Sunday Poster Session
Category: IBD
P1097 - Post-Hospitalization Outcomes in Inflammatory Bowel Disease: Insights from a Diverse Urban Academic Center
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Caleb Glover, DO (he/him/his)
McLaren Greater Lansing Hospital
Lansing, MI
Presenting Author(s)
Caleb Glover, DO1, Fnu Rashi, MD2, Agustin Gavidia Rosario, MD2, Muneer Hasso, MD2, Ali Kadouh, MD2, Jamie Roberman, PhD2, Najwa El-Nachef, MD2
1McLaren Greater Lansing Hospital, Lansing, MI; 2Henry Ford Health, Detroit, MI
Introduction: Patients from low socioeconomic and/or racially diverse backgrounds are known to experience worse outcomes in inflammatory bowel disease (IBD) yet post-discharge outcomes after IBD flares in these groups remain poorly defined. Hospital admissions for IBD flares offer a critical opportunity to reconnect patients with sub-specialty care, making this a key period for potential intervention. We aimed to characterize the post-discharge outcomes for IBD patients admitted to a large, urban academic center that predominantly cares for an underserved population to help identify potential interventions to improve IBD outcomes.
Methods: We retrospectively identified consecutive adult admissions at a single center for Crohn’s disease (CD) or ulcerative colitis (UC) between September 1, 2022, and August 30, 2024. Demographics, IBD therapies, and laboratory markers were abstracted. Primary outcomes were completion of a gastroenterology (GI) visit within 90 days of discharge and any unplanned readmission for IBD flare within 12 months. Unadjusted comparisons used Wilcoxon, χ², or Fisher’s exact tests, and logistic regression assessed predictors of 12-month readmission after adjustment for age, sex, race, smoking status, and IBD subtype.
