics – Consultant. Index Pharma – Consultant. Intercept – Consultant. JAKAcademy – Consultant. Janssen – Advisory Committee/Board Member, Consultant, honoraria; expert testimony. Japan Tobacco Inc. – Consultant. Kaleido Biosciences – Consultant. Klick Health – Consultant. Landos Biopharma – Consultant. Lenczner Slaght – Consultant. LifeSci Capital – Consultant. Lument AB – Consultant. Mage Biologics – Consultant. Merck – Advisory Committee/Board Member. Mestag – Consultant. Millennium – Consultant. MiroBio – Advisory Committee/Board Member, Consultant. Monte Rosa Therapeutics – Consultant. Morgan Lewis – Consultant. Morphic Therapeutics – Advisory Committee/Board Member, Consultant. Mylan – Consultant. Nexera – Consultant. Nexys Therapeutics – Consultant. Nimbus Therapeutics – Consultant. Odyssey – Consultant. OM Pharma – Consultant. OrbiMed – Consultant. Origo BioPharma – Advisory Committee/Board Member, Consultant. Orphagen – Consultant. Pandion Therapeutics – Consultant. Pendopharm – Consultant. Pfizer – Advisory Committee/Board Member, Consultant, honoraria. Progenity – Consultant. Prometheus Therapeutics and Diagnostics (Merck & Co., Inc., Rahway, NJ, USA) – Consultant. Protagonist – Consultant. PTM Therapeutics – Consultant. Q32 Bio – Consultant. Rebiotix – Consultant. REDX Pharma – Advisory Committee/Board Member, Consultant. Roche – Consultant. Roivant/Televant – Consultant. Sandoz – Consultant. Sanofi – Advisory Committee/Board Member, Consultant. Seres Therapeutics – Consultant. Silverback Therapeutics – Consultant. Sobi – Consultant. Spyre Therapeutics – Consultant. Surrozen Inc. – Consultant. Synedgen – Consultant. Takeda – Advisory Committee/Board Member, Consultant, honoraria. Teva – Advisory Committee/Board Member, Consultant. Thelium – Consultant. Tigenix – Consultant. Tillotts – Consultant. Triastek – Consultant. Ventyx – Consultant.
Florian Rieder: Adiso – Advisory Committee/Board Member, Consultant. Adnovate, Agomab, Allergan, AbbVie, Arena, Astra Zeneca, Bausch & Lomb, Boehringer-Ingelheim, Celgene/BMS, Celltrion, CDISC, Celsius, Cowen, 89Bio – Advisory Committee/Board Member, Consultant. Eugit, Ferring, Galapagos, Galmed, Genentech, Gilead, Gossamer, Granite, Guidepoint, Helmsley, Horizon Therapeutics, Image Analysis Limited – Advisory Committee/Board Member, Consultant. Landos, Jannsen, Koutif, Mestag, Metacrine, Mirum, Mobius, Mopac, Morphic, Myka Labs, Organovo, Origo, Palisade, Pfizer, Pliant, Prometheus Bioscience – Advisory Committee/Board Member, Consultant. Receptos, RedX, Roche, Samsung, Sanofi, Surmodics, Surrozen, Takeda, Techlab, Teva, Theravance, Thetis, Tr1x Bio, UCB, Ysios – Advisory Committee/Board Member, Consultant.
