Sunday Poster Session
Category: IBD
P1180 - Unraveling the Significance of Cecal Patch/Periappendiceal Involvement in Ulcerative Colitis: A Systematic Review and Meta-Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Ryan Nazari, BS (he/him/his)
Kansas City University, OK
Presenting Author(s)
Shahryar Khan, MD1, Ryan Nazari, BS2, Manav Nayeni, BMSc2, Sanket Basida, MD3, Olivia Price, MS4, Tuba Esfandyari, MD, FACG4
1University of Kansas Medical Center, Kansas City, KS; 2Kansas City University, Kansas City, MO; 3University of Missouri Health Care, Columbia, MO; 4The University of Kansas Health System, Kansas City, KS
Introduction: The presence of the cecal patch/periappendiceal red patch (PARP) has been observed during colonoscopy in patients with UC; however, its impact on disease characteristics and outcomes remains unclear. This systematic review and meta-analysis aimed to evaluate the clinical significance of PARP involvement in patients with ulcerative colitis (UC).
Methods: A comprehensive search of PubMed and Embase was conducted to identify studies comparing UC patients with UC with and without PARP. Data on the extent of disease, clinical and endoscopic remission, treatment escalation, relapse rates, neoplasia, colectomy, and hospitalization were also extracted. Heterogeneity was assessed using I² statistics. A random-effects model was used to calculate the standardized mean difference (SMD) and odds ratio (OR), with statistical significance defined as p < 0.05.
Results: Thirteen full-text articles were identified, encompassing a total study population of 2,922 participants, with 791 (27.1%) patients presenting PARP involvement. The pooled analysis revealed a relatively high prevalence of PARP in UC patients (20.62%; 95% CI 11.38%-31.75, Fig 1). The meta-analysis did not find statistically significant differences in the rates of pancolitis (OR 0.97, p = 0.82, I² = 13%), left-sided colitis (OR 0.74, p = 0.12, I² = 60%), or proctitis (OR 0.58, p = 0.10, I² = 0%) at initial diagnosis between the PARP and non-PARP groups. During the mean follow-up period of 50.75 ± 24.6 months, UC patients with PARP involvement demonstrated a persistently higher incidence of proctitis (OR 2.50, I², 71%; p = 0.01), with no significant difference in the progression to left-sided colitis (OR 0.54, I² = 61%, p = 0.06) compared to those without PARP. Furthermore, PARP involvement was associated with a non-significant trend towards an increased overall disease extent (OR 1.97, p = 0.06; I² = 78%, Fig 2) and progression to pancolitis (OR 2.01, p = 0.23; I² = 85%). There were no significant differences in the clinical remission rates, endoscopic remission, treatment escalation, neoplasia, colectomy, or hospitalization between the two groups (Table 1).
Discussion: This review highlights the clinical significance of PARP involvement in UC, linking it to distinct disease characteristics and more challenging outcomes. However, the existing evidence has limited value in informing current clinical management. Further study of PARP's mechanisms and implications of PARP is needed to optimize the treatment.
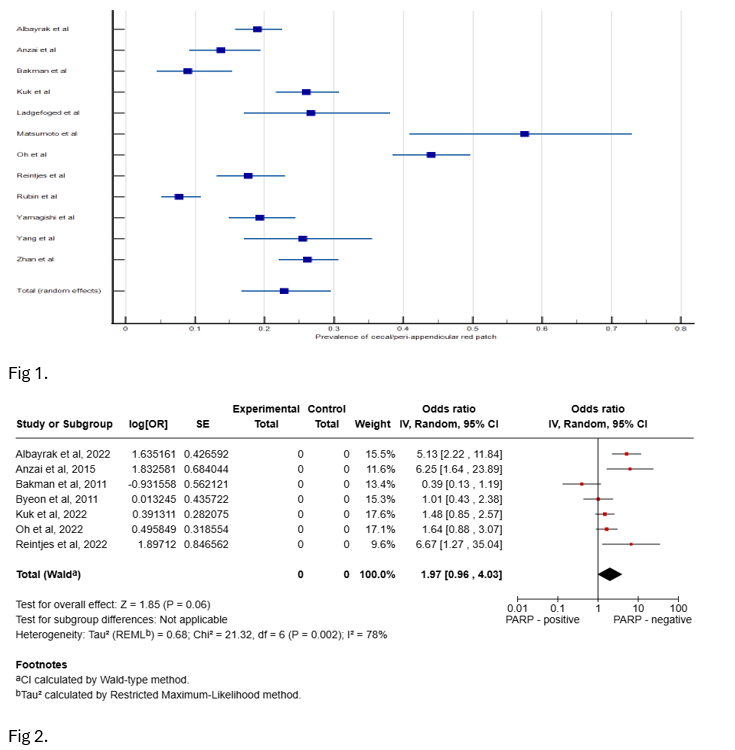
Figure: Fig 1. Pooled Prevalence of Cecal Patch/Periappendiceal Involvement in Ulcerative Colitis; Fig 2. Forest plot comparing overall proximal disease extension between ulcerative colitis patients with and without PARP involvement.