Results: 81 patients met inclusion criteria (median age 42 years; 47% women; 35% Black, 49% White). Median length of stay was 5 days; 54% had CD; 20% were current smokers; 35% initiated a biologic within one month of discharge. 45% (37/81) did not follow up in GI clinic within 90 days. Follow-up differed by race, occurring in 62% White v 50% of Black patients (p = 0.012). Among 79 patients with at least 12 months of observation, 41% (32/79) were readmitted, accounting for 82 readmissions over 928 patient-months. In multivariable analysis, former smoking was associated with lower odds of readmission compared with current smoking (adjusted odds ratio 0.20, 95 % CI 0.04–0.91; p = 0.044), whereas age, sex, race, and IBD subtype were not significant.
Discussion: Nearly half of IBD inpatients were lost to timely post-discharge follow-up, 2 in 5 were readmitted within a year. The observed racial disparity in timely subspecialty follow-up and the strong link between ongoing smoking and readmission highlight modifiable targets. Transition-of-care pathways that prioritize rapid clinic scheduling, smoking cessation, and proactive outreach may represent interventions to improve IBD outcomes and advance health equity in this vulnerable patient population.
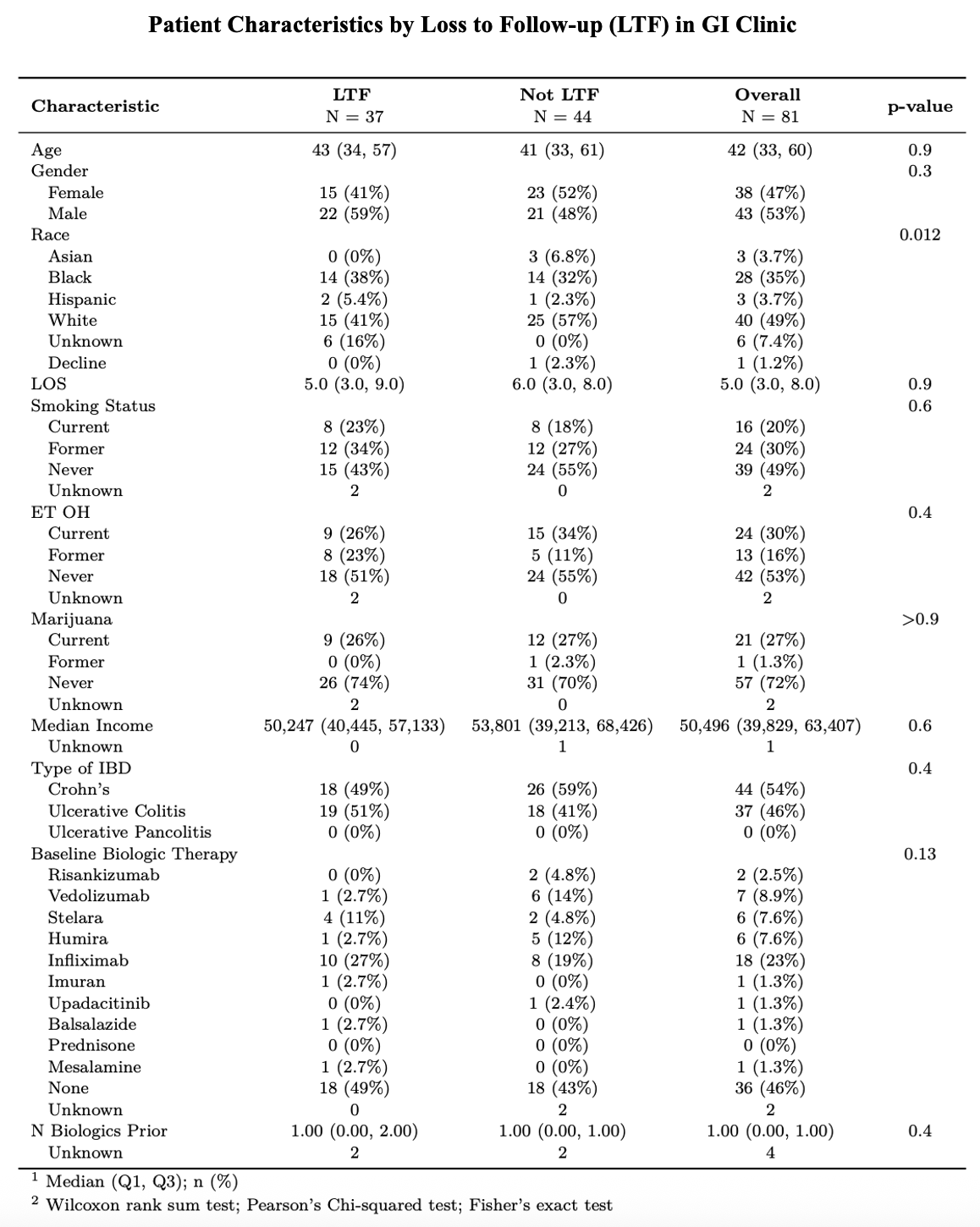
Figure: Patient characteristics by GI clinic follow-up within 90 days.
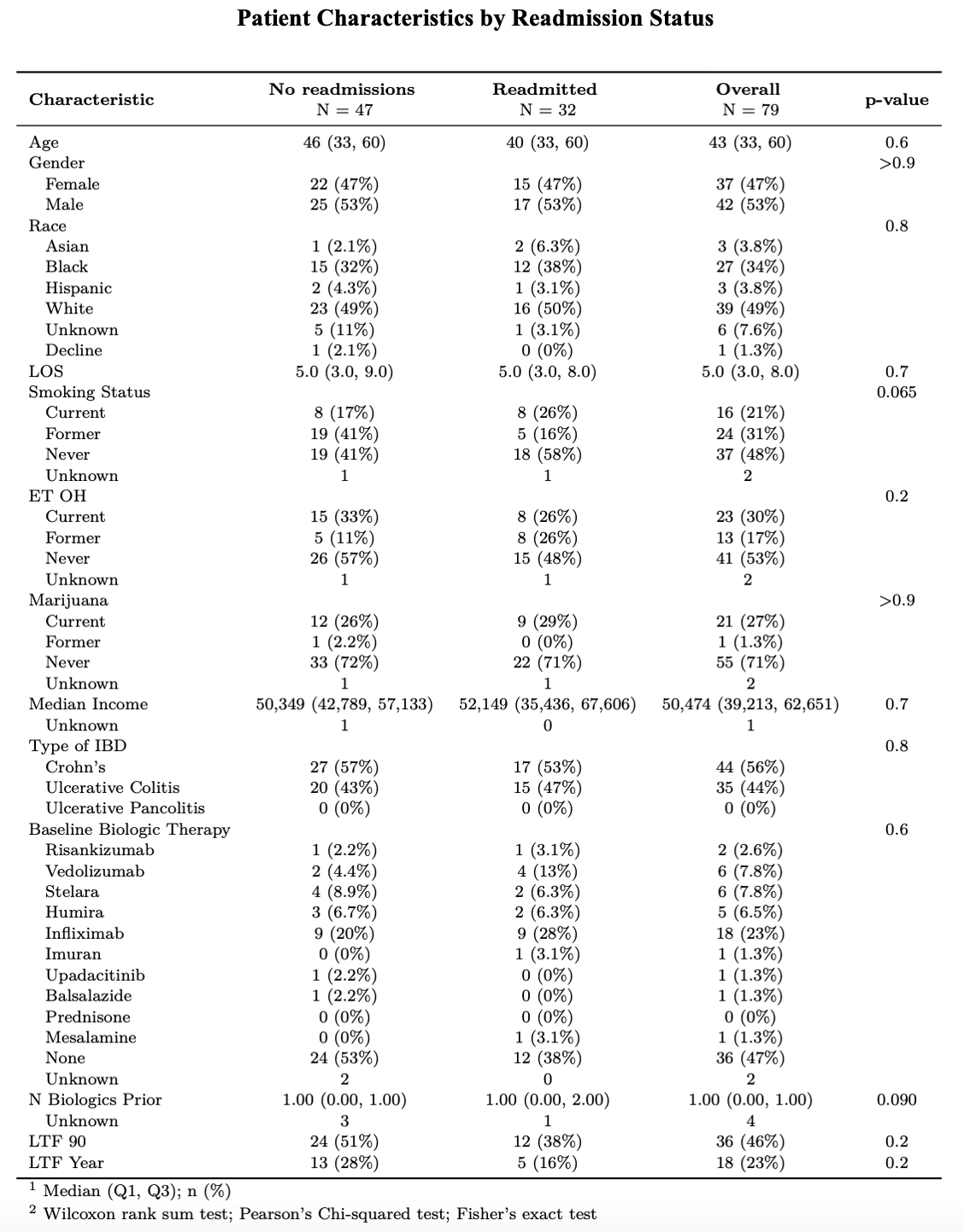
Figure: Patient characteristics by whether the patient was readmitted within a year of discharge.
Disclosures:
Caleb Glover indicated no relevant financial relationships.
Fnu Rashi indicated no relevant financial relationships.
Agustin Gavidia Rosario indicated no relevant financial relationships.
Muneer Hasso indicated no relevant financial relationships.
Ali Kadouh indicated no relevant financial relationships.
Jamie Roberman indicated no relevant financial relationships.
Najwa El-Nachef: Abbvie – Grant/Research Support. Abivax – Grant/Research Support. Genentech – Grant/Research Support. Takeda – Grant/Research Support.
Caleb Glover, DO1, Fnu Rashi, MD2, Agustin Gavidia Rosario, MD2, Muneer Hasso, MD2, Ali Kadouh, MD2, Jamie Roberman, PhD2, Najwa El-Nachef, MD2. P1097 - Post-Hospitalization Outcomes in Inflammatory Bowel Disease: Insights from a Diverse Urban Academic Center, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1McLaren Greater Lansing Hospital, Lansing, MI; 2Henry Ford Health, Detroit, MI