Katherine Falloon, MD1, Suha Abushamma, MD1, Ashwin Ananthakrishnan, 2, Edward L. Barnes, MD, MPH3, Abhik Bhattacharya, MD4, Raymond K. Cross, MD, MS, FACG5, Shashank Cheemalavagu, MD1, Jean-Frederic Colombel, MD4, Emily Gore, MD4, Hans Herfarth, MD, PhD6, Sara Horst, MD, MPH, FACG7, M. Elaine Husni, MD1, Jeremy A.. Klein, MD8, Dana J. Lukin, MD, PhD, FACG9, David T. Rubin, MD10, Ellen J. Scherl, MD9, Taha Qazi, MD1, Qijun Yang, MS11, Benjamin L. Cohen, MD1, Brian G. Feagan, MD12, Florian Rieder, MD1. P1047 - Pattern of Joint Distribution in Peripheral Arthritis Does Not Alter Health-Related Quality of Life Across Multiple Patient-Reported Outcomes – Results From the CHASE Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2Division of Gastroenterology, Massachusetts General Hospital and Harvard Medical School, Boston, MA; 3Multidisciplinary Inflammatory Bowel Diseases Center, Division of Gastroenterology and Hepatology, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA, Chapel Hill, NC; 4Icahn School of Medicine at Mount Sinai, New York, NY; 5The Melissa L. Posner Institute for Digestive Health & Liver Disease, Mercy Medical Center, Baltimore, MD; 6University of North Carolina at Chapel Hill, Chapel Hill, NC, USA, Chapel Hill, NC; 7Vanderbilt University School of Medicine, Nashville, TN; 8University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL; 9Jill Roberts Center for Inflammatory Bowel Disease, Weill Cornell Medicine, New York, NY; 10University of Chicago Medicine Inflammatory Bowel Disease Center, Chicago, IL, USA, Chicago, IL; 11Cleveland Clinic, Cleveland, OH; 12Division of Gastroenterology, Department of Medicine, University of Western Ontario and Alimentiv, London, ON, Canada
Introduction: Inflammatory bowel disease (IBD)-associated peripheral spondylarthritis (IBD-pSpA) is common but not well studied, with limited research regarding impact on health-related quality of life (HRQoL). The type I vs type II classification schema, which groups patient based on the distribution, number and size of involved joints, is commonly utilized in the gastroenterology literature. However, this schema is neither widely accepted within the rheumatology literature nor prospectively validated. The aim of this study was to evaluate whether the HRQoL scores vary based on the type I vs type II classification schema.
Methods: We prospectively recruited patients with IBD-pSpA, defined by previously established consensus criteria via the Cohort for Healing Arthritis, Skin, and Eye Extra-Intestinal Manifestations (CHASE-EIM) from six sites across the United States. The relationship of clinical presentation of IBD-pSpA (number and type of involved peripheral joints) on HRQoL was assessed via three previously validated patient reported outcomes – the Inflammatory Bowel Disease Questionnaire (IBDQ), the Work Productivity and Activity Impairment Questionnaire (WPAI), and the Functional Assessment of Chronic Illness Therapy – Fatigue (FACIT-F). Analyses were performed using R software and a significance level of 0.05 was assumed for all tests.
Results: 134 patients with IBD-pSpA (61.2% female, 70.1% with CD) were included in the analysis (Table 1). 47.3% of patients had < 5 joints involved and the remainder ≥5. Hands (65.7%) and knees (58.2%) were the most commonly involved joints. 103 patients completed the requested questionnaires (76.9%). There were no statistically significant differences in any of the questionnaire scores based on number of swollen or tender joints or location of swollen or tender joints (Table 2, data for hands and knees reported; data for other joints not shown but no statistically significant differences identified).
Discussion: Pattern of joint involvement did not influence HRQoL across multiple previously validated PROs (IBDQ, WPAI, and FACIT-F) in patients with IBD-pSpA, casting additional doubt regarding the clinical utility of the type I vs type II classification schema in this patient population. Development of a novel PRO specific to IBD-pSpA will provide further insights into the clinical impact of IBD-pSpA and is currently underway by our group.
