Sunday Poster Session
Category: IBD
P1250 - A Therapeutic Conundrum for a Rare Case of Colonic MALT Lymphoma in Ulcerative Colitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- ZM
Zeel Modi, MD (she/her/hers)
University of Illinois
Chicago, IL
Presenting Author(s)
Award: ACG Presidential Poster Award
Zeel Modi, MD, Mustansir Abbas Ali, MBBS, Maria El Gemayel, MD, Itishree Trivedi, MD
University of Illinois, Chicago, IL
Introduction: Inflammatory bowel diseases (IBD), including Crohn’s disease (CD) and ulcerative colitis (UC), are autoimmune gastrointestinal (GI) conditions linked to higher neoplasia risk. Recent studies suggest a higher colonic lymphoma risk in IBD, but the absolute risk remains low. Mucosal-associated lymphoid tissue lymphoma (MALT-L) is a rare, poorly investigated complication in IBD. Management guidelines for IBD after MALT-L diagnosis are also limited. We present a case of colonic MALT-L in a poorly controlled UC patient, managed with surgery and cessation of advanced therapies.
Case Description/
Methods: A 24-year-old female with refractory UC presented for a second opinion for persistent hematochezia, mucus in stool, and abdominal cramping. Diagnosed five years ago, her UC was recalcitrant to therapies, due to steroid dependence or intolerable side effects. She was on adalimumab. Colonoscopy showed contiguous endoscopy Mayo score 2-type inflammatory changes in the rectum and sigmoid colon (Figure A), with random biopsies noting extranodal B-cell marginal zone lymphoma arising in a background of chronic colitis. PET study reported diffuse rectosigmoid uptake supporting MALT-L diagnosis. After four Rituximab cycles, she had partial symptom improvement, with follow-up sigmoidoscopy noting MALT-L resolution and reduced colonic uptake on repeat PET. Despite lymphoma remission, she had burdensome GI symptoms. She opted for a laparoscopic diverting loop ileostomy and a pause on advanced therapies, which resulted in complete symptom resolution.
Discussion: Non-Hodgkin Lymphoma (NHL) presents extra-nodally in 40% of cases. Half of them are in the GI tract, with the stomach being a predominant site due to H. pylori infection. IBD involves inappropriate mucosal immune activation leading to chronic gut inflammation and complications like neoplasia, with primary intestinal lymphoma being the most common lymphoma type in IBD. Colonic MALT-L is rare and diagnostically challenging. Chronic immune stimulation from persistent inflammation is suspected as the likely etiology, but treatment-related NHL risk complicates management. Though not directly linked with MALT-L, IBD therapies may also increase NHL risk. Standard MALT-L treatments include H. pylori eradication, chemotherapy, and radiotherapy. However, management of non-gastric MALT-L is less well established. This case highlights the need for updated management guidelines in IBD patients with various GI lymphomas, particularly focusing on advanced IBD therapies.
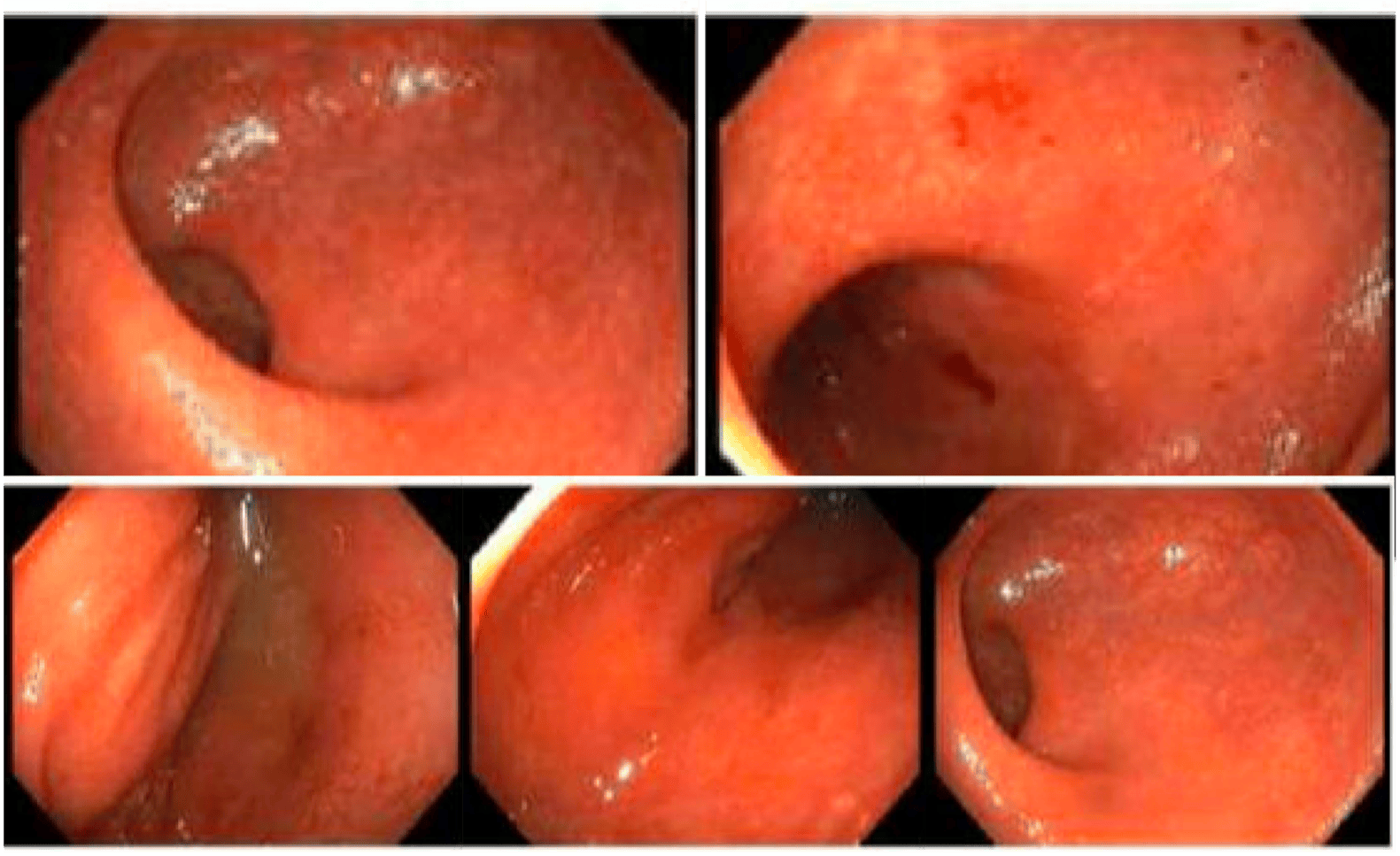
Figure: Figure A: Colonoscopy demonstrating congested, eroded, erythematous, exudative, and friable mucosa without deep ulcerations or raised lesions in the rectosigmoid region, concerning for moderate chronic colitis, and biopsies were taken. The rest of the colon was unremarkable.