Introduction: Patients from low socioeconomic and/or racially diverse backgrounds are known to experience worse outcomes in inflammatory bowel disease (IBD) yet post-discharge outcomes after IBD flares in these groups remain poorly defined. Hospital admissions for IBD flares offer a critical opportunity to reconnect patients with sub-specialty care, making this a key period for potential intervention. We aimed to characterize the post-discharge outcomes for IBD patients admitted to a large, urban academic center that predominantly cares for an underserved population to help identify potential interventions to improve IBD outcomes.
Methods: We retrospectively identified consecutive adult admissions at a single center for Crohn’s disease (CD) or ulcerative colitis (UC) between September 1, 2022, and August 30, 2024. Demographics, IBD therapies, and laboratory markers were abstracted. Primary outcomes were completion of a gastroenterology (GI) visit within 90 days of discharge and any unplanned readmission for IBD flare within 12 months. Unadjusted comparisons used Wilcoxon, χ², or Fisher’s exact tests, and logistic regression assessed predictors of 12-month readmission after adjustment for age, sex, race, smoking status, and IBD subtype.
Results: 81 patients met inclusion criteria (median age 42 years; 47% women; 35% Black, 49% White). Median length of stay was 5 days; 54% had CD; 20% were current smokers; 35% initiated a biologic within one month of discharge. 45% (37/81) did not follow up in GI clinic within 90 days. Follow-up differed by race, occurring in 62% White v 50% of Black patients (p = 0.012). Among 79 patients with at least 12 months of observation, 41% (32/79) were readmitted, accounting for 82 readmissions over 928 patient-months. In multivariable analysis, former smoking was associated with lower odds of readmission compared with current smoking (adjusted odds ratio 0.20, 95 % CI 0.04–0.91; p = 0.044), whereas age, sex, race, and IBD subtype were not significant.