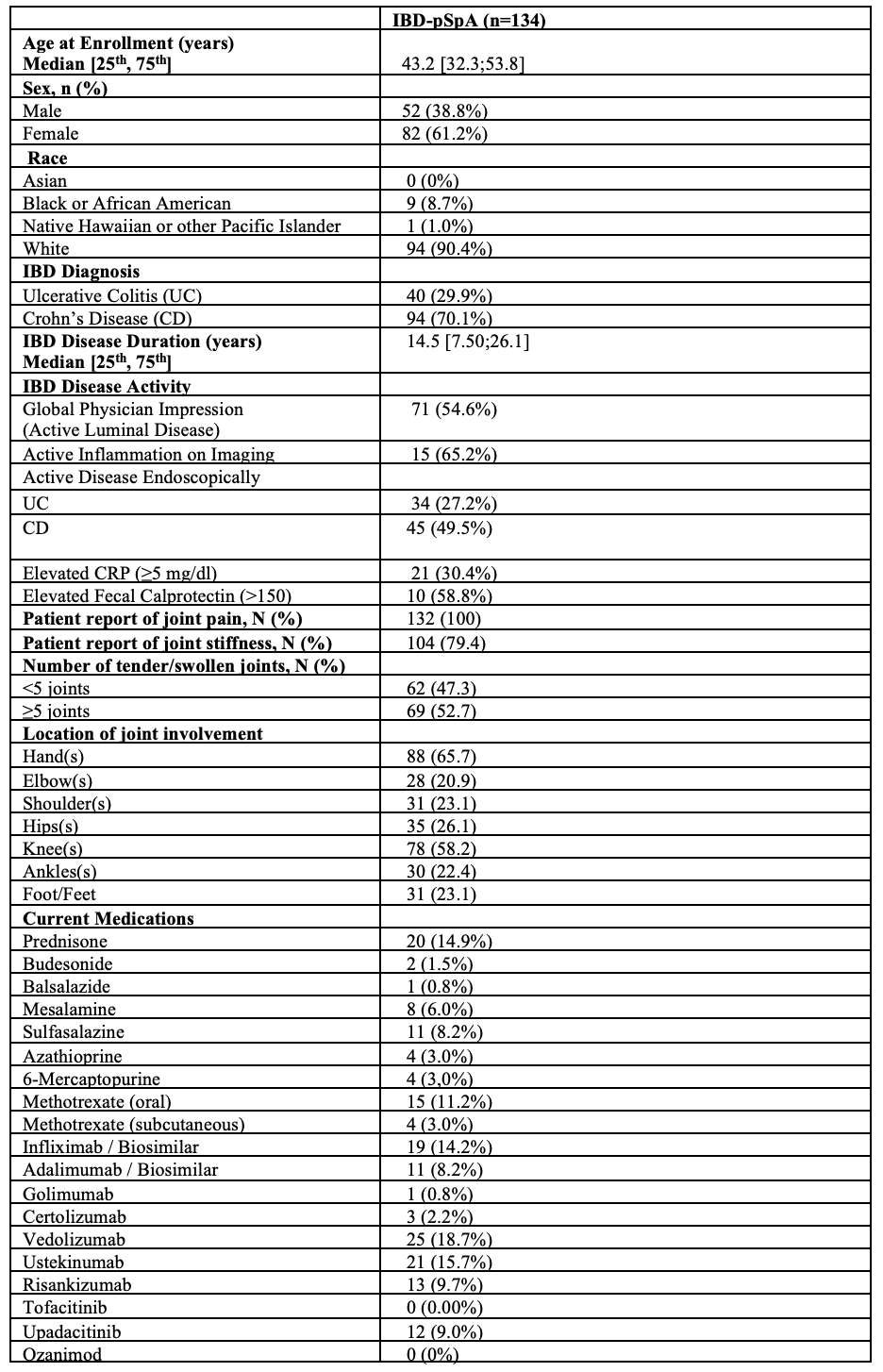
Figure:
Table 1: Baseline Demographics and Clinical Characteristics
IBD-pSpA = inflammatory bowel disease associated peripheral spondyloarthritis, CRP = C reactive protein
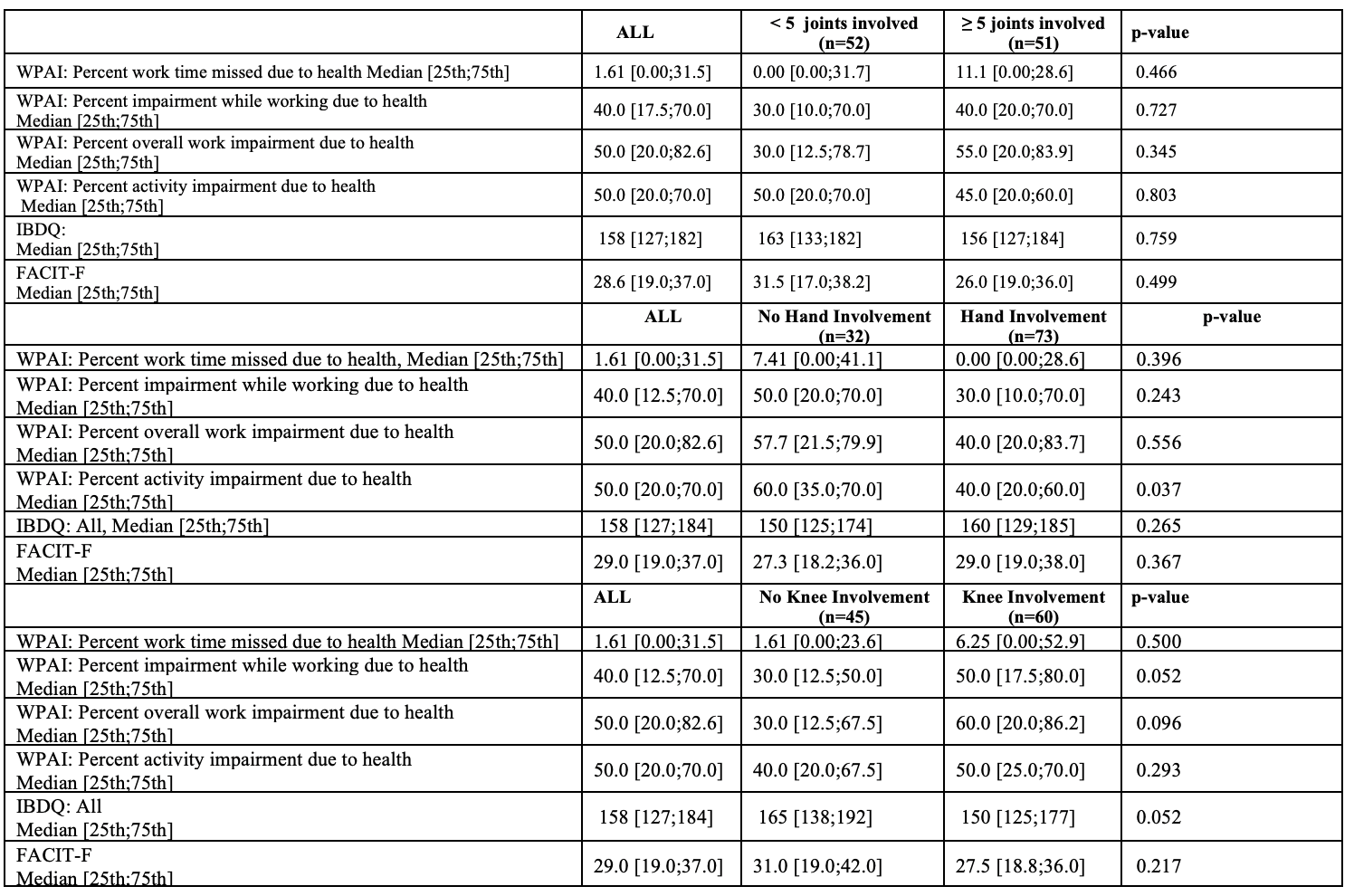
Figure: Table 2: Questionnaire Scores Based on Pattern of Joint Involvement
WPAI = work productivity and activity impairment questionnaire, IBDQ = inflammatory bowel disease questionnaire, FACIT=F = functional assessment of chronic illness therapy
Disclosures:
Katherine Falloon: Cardinal Health, Inc. – Husband is employee. Janssen Pharmaceuticals, Inc. – Consultant. MD Education – Speaker. Pfizer – Grant/Research Support. Takeda Pharmaceuticals, Inc. – Speaker.