Disclosures:
Zeel Modi indicated no relevant financial relationships.
Mustansir Abbas Ali indicated no relevant financial relationships.
Maria El Gemayel indicated no relevant financial relationships.
Itishree Trivedi indicated no relevant financial relationships.
Zeel Modi, MD, Mustansir Abbas Ali, MBBS, Maria El Gemayel, MD, Itishree Trivedi, MD. P1250 - A Therapeutic Conundrum for a Rare Case of Colonic MALT Lymphoma in Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Zeel Modi, MD, Mustansir Abbas Ali, MBBS, Maria El Gemayel, MD, Itishree Trivedi, MD
University of Illinois, Chicago, IL
Introduction: Inflammatory bowel diseases (IBD), including Crohn’s disease (CD) and ulcerative colitis (UC), are autoimmune gastrointestinal (GI) conditions linked to higher neoplasia risk. Recent studies suggest a higher colonic lymphoma risk in IBD, but the absolute risk remains low. Mucosal-associated lymphoid tissue lymphoma (MALT-L) is a rare, poorly investigated complication in IBD. Management guidelines for IBD after MALT-L diagnosis are also limited. We present a case of colonic MALT-L in a poorly controlled UC patient, managed with surgery and cessation of advanced therapies.
Case Description/
Methods: A 24-year-old female with refractory UC presented for a second opinion for persistent hematochezia, mucus in stool, and abdominal cramping. Diagnosed five years ago, her UC was recalcitrant to therapies, due to steroid dependence or intolerable side effects. She was on adalimumab. Colonoscopy showed contiguous endoscopy Mayo score 2-type inflammatory changes in the rectum and sigmoid colon (Figure A), with random biopsies noting extranodal B-cell marginal zone lymphoma arising in a background of chronic colitis. PET study reported diffuse rectosigmoid uptake supporting MALT-L diagnosis. After four Rituximab cycles, she had partial symptom improvement, with follow-up sigmoidoscopy noting MALT-L resolution and reduced colonic uptake on repeat PET. Despite lymphoma remission, she had burdensome GI symptoms. She opted for a laparoscopic diverting loop ileostomy and a pause on advanced therapies, which resulted in complete symptom resolution.
Discussion: Non-Hodgkin Lymphoma (NHL) presents extra-nodally in 40% of cases. Half of them are in the GI tract, with the stomach being a predominant site due to H. pylori infection. IBD involves inappropriate mucosal immune activation leading to chronic gut inflammation and complications like neoplasia, with primary intestinal lymphoma being the most common lymphoma type in IBD. Colonic MALT-L is rare and diagnostically challenging. Chronic immune stimulation from persistent inflammation is suspected as the likely etiology, but treatment-related NHL risk complicates management. Though not directly linked with MALT-L, IBD therapies may also increase NHL risk. Standard MALT-L treatments include H. pylori eradication, chemotherapy, and radiotherapy. However, management of non-gastric MALT-L is less well established. This case highlights the need for updated management guidelines in IBD patients with various GI lymphomas, particularly focusing on advanced IBD therapies.