Discussion: Nearly half of IBD inpatients were lost to timely post-discharge follow-up, 2 in 5 were readmitted within a year. The observed racial disparity in timely subspecialty follow-up and the strong link between ongoing smoking and readmission highlight modifiable targets. Transition-of-care pathways that prioritize rapid clinic scheduling, smoking cessation, and proactive outreach may represent interventions to improve IBD outcomes and advance health equity in this vulnerable patient population.
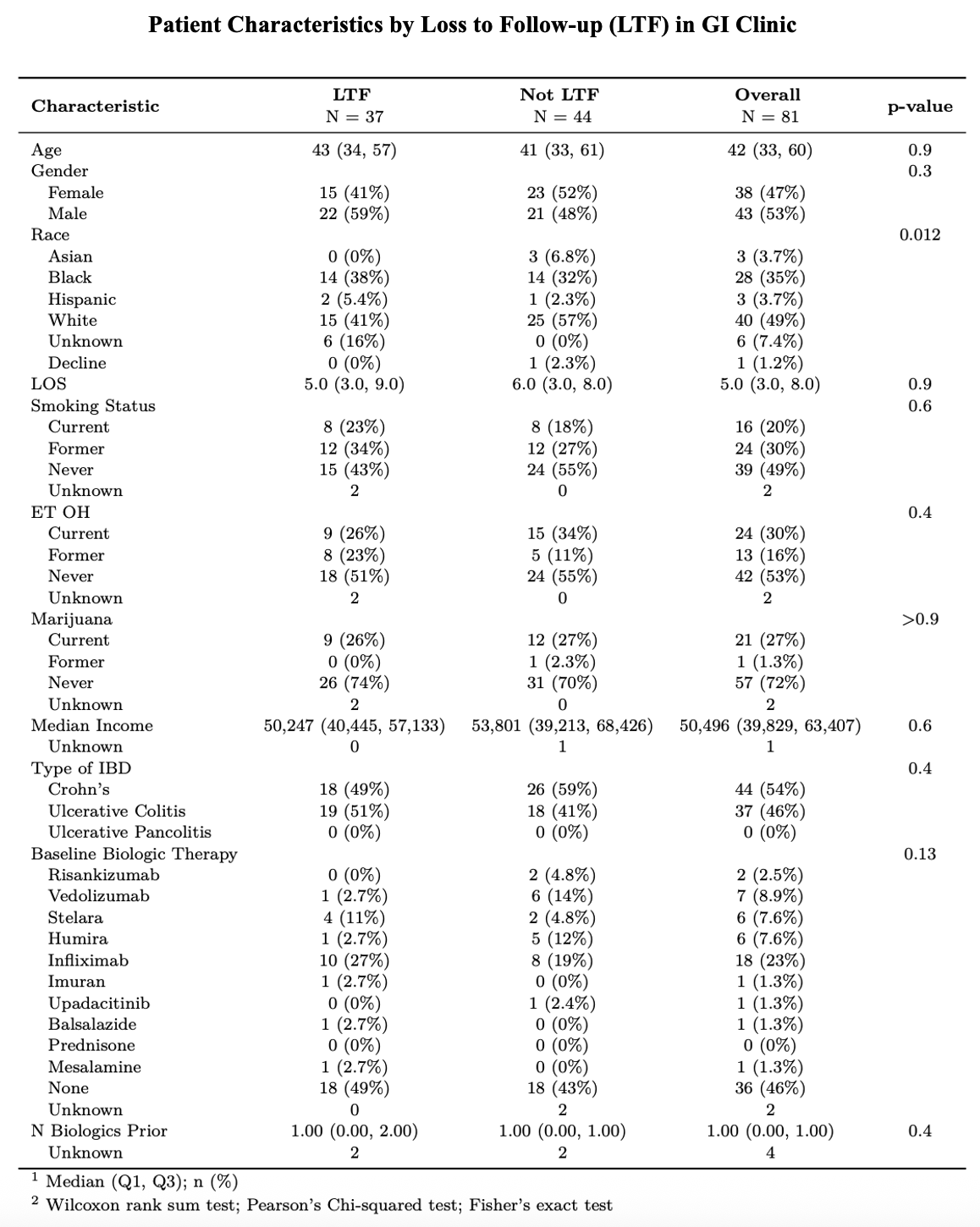
Figure: Patient characteristics by GI clinic follow-up within 90 days.