Suha Abushamma indicated no relevant financial relationships.
Ashwin Ananthakrishnan: Takeda – Grant/Research Support.
Edward Barnes: AbbVie, Inc. – Consultant. Boomerang – Consultant. Eli Lilly – Consultant. Eli Lilly – Grant/Research Support. Pfizer – Consultant. Sanofi – Consultant. Takeda – Consultant. Target RWE – Consultant.
Abhik Bhattacharya indicated no relevant financial relationships.
Raymond K. Cross: Abbvie – Advisor or Review Panel Member, Consultant, Speakers Bureau. BMS – Advisor or Review Panel Member, Consultant, Speakers Bureau. CorEvitas – Advisory Committee/Board Member. Fresenius Kabi – Advisory Committee/Board Member, Consultant. Genetech – Advisory Committee/Board Member, Consultant. Gilead – Advisory Committee/Board Member, Consultant. IBD Education Group – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Magellan Health – Advisory Committee/Board Member, Consultant. Option Care – Advisory Committee/Board Member, Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Speakers Bureau. Pharmacosmos – Advisory Committee/Board Member, Consultant. Samsung Bioepis – Advisory Committee/Board Member, Consultant. Sandoz – Advisory Committee/Board Member, Consultant. Takeda – Grant/Research Support.
Shashank Cheemalavagu indicated no relevant financial relationships.
Jean-Frederic Colombel: AbbVie – Grant/Research Support, Personal fees. Amgen – Personal fees. Boehringer Ingelheim – Personal fees. Celgene – Personal fees. Celltrion – Personal fees. Enterome – Personal fees. Ferring – Personal fees. Genentech – Personal fees. Genfit – Stock Options. Intestinal Biotech Development – Stock Options. Janssen – Grant/Research Support, Personal fees. MedImmune – Consultant, Personal fees. Merck – Personal fees. Pfizer – Personal fees. PPM Services – Personal fees. Protagonist – Personal fees. Second Genome – Personal fees. Seres – Personal fees. Shire – Personal fees. Takeda – Grant/Research Support, Personal fees. Theradiag – Personal fees.
Emily Gore indicated no relevant financial relationships.
Hans Herfarth: Celltrion – Consultant. ExeGi – Consultant. Gilead – Consultant. Janssen – Consultant. Lilly – Grant/Research Support. Novo Nordisk – Grant/Research Support.
Sara Horst: Abbvie – Consultant. Biocon – Consultant. Celltrion – Consultant. J&J – Consultant. Pfizer – Consultant. Takeda – Consultant.
M. Elaine Husni: Abbvie – Consultant. BMS – Consultant. Eli Lilly – Consultant. Janssen Pharmaceuticals, Inc. – Consultant. Novartis – Consultant. PASE Questionnaire, Co-Inventor – Royalties. UCB – Consultant.
Jeremy Klein indicated no relevant financial relationships.
Dana Lukin: AbbVie – Consultant, Grant/Research Support, Speakers Bureau. Altrubio – Consultant. Boehringer Ingelheim – Consultant, Grant/Research Support. Bristol Myers Squibb – Consultant. Johnson & Johnson – Consultant, Grant/Research Support, Speakers Bureau. Palatin Technologies – Consultant. Pfizer – Consultant. Prime – Consultant. PSI – Consultant. Takeda – Consultant. Vedanta – Consultant.