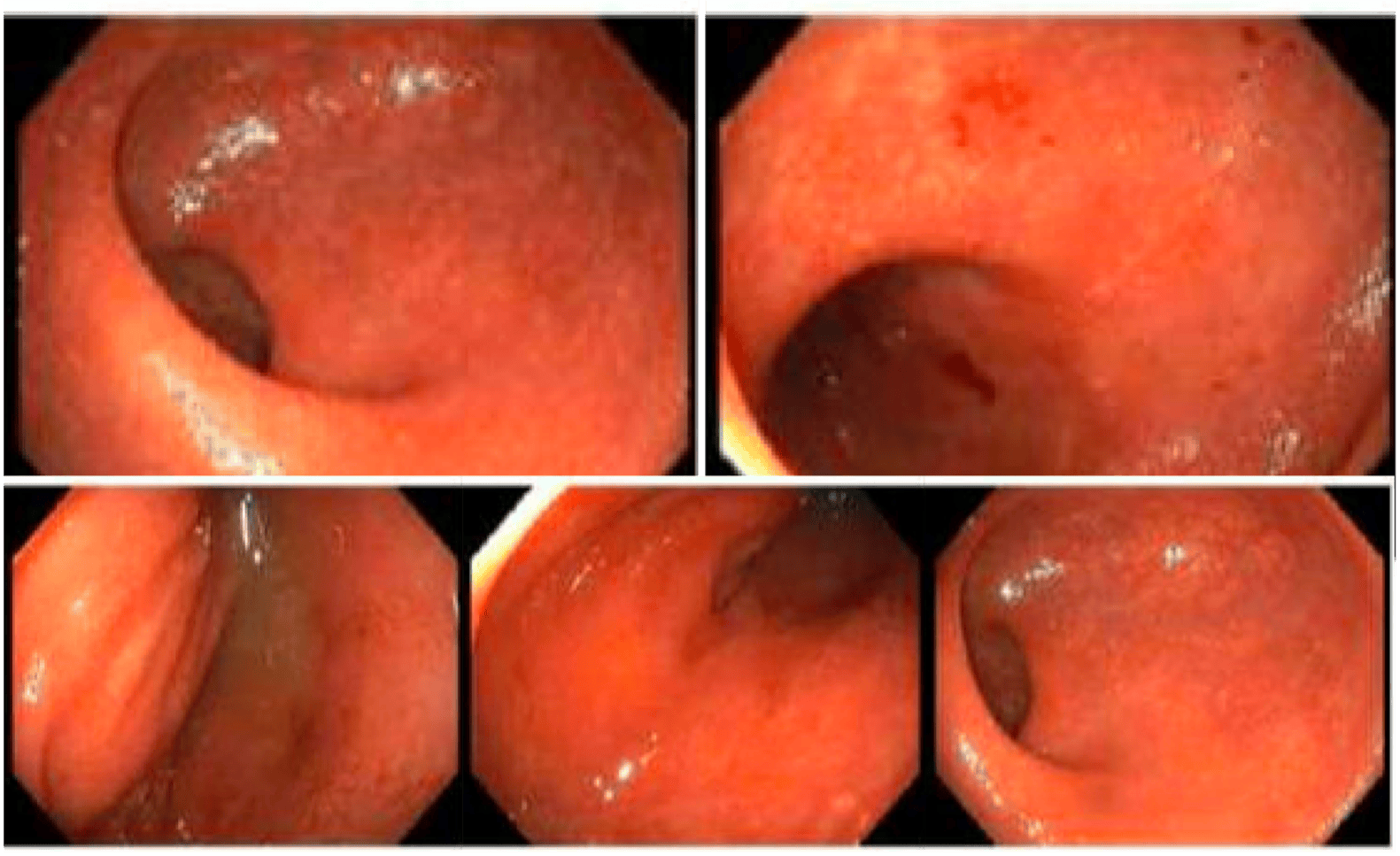
Figure: Figure A: Colonoscopy demonstrating congested, eroded, erythematous, exudative, and friable mucosa without deep ulcerations or raised lesions in the rectosigmoid region, concerning for moderate chronic colitis, and biopsies were taken. The rest of the colon was unremarkable.
Disclosures:
Zeel Modi indicated no relevant financial relationships.
Mustansir Abbas Ali indicated no relevant financial relationships.
Maria El Gemayel indicated no relevant financial relationships.
Itishree Trivedi indicated no relevant financial relationships.
Zeel Modi, MD, Mustansir Abbas Ali, MBBS, Maria El Gemayel, MD, Itishree Trivedi, MD. P1250 - A Therapeutic Conundrum for a Rare Case of Colonic MALT Lymphoma in Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