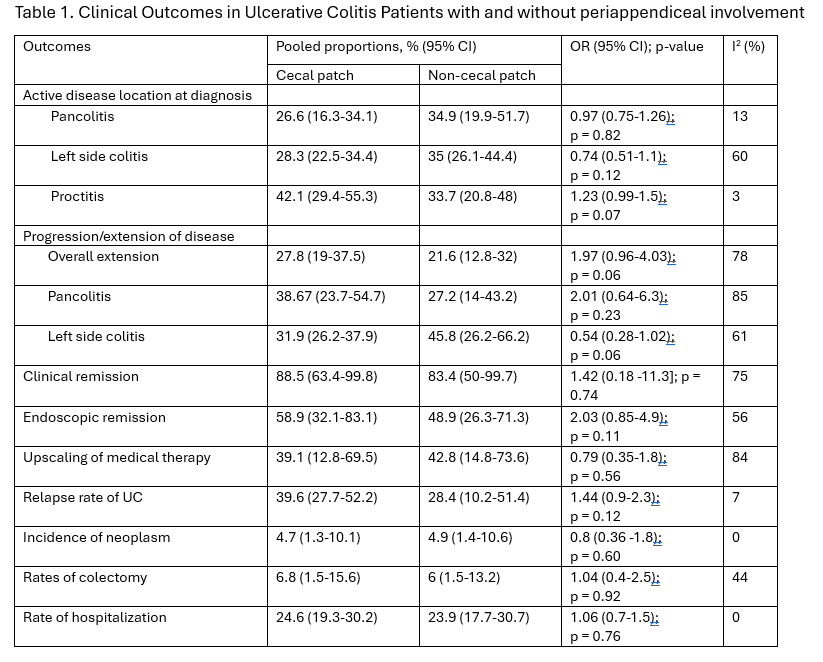
Figure: Table 1. Clinical Outcomes in Ulcerative Colitis Patients with and without periappendiceal involvement
Disclosures:
Shahryar Khan indicated no relevant financial relationships.
Ryan Nazari indicated no relevant financial relationships.
Manav Nayeni indicated no relevant financial relationships.
Sanket Basida indicated no relevant financial relationships.
Olivia Price indicated no relevant financial relationships.
Tuba Esfandyari indicated no relevant financial relationships.
Shahryar Khan, MD1, Ryan Nazari, BS2, Manav Nayeni, BMSc2, Sanket Basida, MD3, Olivia Price, MS4, Tuba Esfandyari, MD, FACG4. P1180 - Unraveling the Significance of Cecal Patch/Periappendiceal Involvement in Ulcerative Colitis: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Kansas Medical Center, Kansas City, KS; 2Kansas City University, Kansas City, MO; 3University of Missouri Health Care, Columbia, MO; 4The University of Kansas Health System, Kansas City, KS
Introduction: The presence of the cecal patch/periappendiceal red patch (PARP) has been observed during colonoscopy in patients with UC; however, its impact on disease characteristics and outcomes remains unclear. This systematic review and meta-analysis aimed to evaluate the clinical significance of PARP involvement in patients with ulcerative colitis (UC).
Methods: A comprehensive search of PubMed and Embase was conducted to identify studies comparing UC patients with UC with and without PARP. Data on the extent of disease, clinical and endoscopic remission, treatment escalation, relapse rates, neoplasia, colectomy, and hospitalization were also extracted. Heterogeneity was assessed using I² statistics. A random-effects model was used to calculate the standardized mean difference (SMD) and odds ratio (OR), with statistical significance defined as p < 0.05.