David Rubin: AbbVie – Advisory Committee/Board Member, Consultant, Speaker fees. Abivax SA – Consultant. Altrubio – Advisory Committee/Board Member, Consultant, Speaker feees, Stock Options. Avalo – Advisory Committee/Board Member, Consultant, Speaker fees. Bausch Health – Consultant. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant, Speaker fees. Buhlmann Diagnostics – Advisory Committee/Board Member, Consultant, Speaker fees. Celltrion – Consultant. ClostraBio – Consultant. Connect BioPharma – Consultant. Cornerstones Health, Inc – Board of Directors membership. Douglas Pharmaceuticals – Consultant. Eli Lilly & Co. – Consultant. Foresee, Genentech (Roche) Inc. – Consultant. Image Analysis Group – Consultant. InDex Pharmaceutical – Consultant. Intouch Group – Advisory Committee/Board Member, Consultant, Speaker fees. Iterative Health – Advisory Committee/Board Member, Consultant, Speaker fees. Iterative Health – Stock Options. Janssen Pharmaceuticals – Consultant. Lilly – Advisory Committee/Board Member, Consultant, Speaker fees. Odyssey Therapeutics – Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Speaker fees. Sanofi – Consultant. Takeda – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speaker fees. Throne – Consultant. Vedanta – Consultant.
Ellen Scherl indicated no relevant financial relationships.
Taha Qazi: Abbvie – Advisor or Review Panel Member, Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Celltirion – Grant/Research Support. Eli Lilly – Advisor or Review Panel Member, Advisory Committee/Board Member, Consultant. Johnson and Johnson – Advisor or Review Panel Member, Advisory Committee/Board Member, Consultant, Speakers Bureau. pfizer – Grant/Research Support.
Qijun Yang indicated no relevant financial relationships.
Benjamin Cohen: Abbvie – Advisory Committee/Board Member, Consultant, Speakers Bureau. ALPCO – Advisory Committee/Board Member, Consultant. Emmes Biopharma Services LLC – DSMB. J&J Innovative Medicine – Advisory Committee/Board Member. Pfizer – Advisory Committee/Board Member. Takeda – Consultant, Speakers Bureau.
Brian G. Feagan: Abbvie – Advisory Committee/Board Member, Consultant, honoraria. Abivax – Consultant. Adiso – Consultant. AgomAb Therapeutics – Consultant. Allianthera – Consultant. Amgen – Consultant. AnaptysBio – Advisory Committee/Board Member, Consultant. Arena Pharma – Consultant. Atomwise – Consultant. Avoro Capital Advisors – Consultant. BioJamp – Consultant. Biora Therapeutics – Consultant. Blackbird Laboratories – Consultant. Boehringer Ingelheim – Advisory Committee/Board Member, Consultant. Boxer Capital – Consultant. Celgene/BMS – Advisory Committee/Board Member, Consultant. Connect BioPharma – Consultant, Stock-publicly held company(excluding mutual/index funds). Cytoki – Consultant. Disc Medicine – Consultant. Duality – Consultant. EcoR1Capital – Advisory Committee/Board Member, Consultant. Eli Lilly – Advisory Committee/Board Member, Consultant. EnGene – Stock-publicly held company(excluding mutual/index funds). Equillium – Consultant. Ermium – Consultant. Evida – Stock-privately held company. First Wave – Consultant. Forbion – Consultant. Galapagos – Consultant. Galen Atlantica – Consultant. Genentech/Roche – Advisory Committee/Board Member, Consultant. Gilead – Consultant. GlaxoSmithKline – Advisory Committee/Board Member, Consultant. Gossamer Pharma – Consultant. Hinge Bio – Consultant. Imhotex – Consultant. Immunic