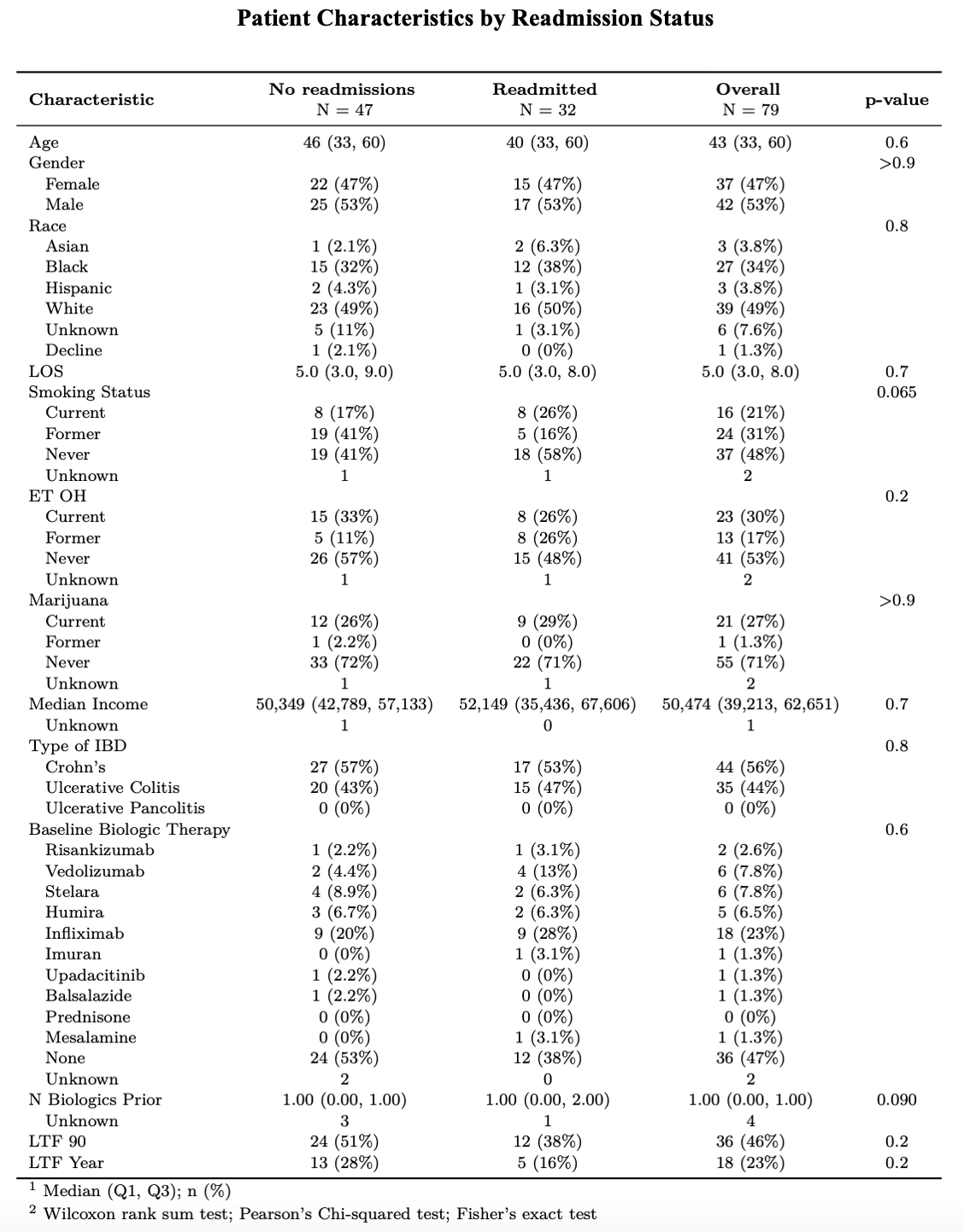
Figure: Patient characteristics by whether the patient was readmitted within a year of discharge.
Disclosures:
Caleb Glover indicated no relevant financial relationships.
Fnu Rashi indicated no relevant financial relationships.
Agustin Gavidia Rosario indicated no relevant financial relationships.
Muneer Hasso indicated no relevant financial relationships.
Ali Kadouh indicated no relevant financial relationships.
Jamie Roberman indicated no relevant financial relationships.
Najwa El-Nachef: Abbvie – Grant/Research Support. Abivax – Grant/Research Support. Genentech – Grant/Research Support. Takeda – Grant/Research Support.
Caleb Glover, DO1, Fnu Rashi, MD2, Agustin Gavidia Rosario, MD2, Muneer Hasso, MD2, Ali Kadouh, MD2, Jamie Roberman, PhD2, Najwa El-Nachef, MD2. P1097 - Post-Hospitalization Outcomes in Inflammatory Bowel Disease: Insights from a Diverse Urban Academic Center, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