Results: Thirteen full-text articles were identified, encompassing a total study population of 2,922 participants, with 791 (27.1%) patients presenting PARP involvement. The pooled analysis revealed a relatively high prevalence of PARP in UC patients (20.62%; 95% CI 11.38%-31.75, Fig 1). The meta-analysis did not find statistically significant differences in the rates of pancolitis (OR 0.97, p = 0.82, I² = 13%), left-sided colitis (OR 0.74, p = 0.12, I² = 60%), or proctitis (OR 0.58, p = 0.10, I² = 0%) at initial diagnosis between the PARP and non-PARP groups. During the mean follow-up period of 50.75 ± 24.6 months, UC patients with PARP involvement demonstrated a persistently higher incidence of proctitis (OR 2.50, I², 71%; p = 0.01), with no significant difference in the progression to left-sided colitis (OR 0.54, I² = 61%, p = 0.06) compared to those without PARP. Furthermore, PARP involvement was associated with a non-significant trend towards an increased overall disease extent (OR 1.97, p = 0.06; I² = 78%, Fig 2) and progression to pancolitis (OR 2.01, p = 0.23; I² = 85%). There were no significant differences in the clinical remission rates, endoscopic remission, treatment escalation, neoplasia, colectomy, or hospitalization between the two groups (Table 1).
Discussion: This review highlights the clinical significance of PARP involvement in UC, linking it to distinct disease characteristics and more challenging outcomes. However, the existing evidence has limited value in informing current clinical management. Further study of PARP's mechanisms and implications of PARP is needed to optimize the treatment.
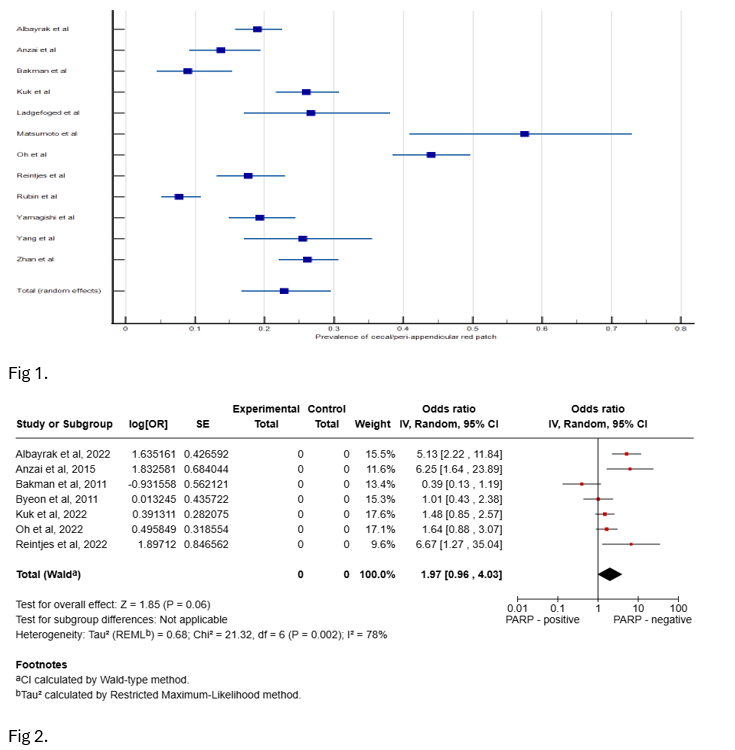
Figure: Fig 1. Pooled Prevalence of Cecal Patch/Periappendiceal Involvement in Ulcerative Colitis; Fig 2. Forest plot comparing overall proximal disease extension between ulcerative colitis patients with and without PARP involvement.
Figure: Table 1. Clinical Outcomes in Ulcerative Colitis Patients with and without periappendiceal involvement
Disclosures:
Shahryar Khan indicated no relevant financial relationships.
Ryan Nazari indicated no relevant financial relationships.
Manav Nayeni indicated no relevant financial relationships.
Sanket Basida indicated no relevant financial relationships.
Olivia Price indicated no relevant financial relationships.
Tuba Esfandyari indicated no relevant financial relationships.
Shahryar Khan, MD1, Ryan Nazari, BS2, Manav Nayeni, BMSc2, Sanket Basida, MD3, Olivia Price, MS4, Tuba Esfandyari, MD, FACG4. P1180 - Unraveling the Significance of Cecal Patch/Periappendiceal Involvement in Ulcerative Colitis: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