Therapeutics – Consultant. Index Pharma – Consultant. Intercept – Consultant. JAKAcademy – Consultant. Janssen – Advisory Committee/Board Member, Consultant, honoraria; expert testimony. Japan Tobacco Inc. – Consultant. Kaleido Biosciences – Consultant. Klick Health – Consultant. Landos Biopharma – Consultant. Lenczner Slaght – Consultant. LifeSci Capital – Consultant. Lument AB – Consultant. Mage Biologics – Consultant. Merck – Advisory Committee/Board Member. Mestag – Consultant. Millennium – Consultant. MiroBio – Advisory Committee/Board Member, Consultant. Monte Rosa Therapeutics – Consultant. Morgan Lewis – Consultant. Morphic Therapeutics – Advisory Committee/Board Member, Consultant. Mylan – Consultant. Nexera – Consultant. Nexys Therapeutics – Consultant. Nimbus Therapeutics – Consultant. Odyssey – Consultant. OM Pharma – Consultant. OrbiMed – Consultant. Origo BioPharma – Advisory Committee/Board Member, Consultant. Orphagen – Consultant. Pandion Therapeutics – Consultant. Pendopharm – Consultant. Pfizer – Advisory Committee/Board Member, Consultant, honoraria. Progenity – Consultant. Prometheus Therapeutics and Diagnostics (Merck & Co., Inc., Rahway, NJ, USA) – Consultant. Protagonist – Consultant. PTM Therapeutics – Consultant. Q32 Bio – Consultant. Rebiotix – Consultant. REDX Pharma – Advisory Committee/Board Member, Consultant. Roche – Consultant. Roivant/Televant – Consultant. Sandoz – Consultant. Sanofi – Advisory Committee/Board Member, Consultant. Seres Therapeutics – Consultant. Silverback Therapeutics – Consultant. Sobi – Consultant. Spyre Therapeutics – Consultant. Surrozen Inc. – Consultant. Synedgen – Consultant. Takeda – Advisory Committee/Board Member, Consultant, honoraria. Teva – Advisory Committee/Board Member, Consultant. Thelium – Consultant. Tigenix – Consultant. Tillotts – Consultant. Triastek – Consultant. Ventyx – Consultant.
Florian Rieder: Adiso – Advisory Committee/Board Member, Consultant. Adnovate, Agomab, Allergan, AbbVie, Arena, Astra Zeneca, Bausch & Lomb, Boehringer-Ingelheim, Celgene/BMS, Celltrion, CDISC, Celsius, Cowen, 89Bio – Advisory Committee/Board Member, Consultant. Eugit, Ferring, Galapagos, Galmed, Genentech, Gilead, Gossamer, Granite, Guidepoint, Helmsley, Horizon Therapeutics, Image Analysis Limited – Advisory Committee/Board Member, Consultant. Landos, Jannsen, Koutif, Mestag, Metacrine, Mirum, Mobius, Mopac, Morphic, Myka Labs, Organovo, Origo, Palisade, Pfizer, Pliant, Prometheus Bioscience – Advisory Committee/Board Member, Consultant. Receptos, RedX, Roche, Samsung, Sanofi, Surmodics, Surrozen, Takeda, Techlab, Teva, Theravance, Thetis, Tr1x Bio, UCB, Ysios – Advisory Committee/Board Member, Consultant.
Katherine Falloon, MD1, Suha Abushamma, MD1, Ashwin Ananthakrishnan, 2, Edward L. Barnes, MD, MPH3, Abhik Bhattacharya, MD4, Raymond K. Cross, MD, MS, FACG5, Shashank Cheemalavagu, MD1, Jean-Frederic Colombel, MD4, Emily Gore, MD4, Hans Herfarth, MD, PhD6, Sara Horst, MD, MPH, FACG7, M. Elaine Husni, MD1, Jeremy A.. Klein, MD8, Dana J. Lukin, MD, PhD, FACG9, David T. Rubin, MD10, Ellen J. Scherl, MD9, Taha Qazi, MD1, Qijun Yang, MS11, Benjamin L. Cohen, MD1, Brian G. Feagan, MD12, Florian Rieder, MD1. P1047 - Pattern of Joint Distribution in Peripheral Arthritis Does Not Alter Health-Related Quality of Life Across Multiple Patient-Reported Outcomes – Results From the CHASE Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
